Surgical Exposure of Impacted Mandibular Second Premolar
Evangelia Theodoropoulou, Panagiotis Karakostas, Sotiria Davidopoulou*
School of Dentistry, Aristotle University of Thessaloniki, Greece
Department of Preventive Dentistry, Periodontology and Implant Biology, School of Dentistry, Aristotle University of Thessaloniki, Greece
Department of Preventive Dentistry, Periodontology and Implant Biology, School of Dentistry, Aristotle University of Thessaloniki, Greece
Received Date: 28/09/2021; Published Date: 05/11/2021
*Corresponding author: Sotiria Davidopoulou, Academic Fellow, Department of Preventive Dentistry,
Periodontology and Implant Biology, School of Dentistry, Aristotle University of Thessaloniki, Greece
Orcid no: 0000-0002-3436-3606
Abstract
Tooth impaction occurs when a tooth fails to erupt normally at its ideal place in the arch. Second premolars of the mandible are the third most prevalent teeth detected with impaction. A case report of a 13-year-old patient reported with an impacted right second premolar of the mandible is described. A brief review of the international literature is also presented regarding the proper diagnosis of impaction and the surgical technique of choice. In conclusion, a combined use of orthopantomography and cone beam computerized tomography establishes the level of a tooth impaction, while the surgical exposure of the crown of the impacted tooth constitutes a safe and predictable procedure.
Keywords: impacted premolar, tooth eruption, tooth impaction, surgical exposure
Introduction
Tooth impaction occurs as a result of the tooth incapacity of rising in the arch, during the normal period of eruption with closed apexes [1]. As regards mandibular second premolars, they consitute the third most frequent impacted teeth following third molars and maxillary canines [2]. The frequency of their impaction is reported to be 0,2-0,3%, with an increased prevalence in women [2,3].
Etiological factors may be divided to local and systematic. Local factors comprise lack of space in the arch, prolonged stay of a priamary tooth, redundant teeth, anchorage, trauma, root dysplasia and presence of a cyst [3]. Systematic causes are consisted of lack of vitamin D and calcium, endocrinopathies, developmental abdnormalities as well as dwarfism [3].
The level of impaction varies from case to case and regarding mandibular second premolars, it is defined as the distance between the cementum-enamel junction of distal tooth and the most coronal point of the crown of the impacted tooth [2]. Moreover, a tooth may have been erupted merely from the bone and not from the gum tissues. In this case the tooth is characterised as soft tissues impacted tooth [4].
The mineralization of premolars occurs from the age of 18-30 months and their eruption is between 10 and 13 years of life [5]. Premolars erupt following the first molar and canine of mandible, whereas the ideal position of their dental sperm is located between the roots of the second primary molar [4]. Therefore, the pathway of the premolar eruption follows mainly the absorption of the roots of the primary molar [4]. In case of lack of space, one of the premolars, usually the second one, cannot erupt and may stay impacted [4].
Case Report
A 13-year-old male patient was referred to our private practice by an orthodontist, due to the intraoral absence of the lower second right premolar. The orthopantomography revealed the impaction of the premolar, which was surrounded by an eruption cyst. The patient was prescribed a cone beam computerized tomography in order to reevaluate the case in cooperation with the orthodontist (Figure 1). The patient ‘s medical history revealed that he was systematically healthy. Following the evaluation of all the clinical and radiographic information, it was decided to proceed to the surgical exposure of the impacted premolar and the placement of an orthodontic bracket with metallic chain, aiming to help the tooth eruption via the orthodontic treatment.

Figure 1: Cone beam computerized tomography of the impacted lower right second premolar.
At the day of the operation, anesthesia of the inferior alveolar nerve block was conducted at the fourth quadrant, combined to supra-periosteal local infiltration at the buccal musoca of the premolars (Figure 2); lidocaine 1:80000 was the anesthetic of choice. An intra-crevicular incision was conducted at the distal side of the canine and at the first premolar, then an incision at the top of the alveolar crest, combined to a vertical releasing incision at the proximal side of the first molar. A full-thickness flap was elevated allowing adequate access of the surgical site. The operator drilled the buccal bone plate until the crown of the impacted premolar was revealed (Figure 3). The eruption cyst was removed and an orthodontic bracket and metallic chain was placed at the crown of the tooth with the use of composite resin (Figure 4). Following the replacement of the flap, the latter was sutured with simple interrupted sutures (Figure 5). The patient was prescribed antibiotic regimen containing a combination of amoxicillin (500mg) and clavulanate (125mg) three times per day for one week. Additionally, he was consulted to rinse with a mouthwash containing 0.2% chlorhexidine twice daily for one week.

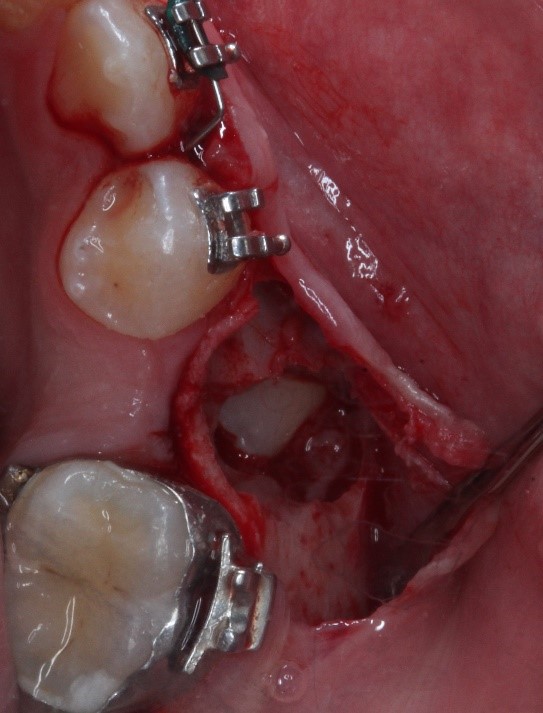


Figure 5: The flap was replaced and sutured with simple interrupted sutures.
The patient ‘s post-surgical course was uneventful, and the sutures were removed one week after the operation. The premolar was moved orthodontically, being visible intraorally, after 4 months (Figure 6).

Discussion
A case of patient with a lower impacted premolar was described above. The combined use of orthopantomography and cone beam computerized tomography let the proper evaluation of the tooth. Subsequently, the surgical exposure of the impacted tooth was conducted, followed by the placement of the chain and sutiuring of the flap at its intial site. Our case is in accordance to the average age of occurence (13 years of life), although our patient was a male in contrast to the female prevalence.
Impaction of premolars usually occurs due to local etiological factors [5]. Among all these factors, the location out of the arch is reported as the most frequent cause of impacted premolars, even though in few cases the tooth initally out of the arch may result in a normal eruption [2]. Other local factors include lack of space due to premature loss of primary molars, and anchored primary molars [4]. A number of genetic diseases including osteoporosis and Down syndrom may lead in impacted premolars as well [5].
Proper diagnosis demands combined clinical and radiographic evaluation of the case [5]. A cone beam computerized tomography constitutes the radiographic examination of choice in order to define the exact location of the tooth and the surrounding anatomical structures, such as the inferior alveolar nerve [5]. It is a common case an initial treatment plan based on evaluation merly with the use of a panoramic radiograph may be altered following a second evaluation with the use of cone beam computerized tomography, especially when the impacted tooth is located nearby major anatomical structures [6,7,8]. The latter lets the clinician to choose the appropriate surgical technique for the exposure of the impacted tooth, and the orthodontist to evaluate the level of difficulty during the tooth movement in the arch [5].
In case of impacted premolars, the surgical procedure of choice includes conservative crown exposureς even though this technique is unpredictable with difficult surgical steps [5]. This procedure is indicated merely for impacted premolars the vertical axis of which has a slope less than 45o compared to the vertical axis of the tooth at its ideal place [5]. In that case, a full-thickness flap is needed to be elevated buccally or lingually, depending to the loaction of the tooth, and afterwards a chain has to be placed at the crown of the tooth [5].
Prognogis of surgical exposure of impacted teeth is good. However, it is affected by the type of the surgical technique, the placement of the bracket and the orthodontic movement [9]. Additional factors that affect the prognosis of the procedure may be the dental plaque, the presence of periopathogens, the periodntal architecture and their interaction as well [9].
In conclusion, second premolars of the mandible are often detected as impacted. The combined use of orthopantomography and cone beam computerized tomography are crucial in order to evaluate the case and proceed to the proper surgical technique.
Competing interests
Authors declare no conflict of interest.
Grand information
There was no funding for the conduction of the present article.
Conclusion
Of the three pillars on which the prevention, fight and control of intestinal parasitoses is based, it is considered essential to enhance and invest in environmental sustainability, i.e. the provision of acceptable drinking water and the provision of excreta disposal systems or to proceed, if not, to the construction and use of latrines. This measures of environmental sustainability must be focused on the entirety of Department of Managua. The basic role of timely and relevant education and information for both urban and rural communities should be strengthened, particularly with regard to pollution of the teluric and water environment and the application of adequate personal hygiene measures, especially in the female sex and in the population over 5 years of age. And finally, the marked differences that the qualitative and especially the quantitative level, detected between the two parasitic groups protozoa and helminths, show is the positive role the Nicaraguan government plays with the helmintic deworming program in children carried out along with the childhood vaccination campaigns in most of the country’s departments.
Conflictis of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Acknowledgement
We are very grateful to the principals and teachers of each school, and the parents of the schoolchildren who have participated in this study.
The funds for this study were obtained from the Development Cooperation Project 2007 (s/n) of the Vice-Chancellor of Institutional Relations and Cooperation of University of Valencia-Estudi General (Valencia, Spain).
Declaration of Interests
None
References
- Dinoi MT, Lacarbonara M, Dimartino S, Monaco A, Marzo G. Periodontal probing of an impacted tooth recovered through a surgical-orthodontic approach: a case report. J Med Case Rep. 2014; 8: 25.
- Ismail MQ, Lauridsen E, Andreasen JO, Hermann NV. Ectopic eruption of the second premolar: an analysis of four different treatment approaches. Eur Arch Paediatr Dent. 2020; 21(1): 119-127.
- Chipashvili N, Kublashvili T, Beshkenadze E. Teeth Impaction: Challenges and Solutions. Georgian Med News. 2019; 289: 36-42.
- Muhamad AH, Nezar W, Omri E, Obaida A. Management of Lower Second Premolar Impaction. J Adv Dent Res. 2015; 1(1): 1-9.
- Alberto PL. Surgical Exposure of Impacted Teeth. Oral Maxillofac Surg Clin North Am. 2020; 32(4): 561-570.
- Araujo GTT, Peralta-Mamani M, Silva AFMD, Rubira CMF, Honório HM, Rubira-Bullen IRF. Influence of cone beam computed tomography versus panoramic radiography on the surgical technique of third molar removal: a systematic review. Int J Oral Maxillofac Surg. 2019; 48(10): 1340-1347.
- Hermann L, Wenzel A, Schropp L, Matzen LH. Impact of CBCT on treatment decision related to surgical removal of impacted maxillary third molars: does CBCT change the surgical approach? Dentomaxillofac Radiol. 2019; 48(8): 20190209. doi: 10.1259/dmfr.20190209.
- Tkachenko PI, Dmytrenko MI, Cholovskyi MO. Optimization of surgical-orthodontic treatment tactics in patients with impacted teeth. Wiad Lek. 2019; 72(5 cz 1): 838-845.
- Frank CA, Long M. Periodontal concerns associated with the orthodontic treatment of impacted teeth. Am J Orthod Dentofacial Orthop. 2002; 121(6): 639-649.

