Colonic Obstruction Secondary to Chronic Diverticulitis: Case Report and Literature Review
Chidubem Ekpereamaka Okechukwu*, Shawntiah N. Jones, Tobe Momah
University of British Columbia, Vancouver, British Columbia, Canada
Department of Family Medicine, University of Mississipi Medical Center, Jackson, Mississippi, USA
Received Date: 11/10/2021; Published Date: 08/11/2021
*Corresponding author: Chidubem Ekpereamaka Okechukwu, University of British Columbia, Vancouver, British Columbia, V6T 1X7, Canada
Abstract
Background
Chronic diverticulitis is a rare cause of colonic stricture, with less than 6% of large bowel obstructions secondary to diverticulitis. This highlights the need for a high index of suspicion by attending physicians. We report a case of a 63-year-old female, who presented with sudden onset of abdominal pain, nausea, and vomiting. Imaging revealed a colonic stricture with chronic diverticulitis and diverticulosis found on surgical intervention. It is pertinent to be aware of this relatively rare case of colon obstruction for prompt diagnosis and management. Contrast CT Scan plays a critical role in the diagnosis, and in guiding the albeit, controversial, surgical management of this condition.
Keywords: Stricture; Colon; Diverticulosis; Diverticulitis; Obstruction
Background
Diverticular disease occurs more frequently in the developed world and the aging demographics. It is prevalent in about 30% of individuals aged 60 and above, with slight preponderance in women between ages 50 and 70 years [1]. The sigmoid colon is involved in 95% of cases and this could become symptomatic in 70% of cases [1].
Diverticular disease could result in various life-threatening complications. These complications have been observed more in smokers, obese, and those who use non-steroidal anti-inflammatory drugs and low-fiber diets, and they include stricture, abscess, perforation, fistula, and bleeding. Though rare, strictures due to diverticular disease could cause complete bowel obstruction, in about 10% of large bowel obstructions [1].
Colorectal strictures are usually chronic and progressive. Though diverticular disease is the most common cause of benign colonic strictures, chronic diverticulitis is a rare cause of colon obstruction [2]. Only a few cases of colon strictures due to chronic diverticulitis has been reported, which poses a diagnostic challenge to differentiate from colon cancer, especially due to the varying clinical presentations. Hence the need for increased awareness for a high index of suspicion in the diagnosis of colonic strictures caused by diverticular disease in North America.
Case Presentation
A 63-year-old female presented to the emergency room (ER) of a community hospital with a four-day history of abdominal pain, nausea, and vomiting, which was sudden in onset and associated with a new high-grade fever (101°F) which began the day before the presentation. The patient’s physical examination was significant for abdominal distention, and positive rebound tenderness in the left lower quadrant. She had normal vital signs and an abnormally elevated Chloride level (111mg/dl). Other laboratory investigations were normal, and her home medications included levothyroxine, budesonide/formoterol, atorvastatin, butalbital/caffeine/Acetaminophen, and albuterol.
She has a past medical history (PMHx) of Chronic Obstructive Pulmonary Disease (COPD), Hypothyroidism, Dyslipidemia, a cerebral aneurysm with a surgical history of clipping of the aneurysm (twice), and a Total Abdominal Hysterectomy (TAH). She is retired and has a 35 pack-years history of cigarette smoking. She had never had a colonoscopy and had been taking magnesium citrate and Colace for the last three days before presentation, as recommended by her health care provider, without any relief. She endorsed not having a bowel movement or passing flatulence over the last three days.
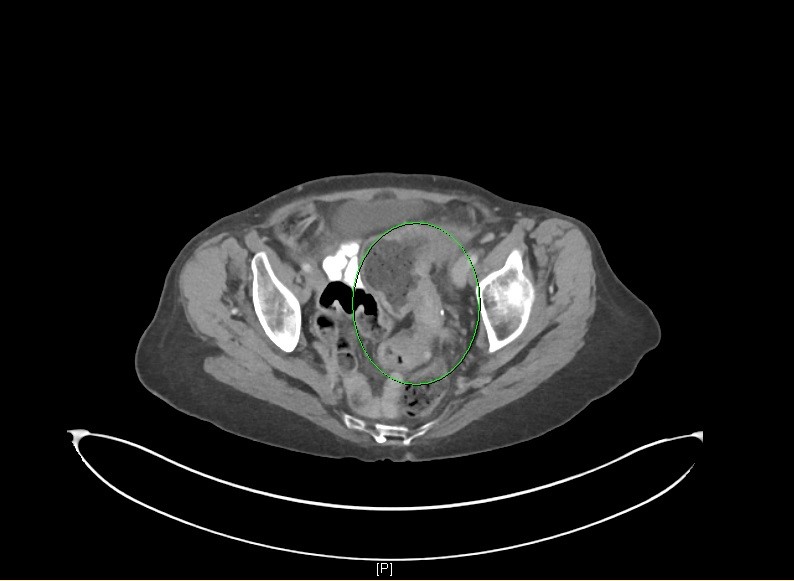
An abdominopelvic Computerized Tomography (CT) with oral and intravenous contrast in the ER showed fecalization of intraluminal contents within the distal ileum with a sharp transition point within the sigmoid colon, suggesting underlying partially occlusive etiology. Furthermore, there is moderate inflammation/mucosal thickening of the distal descending colon and sigmoid colon suggesting infection/inflammatory colitis.
She was kept Nil Per Oral (NPO), started on empiric intravenous antibiotics (Piperacillin/Tazobactam), intravenous morphine, and intravenous fluids. She was seen by General surgery and scheduled for exploratory laparotomy the next morning. She successfully underwent a low anterior colonic resection with primary end-to-end anastomoses of the distal third of the distal descending colon and the rectum.
Recovery was complicated by postoperative ileus on post-op day 4. Naso-Gastric Tube (NGT) with suction was initiated for 2 days. The patient received neostigmine and mineral oil that resulted in the resolution of ileus. Pathology from the resected distal colon was significant for diverticulosis with chronic diverticulitis associated with muscular hypertrophy and serosal fibrosis. She was discharged home on postoperative day eleven and educated to avoid cigarette use. She has been stable post-operatively with normal bowel movements.


Discussion
Diverticular disease is a common disease with increasing incidence in the aging population and Western countries. It varies widely by geographic location but the rate of hospitalizations has consistently increased over time in all age groups and in both sexes [3].
Diverticular disease consists of diverticulosis and diverticulitis, both of which were present in the patient. Diverticular disease is diverticulosis of the colon, which are small pockets from the colonic lumen caused by herniation of the mucosa through the weakened colonic wall, while chronic diverticulitis is characterized by frequent abdominal pain and chronic obstructive symptoms [4,5]. Around 80% of people with diverticular disease are asymptomatic but could become symptomatic in about 10-20% of cases, with resultant complications such as obstruction, perforation, abscess, and colonic stricture [6]. Colonic stricture caused by fibrosis or chronic inflammation of the colonic wall is most commonly caused by chronic diverticulitis with a high rate of bowel resection to relieve the obstructive symptoms [7].
The strictures commonly occur in the descending and sigmoid colon, but most especially at the sigmoid colon which is the narrowest part of the large intestine and with the highest intersegmental peristaltic pressure [8]. The resultant dilatation of the proximal colon and intraluminal stasis leads to overgrowth of intestinal flora, which in turn leads to translocation of the bacteria across the bowel wall with stool formation within the small bowel [9]. This is known as fecalization or small bowel feces sign, as seen in this patient. Fecalization of small intestines, which is a non-specific sign on contrast Computerized Tomography (CT) can also be seen in inflammation, ischemia, ileus, obstruction, and infection. Smoking, as in this patient, obesity, and a low fiber diet is believed to be some of the risk factors for symptomatic diverticular disease.
The diagnosis of diverticulosis and chronic diverticulitis is usually made by the characteristic clinical symptoms and radiographic findings [5]. Emesis, as seen in this patient, usually leads to electrolyte derangement due to loss of gastric hydrogen, chloride, and potassium which leads to metabolic alkalosis, but ironically, this patient had an abnormally elevated chloride level [9]. Colonoscopy has been considered in uncertain diagnosis and to rule out malignant obstruction, however, increased difficulty of diagnostic colonoscopy due to narrow lumen, colon spasms, and difficulty with angulations has limited its use [10]. Contrast CT is of great importance in the assessment of colonic abnormalities, as in addition to delineating the degree of bowel wall affectation, it provides extraluminal information that could impact treatment and prognosis, as well as, in exclusion of malignancy [8,11]. Another imaging modality which has been explored is the use of magnetic resonance imaging (MRI) which has been found to provide similar level of diagnostic accuracy in patients with diverticular disease [12].
Surgery is the definitive treatment of obstruction caused by colonic strictures in most cases. Acute surgical interventions are usually indicated when the colonic obstruction is not amenable to medical interventions and to completely exclude malignancies [13]. One-stage colorectal resection and primary end-to-end anastomosis are generally preferred [14]. Of great note, is the fact that this patient has had a total abdominal hysterectomy and a provisional diagnosis of intestinal obstruction secondary to adhesive bands could have been entertained before the diagnosis was confirmed to be colonic stricture due to diverticular disease after the surgery.
Conclusion
Chronic diverticulitis can initiate progressive chronic colon stricture, even in the absence of acute inflammation. Although colonoscopy can be helpful to rule out other differentials, CT plays a critical role in the diagnosis and overall management of the patient as a colonoscopy could be difficult in a narrow and tortuous colon. Surgical intervention has been proposed in most cases both for prophylaxis and treatment of complications, but this often depends on the individual case, the severity of the episode, age, risk factors, complications, comorbidities, and the surgeon.
Author Contributions
- Chidubem Ekpereamaka Okechukwu: contributed to conceptualization, drafted the original manuscript and performed literature review
- Shawntiah N. Jones: edited and revised the manuscript, and provided pictures
- Tobe Momah: contributed to conceptualization and revision of the manuscript.
All the authors read and approved the final version of the manuscript.
References
- Murphy T, Hunt RH, Fried M, Krabshuis JH. World Gastroenterology Organisation Practice Guidelines: Diverticular Disease: World Gastroenterology Organisation; 2021.
- Lerma MT, Hidalgo AM, Zorita BD. Toxic megacolon and perforation of the right colon due to sigmoid stenosis associated to chronic diverticulitis. Edorium Journals. 2018.
- Nguyen GC, Sam J, Anand N. Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol. 2011; 17(12): 1600-1605.
- Stollman N, Raskin JB. Diverticular disease of the colon. The Lancet. 2004; 363(9409): 631-639.
- Sheiman L, Levine MS, Levin AA, Hogan J, Rubesin SE, Furth EE, et al. Chronic diverticulitis: clinical, radiographic, and pathologic findings. AJR Am J Roentgenol. 2008; 191(2): 522-528.
- Spiller RC. Changing views on diverticular disease: impact of aging, obesity, diet, and microbiota. Neurogastroenterology & Motility. 2015; 27(3): 305-312.
- Sheiman L, Levine MS, Levin AA, Hogan J, Rubesin SE, Furth EE, et al. Chronic Diverticulitis: Clinical, Radiographic, and Pathologic Findings. American Journal of Roentgenology. 2008; 191(2): 522-528.
- Wan D, Bruni SG, Dufton JA, O’Brien P. Differential Diagnosis of Colonic Strictures: Pictorial Review With Illustrations from Computed Tomography Colonography. Canadian Association of Radiologists Journal. 2015; 66(3): 259-271.
- Jackson P, Vigiola Cruz M. Intestinal Obstruction: Evaluation and Management. Am Fam Physician. 2018; 98(6): 362-367.
- Fejleh MP, Tabibian JH. Colonoscopic management of diverticular disease. World J Gastrointest Endosc. 2020; 12(2): 53-59.
- Horton KM, Corl FM, Fishman EK. CT Evaluation of the Colon: Inflammatory Disease. RadioGraphics. 2000; 20(2): 399-418.
- Schreyer AG, Fürst A, Agha A, Kikinis R, Scheibl K, Schölmerich J, et al. Magnetic resonance imaging based colonography for diagnosis and assessment of diverticulosis and diverticulitis. Int J Colorectal Dis. 2004; 19(5): 474-480.
- Stocchi L. Current indications and role of surgery in the management of sigmoid diverticulitis. World J Gastroenterol. 2010; 16(7): 804-817.
- El Zarrok Elgazwi K, Baca I, Grzybowski L, Jaacks A. Laparoscopic sigmoidectomy for diverticulitis: a prospective study. JSLS. 2010; 14(4): 469-475.

