Subarachnoid Hemorrhage Like Appearance After Cervical Epidural Neuroplasty: A Case Report
Gözde Dağıstan*
Akdeniz University University Faculty, Anesthesiology and Resuscitation ABD, Turkey
Received Date: 27/09/2021; Published Date: 01/11/2021
*Corresponding author: Gözde Dağıstan, Akdeniz University University Faculty, Anesthesiology and Resuscitation ABD, Algoloji BD, Antalya, Turkey
Abstract
Background: Percutaneous epidural neuroplasty is a minimally invasive procedure used in chronic spinal pain. Although it seems like a simple procedure, many complications may develop during or after the procedure.
Case presentation: A 45-year-old male patient applied to our clinic with severe neck pain radiating to his left arm. On MRI of the patient, a diffuse disc protrusion indenting the anterior subarachnoid space was observed in the C4-5 disc. Although the patient used medications, his pain continued. Interlaminar epidural steroid was applied to the patient but the patient's pain persisted in his follow up one month later. It was decided to perform cervical epidural neuroplasty. Catheter malposition was observed catheter into the intradural space during the procedure. The procedure was terminated.
Conclusion: We report a case of subarachnoid hemorrhage like appearance after cervical percutaneous neuroplasty. Our case is the second case of subarachnoid hemorrhage like appearance reported after percutaneous epidural neuroplasty.
Keywords: Cervical epidural neuroplasty; Subarachnoid hemorrhage
Abbreviations: PEN: Percutaneous Epidural Neuroplasty; MRI: Magnetic Resonance İmaging; CT: Computerized Tomography; SAH: Subarachnoid Hemorrhage
Introduction
Percutaneous Epidural Neuroplasty (PEN) is a minimally invasive procedure used in chronic spinal pain [1,2]. PEN also known as percutaneous adhesiolysis or the Racz procedure, is effective in the treatment of low back and/or extremity pain symptoms which has not responded to more conservative treatment, including epidural injections [3]. The goal during lysis of epidural adhesions is to reduce mechanical barriers preventing medications from reaching areas of pathology in the epidural space [2].
Although it seems like a simple procedure, many complications may develop during or after the procedure. These complications may be due to the procedure itself or the drugs used during the procedure. The development of neurological deficit, epidural or cerebral hemorrhage are some of the serious complications.
Case Presentation
A 45-year-old male patient applied to our clinic with severe neck pain radiating to his left arm. On Magnetic Resonance İmaging (MRI) of the patient, a diffuse disc protrusion indenting the anterior subarachnoid space was observed in the C4-5 disc. At this level, stenosis was observed in the left neural foramen with the contribution of spondylotic changes. Although the patient used pregabalin 150 mg 2x1/day and tramadol 50 mg 3x1/day, his pain continued. Interlaminar epidural steroid was applied to the patient but the patient's pain persisted in his follow up one month later. It was decided to perform cervical epidural neuroplasty.
A pop feeling was felt while advancing the catheter during the procedure. Due to the suspicion that the catheter ruptured the dura, approximately 1.5-2 cc of contrast was administered through the catheter. Intrathecal spread of the contrast was observed (Figure 1).
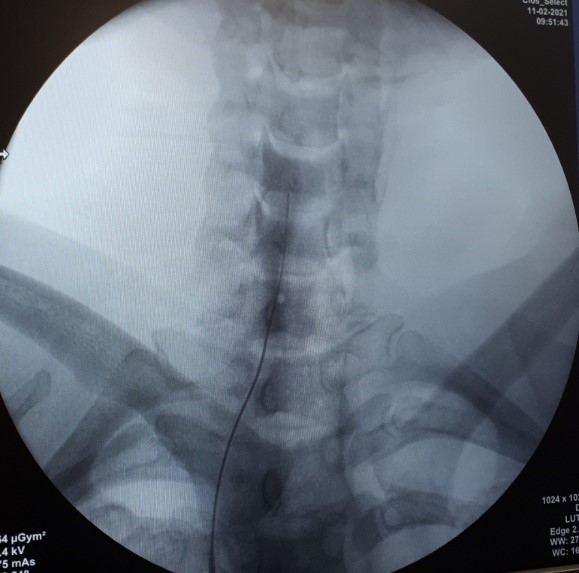
Figure 1: Intrathecal spread of the contrast on anteroposterior view.
The procedure was terminated removing the catheter. The patient was transferred to his room. About 2-3 hours later, the patient complained of severe headache. All of his the vital signs were stabile. His neurologic examination was normal. His Glasgow Coma Scale was 15. A Computerized Tomography (CT) of his brain showed a subarachnoid hemorrhage (SAH) like appearance. Hyperdensities were found in the cerebral sulci and cerebellar folia on CT imaging (Figure 2).
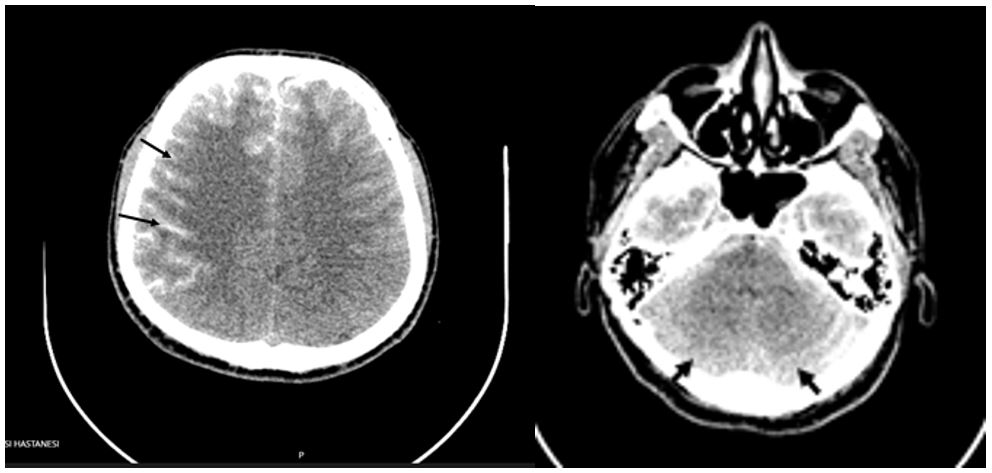
Figure 2: Hyperdensities in the cerebral sulci and cerebellar folia.
Similar hyperdensities were also observed in the prepontine, interpeduncular, quadrigeminal and ambient cisterns (Figure 3).

Figure 3: Hyperdensities in the quadrigeminal and ambient cisterns.
In addition, there were hyperdensities in the extraaxial distance in the cervical canal (Figure 4). Increased lucency was observed in the mesencephalon, pons, brain stem and periventricular white matter. There were millimetric air densities around the C1-C2 intervertebral disc (Figure 4).
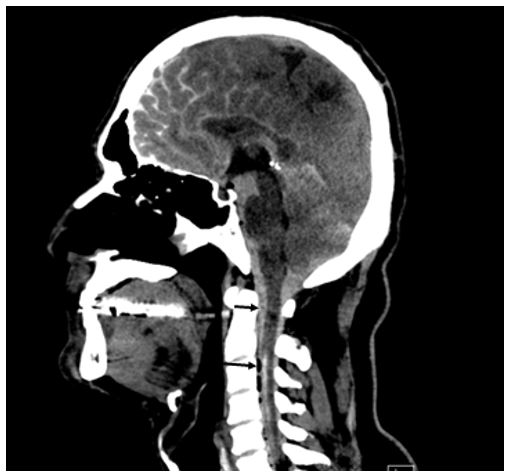
Figure 4: hyperdensities in the extraaxial distance in the cervical canal and millimetric air densities around the C1-C2 intervertebral disc.
A follow up CT scan after one day was completely normal. The patient was discharged without any neurological deficit. The patient was neurologically asymptomatic during the three month follow up.
Discussion
Radiographic mimics of SAH have been reported in case reports [4,5]. A contrast enhancement of the subarachnoid space after caudal PEN has been reported in one case [6]. In this case, after caudal PEN patient had severe headache. A SAH like appearance was observed on his CT scan. In their case they observed catheter malposition into the intradural space at the first attempt. They repositioned the catheter and completed the procedure. In our case, dural puncture was suspected while the catheter was being advanced. Then 1.5-2 ml contrast was given and catheter malposition was determined. The procedure was terminated removing the catheter and needle. In our case, the patient also complained of severe headache too. The results of the experiments show that contrast media are routinely removed directly into the vascular circulation from the cervical subarachnoid space, with no considerable accumulation in the cerebral cisterns [6]. It was not understood how the contrast material mimicking the SAH in brain CT 3 hours after the procedure. Oh et al. thought that this image in their case was caused by the patient's supine position and high blood pressure [6]. Haughton et al. Also evaluated the concentration of cisternal cerebrospinal fluid in monkeys undergoing myelography in the sitting and supine postures. When animals were kept supine, iodine concentrations in the cerebral cisterns were higher than when they were kept sitting [7]. We thought that the patient is in a supine position after the procedure may have an effect on this image too.
Conclusion
This case demonstrates that contrast administered during percutaneous epidural neuroplasty can pass through the dural tear and mimic subarachnoid hemorrhage. Catheter position should be considered during PEN. If malposition is observed, the catheter should be removed. Physicians should be alert to such complications.
References
- Helm S, Knezevic NN. A review of the role of epidural percutaneous neuroplasty. PainManag. 2019; 9(1): 53-62.
- Racz GB, Heavner JE, Trescot A. Percutaneous lysis of epidural adhesions--evidence for safety and efficacy. Pain Pract 2008; 8: 277-286.
- Manchikanti L, Pampati V, Fellows B, Beyer CD, Damron KS, Cash KA. Effectiveness of percutaneous adhesiolysis with hypertonic saline neurolysis in refractory spinal stenosis. Pain Physician 2001; 4: 366-373.
- Cucchiara B, Sinson G, Kasner SE, Chalela JA: Pseudo-subarachnoid hemorrhage: report of three cases and review of the literature. Neurocrit Care 2004; 1: 371-374.
- Eckel T, Breiter SN, Lee HM: Subarachnoid contrast enhancement after spinal angiography mimicking diffuse subarachnoid hemorrhage. Am J Roentgenol 1998; 170: 503-505.
- Oh CH, An SD, Choi SH, Ji GY. Contrast mimicking a subarachnoid hemorrhage after lumbar percutaneous epidural neuroplasty: a case report. Journal of Medical Case Reports 2013; 7: 88.
- Haughton VM, Eldevik OP, Lipman B: Excretion of contrast medium from the lumbar subarachnoid space of monkeys. Radiology 1982; 142: 673-676.

