Enveloped Silicone Foam for Breast Prostheses
Vladimir Frias*
Associate professor of oncology, Director of maxillofacial prosthetics, Roswell park comprehensive cancer center Buffalo, USA
Received Date: 28/09/2021; Published Date: 04/11/2021
*Corresponding author: Vladimir Frias DDS MS, Department of Oral Oncology, Roswell Park Comprehensive Cancer Center, Elm & Carlton Streets, Buffalo, NY 14203, USA
Abstract
The fabrication of breast prosthetics for post-mastectomy patients has often been considered a part of maxillofacial prosthetics since the techniques used in the creation of the prosthetic often utilizes the procedures and materials similar to those used in head and neck prosthetic reconstruction. A common complaint from patients who use stock prosthetics are the poor fit and contour of the prosthesis while the creation of custom prosthetics in solid silicone adds weight due to the density of medical grade silicone. A method of creating a customized prosthesis with reduced weight by enveloping silicone foam in medical grade silicone is described along with a case report.
Keywords: Silicone foam; Custom breast prostheses; Mastectomy
Introduction
The psychosocial effect of a breast cancer diagnosis has long been reported in the literature and the removal of one or both breasts as part of the surgical treatment of breast cancer is often adds multiple complex layers of physical and psychosocial distress, especially when a surgical reconstruction is not an option [1-3].
The use of an External Breast Prosthesis (EBP) has often been recommended for patients who are unable to have a satisfactory surgical reconstruction performed due to local or systemic factors. Other patients may elect to have an EBP to lessen the burden of the multiple surgeries often required for an adequate surgical reconstruction or as a temporary prosthesis [4].
EBP’s are generally stock prosthetics that are fitted at the hospital by a breast care nurse or in-store with limited options for customization. Many of the concerns with stock prostheses are due to poor adaptation and contour and result from the fact that stock prosthetic tissue surface does not accurately mold to the residual breast or chest wall and the external surface of a stock prosthetic does not always match the opposing breast even with the support of an undergarment and the concealment of clothing. For most women, the greatest benefit of a prosthesis is to restore their pre-surgical appearance which not only improves a patient’s physical but psychological well-being [5]. This is best served with a custom- made prosthesis. Custom breast prostheses also provide a cushion during the post-surgical period as incisions heal as well as help hold bras and undergarments in place so that they fit securely and don't irritate healing tissues6. Radical mastectomies can often change a patient’s center of gravity and this has been shown to happen even in the case of partial mastectomies or lumpectomies7. While the creation of custom EBP by an experienced practitioner can often reduce or eliminate many of a patient’s concerns with balance, the increase in contour of a prosthesis to satisfy esthetic demands can also have a detrimental effect on posture due to the increased weight and there must be a consideration for the type of material used in EBP fabrication [8].
Materials used in over-the counter or stock prostheses usually consist of silicone, foam, natural or synthetic fiber encased in a natural or synthetic material. The silicone material is often used because of its weight and closer similarity to a natural breast as far as feel or movement however complaints usually concern the weight and lack of breathability of the material. Cotton or polyester filled prostheses are lighter and allow for increased air circulation however their relative lack of stiffness prevents natural contours and possible indentation during use. Foam materials usually provide improved contours but do not flex naturally on movement and suffer from similar indentation issues as seen in fiber-based prostheses.
Some studies have shown that weight of a prosthesis does not affect the level of comfort a patient experiences9 however since discomfort and mobility issues are proportional to increased breast size, the larger the defects in the chest wall or contra-lateral breast size will result in an increase in the number of complaints with discomfort due to weight10. Another issue is the difference in density between the natural breast tissue versus the prosthetic replacement material. The average density of fat, the primary component of breast tissue averages .9gm/ml [11] while the density of medical grade silicone rubber varies from 1.2 to 3gm/ml depending on its composition [12]. These calculations are complicated by the fact that breast tissue is composed of both fatty tissue as well as glandular and fibrous tissue and breast density can vary depending on these factors. Mammograms can often give us the relative density of breast tissue however the rating of breast density based on the appearance of the mammogram is speculative and difficult to accurately estimate and compare. Because of this, the choice of material for breast prosthetics relies on discussion of the options with the patient and the necessary adjustment of weight and contour from existing prostheses.
The following case report describes a method to reduce the weight of an EBP as desired by the patient.
Case Report
A patient was referred to the maxillofacial prosthetics department from the breast clinic with complaints of discomfort with her current stock prosthetic. She had a left mastectomy performed 2 years prior along with an extensive removal of muscle and a hollowing of her chest wall as well as the tagging of remnant tissue under her left armpit (Figure 1). Due to the size of the mastectomy and adjuvant radiation therapy she was not a candidate for surgical reconstruction.
She had been fitted with multiple commercial prosthetics over the two years since her mastectomy and her stock prosthetic showed poor fit against the chest wall and a flattened appearance with traditional and compression fit undergarments. This deficiency was minimized by wearing loose fitting outerwear however she was interested in a custom fitting prosthesis which would allow her to wear a high-necked swimsuit. A custom EBP was created for her at the maxillofacial clinic using medical grade silicone rubber [Factor II, Lakeside, AZ] which satisfied her esthetic demands however she returned to the clinic a few months later complaining of excessive weight and resultant back pain from wearing the new prosthesis. It was decided to fabricate a new prosthesis for her with a silicone foam encased in solid silicone rubber to maintain the shape and maintain a comfortable smooth surface while reducing the weight.
A new impression was taken of the chest wall defect with minor displacement of the axillary tissue to allow tucking of the margin under the remnant (Figure 2). The impression was made with a layer of silicone impression material [Silicone Clone, Factor II, Lakeside, AZ] embedded with gauze pads that allowed retention of a fast-setting stone reinforcement [Snow White, Kerr Corp. Brea, CA]. An impression of the opposing breast was created by covering the patient’s choice of a compression undergarment in aluminum foil and painting on a layer of fast setting stone (Figure 3). On the peeling of the foil a hollow breast form was created which allowed envisioning the natural breast contours. A wax form of the breast was created and verified clinically.


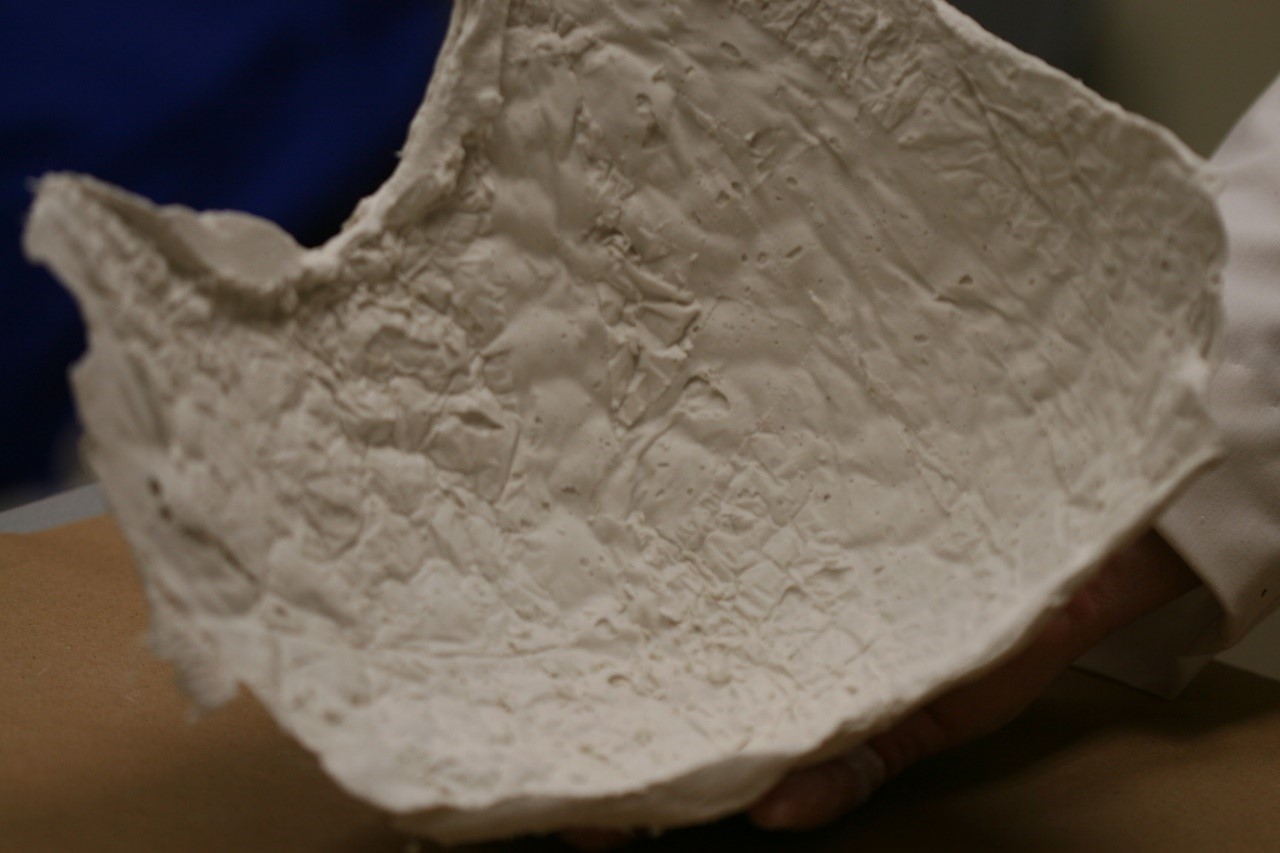
Figure 3: Plaster impression of the opposing breast.
A cut back on the internal contours of the prosthesis was also created to reduce weight while maintaining the stiffness and circumferential contact of the prosthesis. The prosthesis was then invested in Type IV stone [Silky rock, Whip-Mix, Louisville, KY] since the prosthesis was too large to fit in a flask and the compression needed during the processing of foam silicone necessitates extra strength especially along the central portions of the wax pattern where the contours are most convex and the overlaying stone is the thinnest (Figure 4).

Figure 4: Wax form of the breast prosthesis invested in stone.
The investment was separated, and the two halves were painted with a 2mm thick layer of RTV silicone rubber [A-588-1, Factor II, Lakeside, AZ] and allowed to partially cure at room temperature. The silicone foam [Silicone Foam, Factor II, Lakeside, AZ] was them mixed according to manufactures directions and poured into one half of the investment (Figure 5). Since the foam expands to 5:1 ratio, an estimation of the size of the mold is helpful in determining the amount of foam used. This can easily be calculated by melting the wax pattern and measuring its liquid volume. The volumetric amount of the painted silicone shell is subtracted from this volume and one fifth of this remaining measure in foam silicone can be used to the fill the cavity. Since the two silicones will admix during vulcanizing it is important to allow the first layer of silicone to only partially cure to maintain an outer seal. Full cure is not recommended as this will prevent and intimate seal with the foam and the opposing half of silicone.
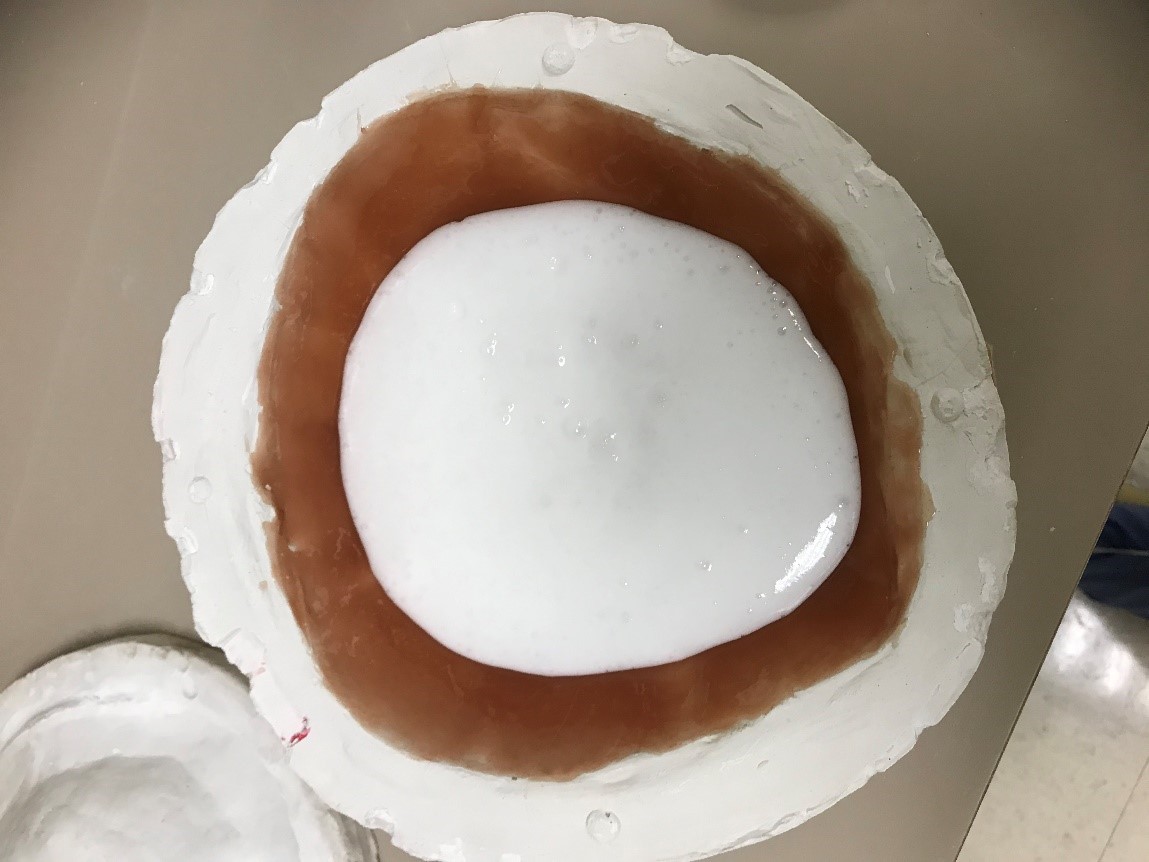
Figure 5: Single layer of partially cured RTV silicone filled with measured foam silicone.
Once the mold is filled with the foam, it then closed and compressed with static weight and allowed to cure at room temperature for 24 hours or in a dry heat oven. The prosthesis can be divested by routine methods and the excess silicone is trimmed (Figure 6). Most breast prosthetics are not visible beyond the undergarment and are not expected to be realistically colored to match the patient’s skin however some coloration is recommended so that the white of the silicone or the translucency of the RTV silicone is not visible under a thin garment. A prosthetic created with this method will require a higher color saturation of the shell silicone as the white of the foam will eventually blend with it and reduce the chroma.

Figure 6: Devested prosthesis.
The final prosthesis is then tried in and verified for fit and comfort (Figure 7). A weight comparison of the original silicone prosthesis with a chest wall cut back compared to a similarly created prosthesis with the foam inclusion showed a reduction in weight of 35% with a foam inclusion. The patient was comfortable with the reduced weight of the prosthesis and found the contour, fit and flexibility of the foam prosthesis was similar to the original silicone prosthesis and allowed for use in undergarments as well a swimwear.

Conclusion
External breast prostheses are a vital part of the post-surgical care for mastectomy patients whether used as a temporary or definitive replacement for the missing breast tissue. The use of custom created silicone prostheses is the gold standard for EBP’s however in certain cases the weight of silicone can cause multiple issues including pain and postural problems. The use of a foam underlayment in the prosthesis can alleviate many of the weight issues in silicone breast prostheses and allow for the creation of a more natural and comfortable feel for these prostheses.
References
- Carlsson M, Hamrin E. Psychological and psychosocial aspects of breast cancer and breast cancer treatment. A literature review. Cancer Nurs. 1994; 17(5): 418-428
- Ganz PA. Psychological and social aspects of breast cancer. Oncology 2008; 22(6): 642-646.
- Izci F, Algun AS, Findikli E, Ozmen VJ. Psychiatric symptoms and Psychosocial problems in patients with breast cancer. Breast Health. 2016; 12(3): 94-101.
- Lee CN, Hultman CS, Sepucha K. What are patients goals and concerns about breast reconstruction after mastectomy? Ann. Plast, Surg. 2010; 64(5): 567-569.
- Jetha ZA, Gul RB, Lalani S. Womens experiences of using external breast prosthesis after mastectomy. Asia Pac. J. Oncol. Nurs. 2017; 4(3): 250-258.
- Glaus SW, Carlson GW. Breast J. Long term role of external breast prostheses after total mastectomy. 2009; 15(4): 385-393.
- Atanes AC, Dias MD, Yugo J et al. Body posture after mastectomy: Comparison between immediate breast reconstruction versus mastectomy alone, Physiotherapy Res. Int. 2017; 22(1).
- Hojan K, Manikowsak F, Chen BP, et al. The influence of an external breast prosthesis on the posture of women after mastectomy. J. back. Musculoskelet. Rehabil. 2016; 29(2): 337-342.
- Can the weight of an external breast prosthesis influence trunk biomechanics during functional movement in postmastectomy women? Hojan K, Manikowska F. Biomed Res Int. 2017; 2017: 9867694.
- External breast prostheses: misonformation and false beliefs. Healey IR. Gen. med. 2003; 5(3): 36.
- Body fat in adult man: semicentenary of fat density and skinfolds. Fidanza F. Acta Diabetol. 2003; 40 Suppl. 1: S242-245.
- Biomechanical characterization of a low-density silicone elastomer filled with hollow microspheres for maxillofacial prostheses. Liu Q, Shao L et al. J. Biomater. Sci. Polym. Ed. 2013; 24(11): 1378-1390.

