Percutaneous Transluminal Renal Angioplasty and Nephrectomy as A Mean to Control Treatment Resistant Hypertension and Save Kidney Function
Kristensen K, Youssef MH, Mose FH
Department of Medicine, Gødstrup Hospital, Denmark
Department of Radiology, Gødstrup Hospital, Denmark
Received Date: 28/09/2021; Published Date: 28/10/2021
*Corresponding author: Katrine Kristensen, Department of Medicine, Gødstrup Hospital, Hospitalsparken 35, 7400 Herning, Denmark
Abstract
Renovascular disease is one of the most common causes of secondary- and treatment resistant hypertension and the main cause is atherosclerotic stenosis of the renal artery
This case report is about a woman aged 65 years who presented with treatment resistant hypertension and increasing creatinine levels. Imaging showed renal artery stenosis, and atrophic left kidney. The woman was treated with percutaneous transluminal renal angioplasty to save kidney function. Blood pressure was not manageable on medication, and a nephrectomy was performed on the atrophic kidney.
In severe cases, renovascular hypertension can be treated satisfyingly with antihypertensiv medication, but in cases with progressive kidney failure, and treatment resistant hypertension, invasive procedures can be necessary to save kidney function and reduce the blood pressure.
Keywords: Renovascular hypertension; Percutaneous transluminal renal angioplasty; Nephrectomy; Treatment resistant hypertension
Background
Renovascular disease is one of the most common causes of secondary and treatment resistant hypertension, and the main cause is atherosclerotic stenosis of the renal artery [1].
We present a case story that aims to draw attention to a group of patients with severe renovascular disease, who may benefit from invasive procedure as a means to control blood pressure and preserve renal function.
Case Presentation
A woman, age 65, with known arteriosclerosis, was referred to the department of nephrology with a rapidly declining renal function and resistant hypertension with systolic blood pressure above 200 mmHg despite 5 types of antihypertensive medications (Table 1, Figure 1A). Ultrasound examination showed a normal sized right kidney (11,3 cm) and an atrophic left kidney (7,1 cm), and no signs of obstruction of the urinary tract. Removal of the angiotensin receptor blockers improved plasma creatinine (Figure 1B). CT-angiography of the renal arteries confirmed the suspicion of renal artery stenosis, with completely occluded left renal artery and 90% stenosis on the right side (Figure 2). Renography showed that the left kidney only accounted for 3% of the total kidney function. The woman underwent a successful stenting (Percutaneous transluminal renal angioplasty - PTRA) of the right renal artery. The procedure reduced the blood pressure, but not to an acceptable level, despite intensifying antihypertensiv treatment (Table 1, Figure 1A). Increased plasma levels of renin and aldosterone led to the suspicion of renin producing atrophic left kidney. To improve blood pressure control a nephrectomy rather than PTRA of the atrophic left kidney was performed. The procedure was complicated by in-stent thrombosis in the right renal artery, with the need for re-PTRA and short term dialysis. Two months after nephrectomy and re-PTRA ambulatory blood pressure was well controlled on three antihypertensive drugs, and a stable eGFR of 30 ml/min.
Table 1: Overview of the patient’s medication during the observation period.
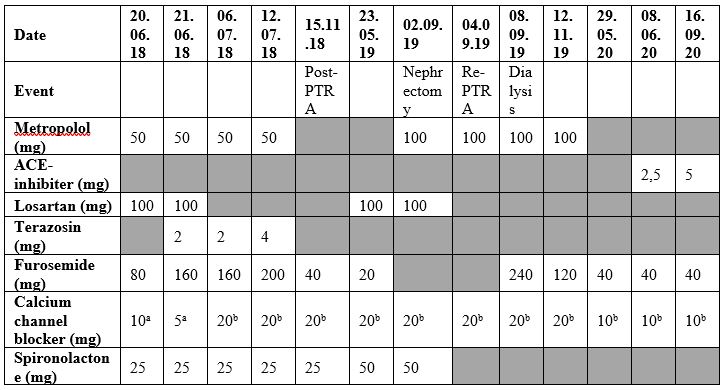
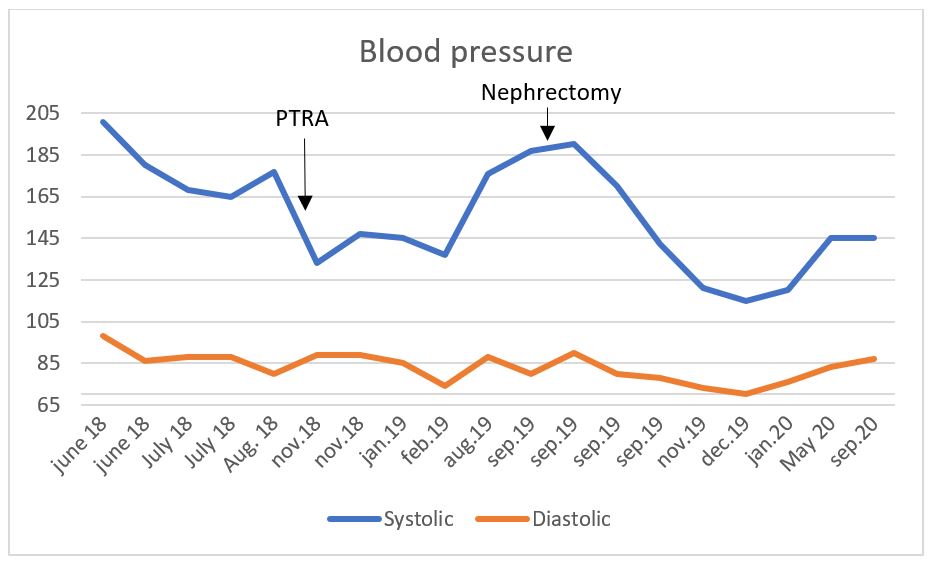
Figure 1A: Overview of the blood pressure.
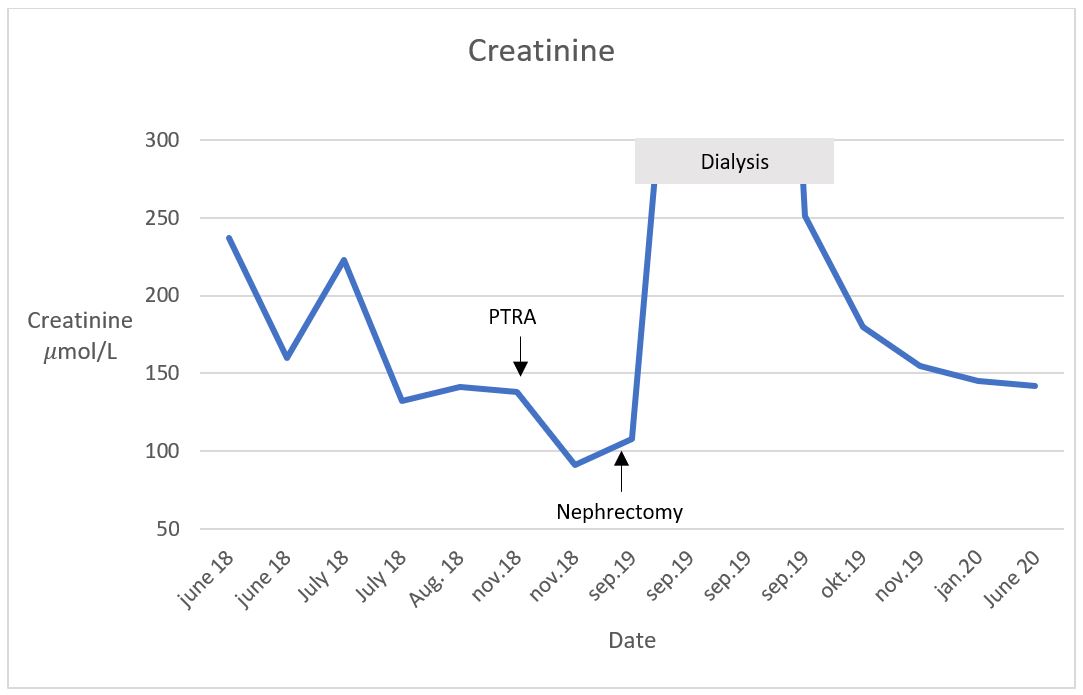
Figure 1B: Creatinine levels.
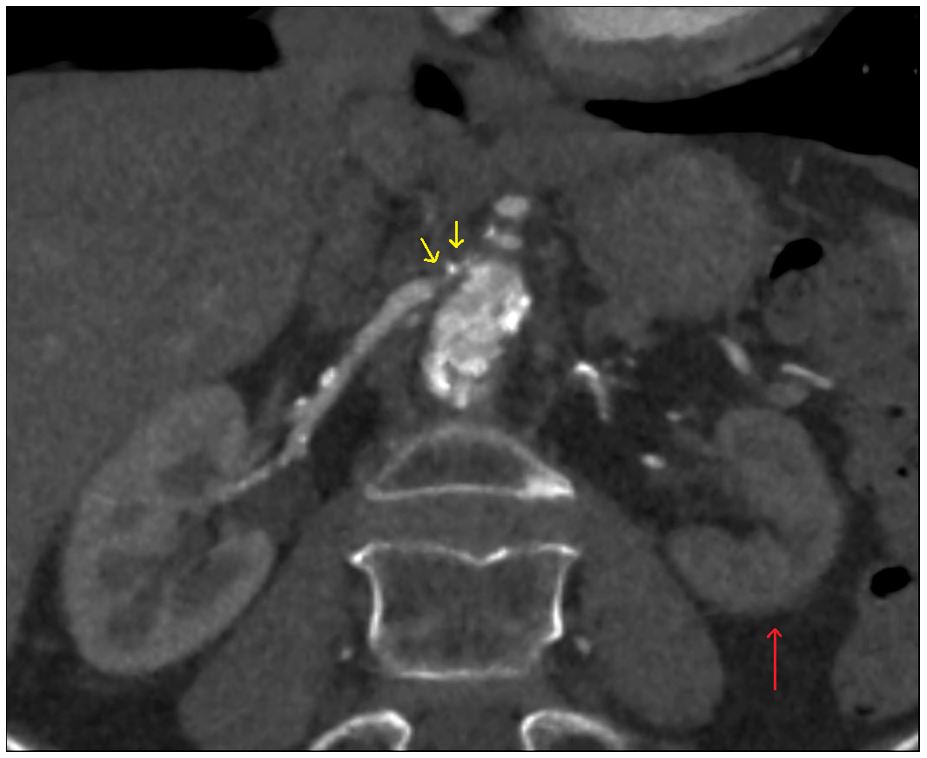
Figure 2: CT-angiography of the kidneys showing atrophic left kidney (red arrow) with sparse blood flow and stenosis of the right renal artery (yellow arrows).
Discussion
Secondary hypertension is rare, but diagnosis is key to prevent progression of organ manifestations of insufficiently treated hypertension, such as cardiac hypertrophy and renal failure. Renal artery stenosis is a common cause of secondary hypertension, with increasing incidence due to increased age [1]. Treatment of renal artery stenosis in treatment of hypertension is debated.
Two recent randomized studies have failed to show benefits of revascularization, as a treatment of renovascular hypertension compared to medical treatment alone [2,3]. The lack of benefit of renal artery stenting, could be explained by the selection of patients in the two trials.
In the ASTRAL study 40 % of the patients had a < 70% stenosis and some even < 50 % stenosis of the renal artery before revascularization [2]. This study only included patients where the referring physician was in doubt of the effect of revascularization.
The CORAL study aimed only to include patients with significant stenosis, but also in this study, the patients assessed most likely to benefit from revascularization were not included [3]. Both studies have a high representation of patients with mild disease, and the patients with severe stenosis, comparable to the woman in this case story, were not considered eligible for inclusion, but were instead referred directly to revascularization.
In this case story the woman was treated with PTRA for her renal artery stenosis with a successful outcome regarding kidney function, and nephrectomy for her renin producing atrophic kidney, with successful blood pressure control. Nephrectomy is a recognized treatment for resistant hypertension, in patients with renovascular disease who have lost renal function and who are unlikely to benefit from revascularization, because of total occlusion of the renal artery or atrophy of the kidney [4]. In our case story none of these parameters were attainable with medical treatment alone.
Treatment of severe renal artery stenoses is based on case series, clinical experience and judgement by treating physicians. Randomized trials of severe renal artery stenosis, compared with a control- or sham group, are not possible to investigate because it is unethical to withhold an organ or lifesaving treatment.
In severe cases, renovascular hypertension can be treated satisfyingly with antihypertensive medication, but in cases with progressive kidney failure, and treatment resistant hypertension, invasive procedures should be considered to save kidney function and reduce blood pressure.
Disclosure and Declarations
Ethics approval and consent to participate: Not relevant for this case story
Consent for publication: The patient has consented to participate in this case story and for publication
Availability of data and materials: Data sharing is not applicable to this case story as no dataset were generated or analysed during the current study
Competing interests: The authors declare that they have no competing interests
Funding: No funding has been received in the production of this case report
Authors’ contributions: KK collected the data, wrote the manuscript and prepared the figures and tables . FHM helped discuss the findings and revise the manuscript. MHY contributed with imaging and revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgements: Not applicable
Disclosure: Authors have nothing to declare.
References
- Herrmann SM, Textor SC. Current concepts in the treatment of renovaskulær hypertension. AM J Hypertens. 2018; 31(2): 139-149.
- ASTAL Investigators, Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, Carr S, Chalmers N, Eadington D, Hamilton G, Lipkin G, Nicholson A, Scoble J. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009;361(20):1953-62
- Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, et al. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014; 370(1): 13-22.
- Kane GC, Textor SC, Schirger A, Garovic VD. Revisiting the role of nephrectomy for advanced renovascular disease. Am J Med 2003; 114: 729-735.

