An Unusual and Near-Fatal Result of Acupuncture for Right Shoulder Girdle Pain Syndrome: Staphylococcal Aureus Cervical Spine Osteomyelitis with Paravertebral and Epidural Abscess
Dennis Nixon, Li Feng, Dan Xu,*, Dingbang Chen
Curtin Medical School, Faculty of Health Sciences, Curtin University, Perth, Australia
Deaprtment of Neurology, First Affiliated Hospital, Sun Yat-sen University, China
Medical Education & General Practice, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
Received Date: 09/10/2021; Published Date: 04/11/2021
*Corresponding author: Dan Xu, Curtin Medical School, Faculty of Health Sciences, Curtin University, Perth, Western Australia, Australia. Medical Education & General Practice, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
Abstract
A 42-year-old Chinese male presented with pain and weakness in right shoulder, upper and lower limbs. Within 24 hours, he was wheelchair-bound. The acupuncture from C5 to T2 did not relieve his pain, instead made it worse, with sleep disturbance and tender redness on the acupuncture sites in the ensuing week. One week later, the patient suddenly developed fever, cough and paralysis. Clinical diagnosis of chest infection, severe cellulitis and soft tissue infection with possible spread into the cervical spine were suspected. With IV antibiotics and antipyretics, cellulitis and chest infection resolved. Investigation with spinal MRI disclosed C7-T1 osteomyelitis, C5-T2 paravertebral and epidural abscess. His paralysis was from myelitis secondary to paravertebral and epidural abscess. The salient learning points include differential diagnosis in acute causes of paralysis with a background of shoulder girdle pain syndrome, for the most relevant investigations, immediate and long-term management, especially as a complication of acupuncture.
Keywords: Shoulder girdle pain syndrome; Spinal abscess; Acupuncture; Paravertebral and epidural abscess
Introduction
Shoulder girdle pain syndrome is a neurologic pain syndrome of unknown cause, characterized by the onset of severe pain affecting the shoulder girdle muscles sporadically; often preceded by some antecedent event such as an upper respiratory infection, hospitalization, vaccination, or nonspecific trauma [1,2]. This common musculoskeletal pain syndrome is usually caused by soft tissue injuries or arthritis of shoulder and cervicothoracic spine [3].
Cervical paravertebral and epidural abscess and osteomyelitis are certainly a rare combination of serious spinal infection in a patient with shoulder girdle pain syndrome. This report addresses the approach to a patient presenting with acute, rapidly progressing paralysis. If not diagnosed quickly, this can result in lasting neurological deficit, and death.
We present a case of shoulder girdle pain syndrome in a 42-year-old Chinese man with both C7-T1 osteomyelitis and C5-T2 paravertebral and epidural abscess in MRI scan of cervicothoracic spine for discussion. The case highlights the risk of alternative medical treatment using acupuncture, which has resulted in cervicothoracic spine osteomyelitis and the potentially fatal paravertebral and epidural abscess with associated myelitis, leading to long-term disability.
Case Report
A 42-year-old Chinese man describes a two-day history of worsening right shoulder girdle and upper back pain which he attributed to his poor sleep posture and work. He states that he has had right shoulder girdle and upper back pain for a couple of years. Patient had regular acupuncture for his chronic neck and shoulder pain related to his occupation as a welder. Recent occupational and social history does not reveal any strenuous work, trauma and upper back or shoulder injuries. He consulted a massager with some relief after a few massage sessions before he travelled to Kenya for work. However, his right shoulder girdle and upper back pain worsened with associated sleep disturbance, so he received a few home sessions of acupuncture, with what he recalls as recycled needles in Kenya for the severe pain with acupuncture points from C6 to T2 but provide no pain relief (Jia Ji Xue, locating along both sides of spinal column), instead made it worse.
On the 8th day after pain onset, he suddenly presented with intermittent swinging fevers of 40-degrees Celsius, cough, and weakness of the right upper limb and both legs. The weakness rapidly progressed to central quadriparesis and he was bound to a wheelchair within 12 hours, complicated with constipation and abdominal bloating. He was sent to a local hospital where he was diagnosed with chest infection, and cellulitis at the back of his neck. It was postulated that soft tissue infection spread to cervical spine causing paralysis. He received intravenous antibiotics and anti-pyretic medications in Kenya. The fever gradually faded with persistent paralysis and he was flown back to present at a tertiary hospital in Guangzhou, China. He had no significant past medical history, family history or social history.
Upper and lower limb neurological examination revealed increased muscle tone of both upper and lower limbs. There was absent power and sensation in upper and lower limbs, except his right shoulder which has slight sensation accompanied with numbness. Reflexes were absent for triceps in his right arm, but present in his left arm. Patient’s biceps and brachioradialis reflex were present in both arms. Hoffman’s sign was positive for his right hand. Both his patellar reflexes showed significant hyperreflexia. Babinski’s test was positive. His ankle reflex showed hyperreflexia with clinically significant clonus. Patient’s neurological examination was consistent with a clinical diagnosis of upper motor neurone lesion most likely in the upper thoracic and lower cervical spine. At his lower-neck, redness and swelling were notable. Physical examinations in other organ systems, and the rest of the neurological exam were unremarkable.
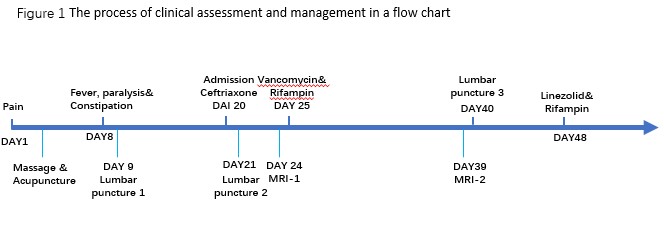
As we proceeded to special investigations, blood work-up and the patient’s MRI scan of cervical and upper thoracic spine were organized to identify the most likely upper motor neuron lesion contributing to his rapid paralysis. The process of clinical assessment and management are briefly summarised in a flow chart (Figure 1).
Investigations
Initially, an ultrasound of the cervicothoracic spine region with redness and warmth showed no fluid collection, revealing only soft tissue oedema.
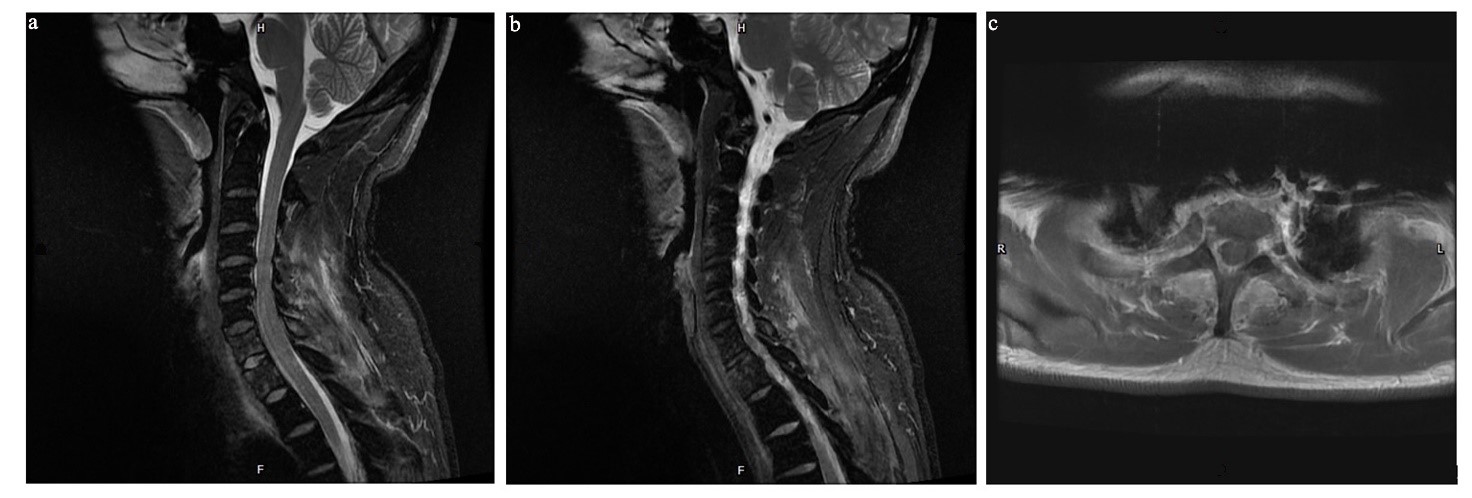
Given his neurological symptoms, the first MRI scan of cervical and upper thoracic spine was ordered on admission, showing osteomyelitis (Figure 2) C7 – T1 and paravertebral abscess (Figure 3) from C5 – T2.
Blood investigations showed raised total white blood cell count with neutrophilia and elevated C reactive protein (CRP), consistent with most likely staphylococcal aureus sepsis.
Blood culture was positive for staphylococcal aureus.
For viral screen, mNGS and antibodies were both negative.
Imaging and clinical picture highly reflected the presence of a paravertebral abscess resulting in acute myelitis. 15 days post-admission, due to the lack of clinical improvement, a second MRI was performed, showing a spread of the lesion involving the epidural space.


Differential Diagnosis
The patient’s initial shoulder pain, as the patient self-explained, was most likely due to poor sleeping posture and chronic shoulder pain for which the patient sought alternative treatments including massages and acupuncture. Despite some pain relief from the treatment, the rapid progression to quadriplegia suggested transverse myelitis as another possible differential diagnosis, though rare [4]. Ischaemic injury, such as anterior spinal artery syndrome [4], is another likely diagnosis, whereby flaccid sudden paralysis occurs below region of spinal cord lesion. Raised neutrophil and MRI scan result made it less likely to distinguish between the inflammatory process of transverse myelitis and the ischaemic process of anterior spinal artery syndrome. Another important differential diagnosis for such rapid progression of quadriplegia is an epidural spinal abscess, which often arise from epidermal lesions/infections [5]. Spinal epidural abscess manifests with pain at site of abscess, can be febrile or afebrile, with neurological deficits ranging from motor and sensory disturbance, bowel and bladder dysfunction to paralysis [6].
The MRI scan of cervicothoracic spine in our case confirmed the diagnosis of C5-T2 paravertebral and epidural abscess and C7-T1 osteomyelitis. Given the cellulitis on posterior neck, we proposed the most likely mechanism in which the bacteria introduced, was through acupuncture using inappropriately-sterile needles during his work-related trip in Kenya. The most likely diagnosis therefore, would be acupuncture-induced staphylococcal aureus C5-T2 paravertebral and epidural abscess and C7-T1 osteomyelitis causing secondary acute myelitis.
Treatment
Vertebral osteomyelitis associated with paravertebral and epidural abscess resulting in myelitis requires urgent empirical therapy. This involves intravenous and oral antibiotic therapy for at least 6 weeks, with a minimum of 4 weeks intravenous therapy [7,8]. The initial antibiotics should include vancomycin, flucloxacillin, and ceftriaxone (glycopeptide antibiotic with narrow-spectrum penicillin and third generation cephalosporin respectively) [8,9]. The antibiotics regimen is usually adjusted according to bacteria culture sensitivity: staphylococcus aureus sensitive to flucloxacillin. The duration of treatment is largely dependent on the following factors [7]:
1) Whether the abscess is surgically drained
2) The clinical measurable improvement of the patient during treatment
3) Susceptibility of pathogen to treatment
4) Radiological evidence of improvement
In this case, following the first MRI, patient was treated with IV flucloxacillin and prednisolone targeting the lower neck cellulitis, paravertebral abscess and acute myelitis.
The surgical debridement was performed after second MRI, with surgical debris sent for growth and susceptibility, which was confirmed to be staphylococcus aureus with sensitivity to flucloxacillin, cephalosporin and vancomycin.
Outcome and Follow-up
The patient had received four weeks of combined intravenous antibiotics including flucloxacillin, ceftriaxone and vancomycin since the start of the focal neurological deficit at the time of the review.
He regained some of his sensory function of hands and trunk as well as a small improvement in motor functions of his right arm. He is predicted to have a few more months of antibiotics. His right arm still had sensory disturbance of paraesthesia at C7-T1 dermatomal distribution. His right arm biceps reflex and brachioradial reflex were present, while his Babinski response was still positive. Patient was undergoing a comprehensive rehabilitation program as well as regular administration of intravenous and oral flucloxacillin. Repeat MRI scan shows improvement of both vertebral osteomyelitis and paravertebral and epidural abscess (Figure 4). Patient was still immobilised with hard cervical collar to ensure the stability of his cervical spine. The follow-up plan would be to continue rehabilitation and antibiotics for the next three months before the next treatment review. Upon follow-up, the patient had a Modified Rankin Scale of +4; he is now wheelchair bound with minimal motor recovery from lower limbs.
Discussion
Spinal epidural abscess is a rare clinical encounter accounting for 0.005% of hospital admissions.[10] Case report literature review showed that radiation related cervical osteomyelitis and epidural abscess for a patient with hypopharyngeal wall carcinoma was reported by Ueki et al [11]. In their case, it was suggested that post-radiation necrosis of posterior pharyngeal wall could develop into cervical spine osteomyelitis [11]. A systematic review by Turner et al. discusses cervical spinal epidural abscesses [12]. This review attributes the most common risk factor for spinal epidural abscesses to drug use [12]. Iatrogenic risk factors which were less common included prior surgery, neck radiation, deep paravertebral injections of the neck and peridural injections [12]. Vertebral osteomyelitis and spinal epidural abscess as a result of acupuncture is rare and not widely reported especially in cervical spine. One case reported [13] of an uncommon complication of acupuncture and wet cupping with another middle-aged man having neck pain and fever and subsequent diagnosis of cervical spine epidural abscess at C4 to T2 by MRI scan. The focal neurological symptoms and signs resolved partially after treatment with antibiotics. The case [13] concluded that acupuncture and wet-cupping therapy should be considered as a cause of spinal epidural abscesses in patients with relevant history. Education with guidelines regarding hygienic measures should be provided to acupuncture and wet-cupping practitioners. This case [13] did not report the bacteria responsible for the cervical spine epidural abscess, while our case reported the acupuncture-introduced Staphylococcal aureus being responsible for C5-T2 spinal abscess and C7-T1 osteomyelitis.
In review of case report literature with spinal abscess formation following acupuncture, seven cases including our case have reported the responsible bacteria [14,15,16,17,18]. Six of seven cases were treated successfully with an extended course of antibiotics and serial MRIs with one case requiring decompression laminectomy. The most common causative pathogen was Staphylococcus aureus, responsible for five of these cases, the others being Serratia marcescens and Escherichia coli. It is to be noted that unlike our patient, none of the cases in literature had profound neurological deficits before treatment. Our case has highlighted a rare but potentially severe complication of acupuncture, which only had an incidence of 0.55 per 10000 patients based on one study [19], even rarer cause would be myelitis following acupuncture. Common complications of acupuncture include acupuncture site infection and rarer complications of neurovascular damage and pneumothorax have been reported [19].
A unique learning point in our case is to stress the importance of identifying red-flag history of recent acupuncture usage, particularly the home-based acupuncture with recycled needles of inappropriate sterilisation, which can lead to an early diagnosis and prompt treatment in order to minimize permanent neurological deficit and prevent the potentially fatal outcome of acute myelitis secondary to paravertebral and epidural abscess.
Authorship Criteria:
Dan Xu and Ding bang Chen concepted and designed the initial draft of the case. Dennis Nixon and Li Feng drafted the initial manuscript of the case. All authors reviewed and edited the revised and final manuscript of the case for important intellectual content. All authors have approved the submitted manuscript of the case and take the responsibility for the integrity of the work.
Conflicts of Interest/ Competing Interests:
All authors have no conflict of interests to declare.
Grant Information:
All authors received no specific funding for this work.
Acknowledgements:
Staff at Curtin Medical School of Curtin University and First Affiliated Hospital of Sun Yat-Sen University
References
- van Alfen N. Clinical and pathophysiological concepts of neuralgic amyotrophy. Nat Rev Neurol 2011; 7: 315-22.
- Feinberg JH, Radecki J. Parsonage- turner syndrome. Hss J, 2010; 6: 199-205.
- Brown R, O’Callaghan J, Peter N. Parsonage Turner syndrome caused by Staphylococcus aureus spondylodiscitis BMJ Case Rep 2020;13: e233073. doi:10.1136/bcr-2019233073.
- Trentman TL. Transverse myelitis. In: Sibell DM, Kirsch JR, editors. 5-minute pain management consult [Internet]. 1st ed. Philadelphia (USA): Lippincott Williams and Wilkins; 2006; p 304-305.
- Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2000; 23(4): 175-204; discussion 205. doi: 10.1007/pl00011954.
- Sexton DJ, Sampson JH. Spinal epidural abscess. 2021 [cited 2021 May 18]. In UpToDate [Internet]. Waltham (MA): UpToDate Inc. Available from: https://www-uptodate-com.dbgw.lis.curtin.edu.au
- Spinal epidural abscess. 2019 [cited 2020 Mar 21]. In: eTG Complete [Internet]. Melbourne (Australia): Therapeutic Guidelines Limited.
- Osteomyelitis. 2019 [cited 2020 Mar 21]. In: eTG Complete [Internet]. Melbourne (Australia): Therapeutic Guidelines Limited.
- Hyslop NE, Hasbun R. Infectious diseases of the spinal cord and peripheral nervous system. In: Gorbach SL, Bartlett JG, Blacklow NR, editors. Infectious diseases [Internet]. 3rd ed. Philadelphia (USA): Lippincott Williams and Wilkins; 2003 [cited 2020 Mar 21]. p 1359-1361.
- Darouiche RO. Spinal epidural abscess. N Engl J Med 2006; 355: 2012-2020
- Ueki Y, Watanabe J, Hashimoto S, et al. Cervical spine osteomyelitis and epidural abscess after chemoradiotherapy for hypopharyngeal carcinoma: a case report. Case Rep Otolaryngol [Internet], 2014:1-4. doi:10.1155/2014/141307
- Turner A, Zhao L, Gauthier P, et al. Management of cervical spinal epidural abscess: a systematic review. Ther Adv Infectious Dis [Internet]. 2019 [cited 2020; 6: 1-17. doi:10.1177/2049936119863940
- Yao Y, Hong W, Chen H, et al. Cervical spinal epidural abscess following acupuncture and wet-cupping therapy: A case report. Complement Ther Med 2016;24: 108-110 https://doi.org/10.1016/j.ctim.2015.12.002Get rights and content
- Yang CW, Hsu SN, Liu JS, et al. Serratia marcescens spinal epidural abscess formation following acupuncture. Intern Med 2014; 53: 1665–1668.
- Yazawa S, Ohi T, Sugimoto S, et al. Cervical spinal epidural abscess following acupuncture: successful treatment with antibiotics. Intern Med 1998; 37: 161–165.
- He C, Wang T, Gu Y, et al. Unusual case of pyogenic spondylodiscitis, vertebral osteomyelitis and bilateral psoas abscesses after acupuncture: diagnosis and treatment with interventional management. Acupunct Med 2015; 33: 154–157.
- Bang MS, Lim SH. Paraplegia caused by spinal infection after acupuncture. Spinal Cord. 2006; 44:258–259.
- Yu HJ, Lee KE, Kang HS, et al. Teaching neuroimages: multiple epidural abscesses after acupuncture. Neurology 2013; 80: 1–2.
- White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med 2004; 22: 122–133.

