Finding Their Own Way: Bilateral Ectopic Premolar Teeth that Spontaneously Repositioned during a Course of Jaw Development Orthodontic Therapy: A Case Report and Literature Review
Anne Maree Cole* and Laurence J Walsh
James Street Dentists, Brisbane, Australia
Received Date: 27/09/2021; Published Date: 26/10/2021
*Corresponding author: Dr Anne Maree Cole, James Street Dentists, 151 Robertson Street, Fortitude Valley QLD 4006, Australia.
Abstract
This case report describes a unique situation where bilateral impacted premolar teeth moved spontaneously into the correct 3-dimensional position without orthodontic force, settling into the location predestined for them within the maxilla. The case illustrates the remarkable ability of teeth to “find their way” to a proper 3-dimensional position within the jawbones without any intervention, when freed from the situation of impaction by providing suitable space to give them an eruption pathway. The required space in the maxillary arch was created using a two-fold approach that leveraged bone remodelling processes and the current understanding of bone physiology, with an Anterior Growth Guidance Appliance followed by treatment of the maxillary teeth using the Controlled Archä System protocol. This clinical approach followed the line of argument that “the teeth are not the problem; the jaws are”. The case also illustrates the important principle of treatment being “as much as necessary, but as little as possible”. In this case, surgical exposure and orthodontic traction were able to be avoided, because the genetic template, that evolved physiologically over millions of years, was able to be expressed.
Keywords: Orthodontic Tooth Movement; Bone Modelling; Tooth Eruption
Introduction
Orthodontic treatment is move than simply moving teeth in a 3-dimensional pattern within the jawbones to improve their function and appearance. Some orthodontic treatment modalities can alter growth patterns of the jaw and lower face, and change the shape and dimensions of the jaws, even after the major pubertal growth periods have ended [1,2] When impactions occur, the challenge of bringing the impacted tooth to the correct position may be so great that the tooth is removed. This case report describes a unique situation where bilateral impacted premolar teeth moved spontaneously into the correct 3-dimensional position without orthodontic force, settling into the location predestined for them within the maxilla.
Case Report
A healthy 11-year-old female was referred from an oral and maxillofacial surgeon. She was a mouth breather, with tell-tale gingival inflammation of the maxillary anterior region, but had no other contributing medical or hereditary factors. The patient had a permanent dentition. The second permanent molars (17 and 27) had erupted and were close to being in full occlusion. Premature loss of both deciduous maxillary second molar teeth occurred as a result of the permanent maxillary first molars (16 and 26) having erupted on a mesio-angular path from their normal position, eroding the roots of the deciduous teeth. There was insufficient space for the two maxillary second premolar teeth (15 and 25) to erupt, and both teeth were impacted and in a palatal position. Other than this, the erupted permanent teeth in the maxilla were in normal positions and there was no crowding, nor excess space. A full set of baseline orthodontic records was taken. The baseline situation is shown in Figure 1 (panels A, C, E, G and H) and in Figure 2 panel A.
The patient had previously been assessed by several clinicians. An orthodontist and an oral and maxillofacial surgeon had recommended that both of the impacted premolar teeth be removed surgically. The child’s mother was not comfortable with this approach.
A clinical examination and radiographic evaluation using cone beam volumetric tomography (CBVT) revealed palatal impaction of the maxillary second premolar teeth, lack of space for an eruption path, poor alignment of the crowns of the second premolar teeth, and minimal root formation (Figure 1 panels G and H). The mandible was yawed to the RHS. All other findings were within normal limits.
To enable the development of sufficient bone within the maxillary dental arch to provide space for the impacted teeth, a course of treatment was commenced which was designed to stimulate the maxillary bone to lay down new bone and thus develop space. An upper fixed Osseo-Restorationä appliance, also commonly referred to as an Anterior Growth Guidance Appliance (AGGA) or an Anterior Remodelling Appliance, was fabricated. Interdental separators were placed along with bite guides on the lower molar teeth to correct the rotation and to give a more forward position of the mandible. This would also allow fixed orthodontic treatment of the maxillary and mandibular teeth to be undertaken independently.
The upper fixed appliance was reactivated on a monthly basis, to ensure that sufficient force was being applied. From the first month of treatment, an increase in the arch circumference was seen as new bone was deposited between the maxillary canine and first premolar teeth (Figure 2 panels A to C).
By four months, sufficient bone had developed on each side to allow the later repositioning of the second premolar teeth (Figure 1 panels I and J). At this stage, the AGGA appliance was left in place for one more month, after which time the treatment of the maxillary teeth was changed to the Controlled Arch™ System protocol [3-5]. Molar bands were placed on the first molar teeth, along with a preactivated Fixed Removable Lingual Appliance (FRLA). Metal self-ligating brackets (TP Nu Edge™) were bonded to the teeth. An 020x020 Bio efficient arch wire was placed in the brackets, and set to replicate a Broad-U arch form. This size and shape were maintained and increased by the use of Stop-Locks positioned mesial to the first molar teeth. These Stop-Locks were used throughout the ensuing phases of treatment. Full orthodontic records were taken at this point, and at subsequent treatment steps. These photographic records can be obtained by contacting the first author.
While ample bone had been deposited anterior to the first premolar teeth, to facilitate space for the second premolar teeth, an orthodontic Power chain was used to protract the first premolar teeth. The spring action contained within the activated archwire, secured by the Stop-Locks, ensured that protraction of the premolars occurred. The secured position of the FRLA and Bite Guides (modified Planus Direct Tracks [6]) on the opposing teeth acted as constraints to prevent against the maxillary molar teeth distalizing. This treatment approach also prevented retraction of the anterior teeth.
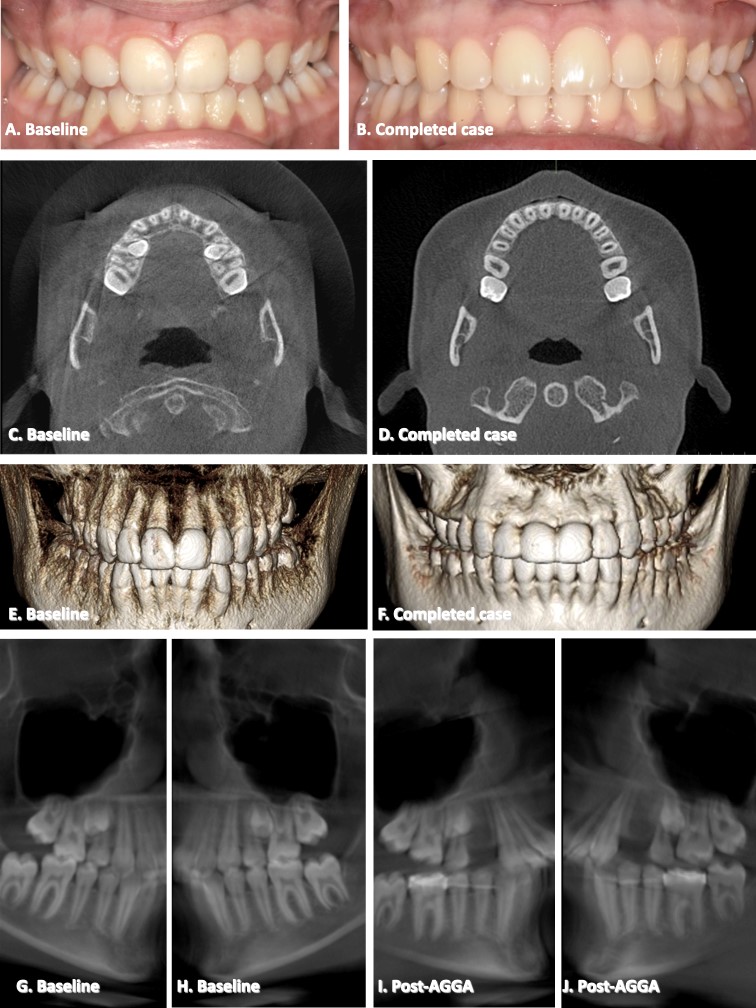
Figure 1: Clinical and radiographic views of the case at baseline (Panels A, C, E, G and H), during treatment (panels I and J), and at completion (panels B, D, and F). Panels A and B are standard anterior views of the dentition; Panels C and D are horizontal slices from cone beam imaging at the same height showing the maxillary arch. Note the impacted teeth present at baseline. There has been an increase in the arch width and arch length due to bone growth during Anterior Growth Guidance Appliance (AGGA) treatment. E and F are 3 dimensional reconstructions from the cone beam data sets. Note the dense labial bone present after treatment. A full orthodontic treatment set of clinical photographs for this case can be obtained by contacting author AMC
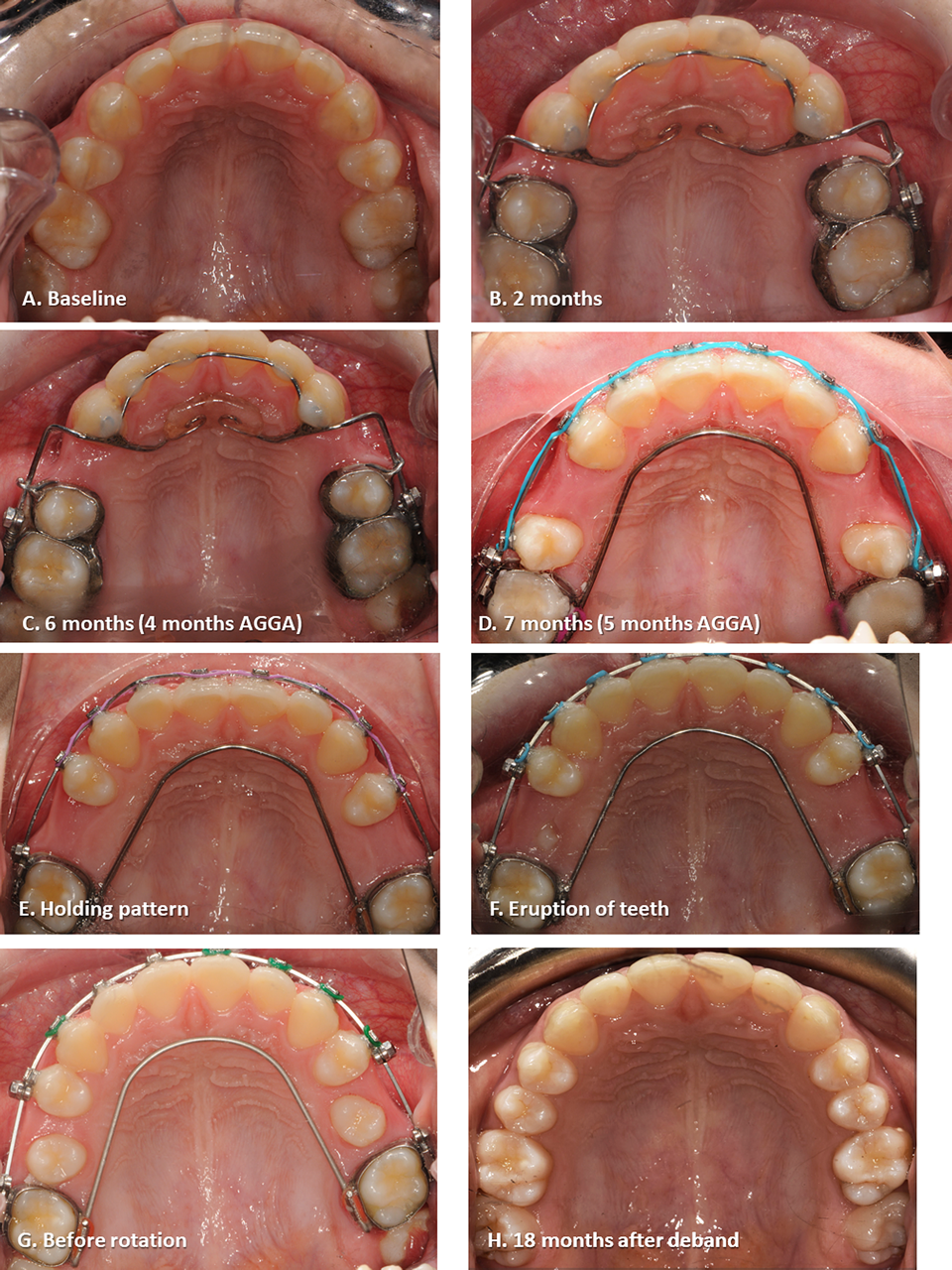
Figure 2: Sequential occlusal arch images of the maxillary dentition, showing the development of maxillary arch length and arch width during treatment. After space had been created by bone growth using Anterior Growth Guidance Appliance (AGGA) (panel E), the impacted premolar teeth erupted spontaneously into the spaces (panels F and G). The completed case at 18 months after debanding is shown in panel H. A full orthodontic treatment set of clinical photographs for this case can be obtained by contacting author AMC.
During the second phase of treatment, the patient was seen every 6 weeks. At each review, the archwire was increased in length by 1 mm bilaterally, and secured again using Stop-Locks. A new Power chain was applied. Over time, the form of the maxillary arch continued to develop. By 5 months, around 10 mm of bone was present on the mesial aspect of the upper first molars on each side, which was more than adequate space for a premolar tooth. At this point in time, it was decided to go into a holding pattern, to wait and see how the body responded to the available space (Figure 2 panel E).
At 10 months, the patient thought a tooth was coming through in the upper left quadrant. Clinical inspection revealed that in the region mesial to the first molar (tooth 26) and within the midpoint of the alveolar ridge, not palatal to it, and the tooth was present just below the surface of the tissue. At the review appointment the following month, the cusp of the second premolar (tooth 25) was emerging, and the same process of eruption was found to be occurring on the right hand side (Figure 2, panel F).
During the ensuing months, both teeth 15 and 25 continued to emerge into their correct position, without any surgical or orthodontic intervention (Figure 2, panel G). Once both teeth had completed their root development, active orthodontic treatment was re-commenced, using the same Controlled ArchÒ treatment approach, until arch size, arch shape and tooth position had optimised, and normal tooth interdigitation between maxillary and mandibular teeth has been achieved. Treatment was completed in 2020. (Figure 1 panels B, D, and F; and Figure 2 panel H).
Discussion
A common situation in dentistry is the early loss of deciduous molar teeth. Early interception prevents the loss of arch length and the predictable consequences of mesial drifting of the permanent molars, such as crowding and impaction of the premolar teeth [7]. However, once the full permanent dentition has erupted, the treatment options for the maxillary arch, which is lacking space for impacted second premolars, are limited.
Ideally, treatment should preserve these teeth and optimize their position within the jawbones. Spontaneous eruption requires that functional space enabling eruption is maintained [8]. In the present case, space was created using orthodontic appliances. These increased the circumference of the dental arch, generating space. This allowed an eruption path for the maxillary premolar teeth, which on their own, found their way into the correct anatomical position, without any external intervention.
The concept of altering bone mass and volume by applying force is not new. In the late 19th century, it was recognised that changing the loads that were applied to bone changed the bony architecture [9]. Understanding the dynamic nature of bone is central to proper clinical practice [10]. Bone is a highly responsive tissue, and its density and shape are influenced by functional demands as well as by the strength and direction of applied forces. Likewise, lack of use and inadequate functional demands, such as from a soft diet and altered oral and nasal functions, including mouth breathing, have epigenetic effects [12,13]. The result is a self-perpetuating cycle where poor form continues to support the aberrant function [14].
For the jawbones, heritable traits and functional environmental influences provide a platform or canvas, upon which can be crafted an improved form. The concepts of altering the jawbones by stimulating growth and remodelling are relevant to patients with cranio-facial deficiencies [15], temporo-mandibular disorders, malocclusions and sleep-disordered breathing [1,16,17] By targeting the hard tissues that have failed to develop to their full genetic potential, the possibility exists to rectify the cranio-facial anatomy or redirect it back towards normal [18].
Bone remodelling occurs throughout life as old bone is replaced by new bone [19]. Normally, the volume, shape and position of bone remain unchanged, despite this remodelling. However, an increased load will lead to a net gain, as was achieved in the present case through the use of two different orthodontic appliances. Bone can respond to applied force because osteocytes have efficient pressure detectors and mechanoreceptors, and can initiate the cascade of events associated with bone remodelling [20]. The first stimulus to intramembraneous bone formation provided in the current case was the Anterior Growth Guidance Appliance, while the second was during the Controlled Arch™ orthodontic technique.
The physiological sequence of active bone remodelling is always the same: activation, resorption, reversal, bone deposition, (collagen matrix formation, hydroxyapatite deposition and mineralization) and quiescence. The bone deposition phase is the longest in duration, and complete mineralization may take more than 12 months to complete [21]. The remodelling process proceeds smoothly, as long as the overlying periosteum is not disturbed [19,22]. In the present case, the lack of surgical intervention meant that no injury to the periosteum occurred. This maximized the bone forming potential. This explains why there was dense bone on the buccal and labial aspects of the maxillary teeth at the end of treatment (Figure 1 panel F).
Bone deposition and remodelling not only occurs during orthodontic treatment, but extend beyond the completion of active treatment. There is risk of misdiagnosis of the situation of bone remodelling when using radiographs, as they will only detect highly mineralized bone. Other diagnostic methods, including medical ultrasound, and optical coherence tomography, do not suffer from this limitation as they can image the early stages of bone formation when only osteoid is present. They reveal what is happening in the tissues, are non-invasive, and do not pose a risk to patients, unlike ionizing radiation [23-25]. Future studies should use such non-invasive high resolution imaging methods to track changes in bony structures during remodelling.
Conclusion
The present case illustrates the remarkable ability of teeth to “find their way” to a proper position when freed from the situation of impaction and provided with suitable space to give them an eruption pathway. The required space in the arch was created using a two-fold approach that leveraged bone remodelling processes and the current understanding of bone physiology. This follows the line of argument that “the teeth are not the problem; the jaws are”. The case also illustrates the important principle of treatment being “as much as necessary, but as little as possible”. In this case, surgical exposure and orthodontic traction as well as the option of extraction were able to be avoided, because the genetic template, that evolved physiologically over millions of years, was able to be expressed.
Authors’ Contributions:
AMC and LJW wrote the paper, AMC provided data; LJW prepared the figures, AMC and LJW revised the manuscript. All authors read and approved the final manuscript. AMC is the guarantor of this manuscript
Compliances with Ethical Standards:
The authors declare that they have no conflicts of interest.
There was no funding for this project.
Informed consent was obtained from the participant included in this report for publication of this report and the accompanying images
References
- Hang WM, Gelb M. Airway Centric® TMJ philosophy/Airway Centric® orthodontics ushers in the post-retraction world of orthodontics. Cranio 2017; 35(2): 68-78.
- Adams O, Griffiths R, Hoff A. Craniofascial structure. Struct Integr. 2012; 40(2): 14-19.
- Sim JM, Galella SA. The controlled arch system: a new method of straightwire treatment. J Gen Orthod. 1999; 10(4): 9-15.
- Sim JM, Galella SA. The controlled arch system: a new method of straightwire treatment for adolescents and young adults (Part II). J Gen Orthod. 2000; 11(1): 9-28.
- Galella SA. ControlledArch Flow Sheet: The Facial Beauty Institute; Collierville, TN, USA 2016.
- Ramirez-Yañez GO. Planas direct tracks for early crossbite correction. J Clin Orthod. 2003; 37(6): 294-298.
- Hafiz ZZ. Ectopic eruption of the maxillary first permanent molar: a review and case report. J Dent Health Oral Disord Ther. 2018; 9(2): 154-158.
- Andrade I, Paschoal MAB, Santos TO. Spontaneous eruption of severely impacted teeth: the report of two cases. J Clin Exp Dent. 2019;11(5): e491-5.
- Frost HM. A 2003 update of bone physiology and Wolff's Law for clinicians. Angle Orthod. 2004; 74(1): 3-15.
- Hill PA. Bone remodelling. Brit J Orthod, 1998; 25(2): 101-7.
- Carlson DS: Growth modification: from molecules to mandibles. In: McNamara JA (ed): Growth Modification: What Works, What Doesn’t, and Why. Craniofacial Growth Series 35, Ann Arbor, Center for Human Growth and Development, The University of Michigan, 1999; pp. 17-62.
- Kahn S, Ehrlich P, Feldman M, Sapolsky R, Wong S. The jaw epidemic: Recognition, origins, cures, and prevention. BioScience 2020; 70(9): 759-771.
- Harari D, Redlich M, Miri S, Hamud T, Gross M. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. Laryngoscope 2010; 120(10): 2089-2093.
- Chaitow L, Bradley D, Gilbert C. Recognizing and treating breathing disorders. A multidisciplinary approach. 2nd edn. Edinburgh: Elsevier Health Sciences; 2014; pp. 23-59.
- Mao JJ, Nah HD. Growth and development: hereditary and mechanical modulations. Am J Orthodont Dentofac Orthop. 2004; 125(6): 676-689.
- Racich MJ. Occlusion, temporomandibular disorders, and orofacial pain: An evidence-based overview and update with recommendations. J Prosthet Dent, 2018; 120(5): 678-685.
- Grant R. Condylar adaptation following mandibular repositioning. Int J Orthod (Milwaukee, Wis.), 2004; 15(4): 27-32.
- Bromage T. Will the knowledge of the biology of facial growth have any impact on your clinical results for your family of patients? International Association of Orthodontics Annual Meeting. Tucson, Arizona 2016.
- Mostafa HKK. Structure and function of periosteum with special reference to its clinical application. Egypt J Histol. 2019; 42(1): 1-9.
- Cowin SC, Moss-Salentijn L, Moss ML. Candidates for the mechanosensory system in bone. J Biomech Eng. 1991; 113(2): 191-197.
- Allen MR, Burr DB. Bone modeling and remodeling. In: Burr DB, Allen MR (eds) Basic and applied bone biology, 2nd Edn: New York, Elsevier; 2019; p. 85-100.
- Giannobile WV, Berglundh T, Al‐Nawas B, et al. Biological factors involved in alveolar bone regeneration: Consensus report of Working Group 1 of the 15th European Workshop on Periodontology on Bone Regeneration. J Clin Periodont. 2019; 46(21): 6-11.
- Laugier P. Quantitative ultrasound instrumentation for bone in vivo characterization. In: Laugier P, Haïat G. Bone quantitative ultrasound: Dordrecht, Springer; 2011; pp. 47-71.
- Yamato Y, Matsukawa M, Yanagitani T, Yamazaki K, Mizukawa H, Nagano A. Correlation between hydroxyapatite crystallite orientation and ultrasonic wave velocities in bovine cortical bone. Calcif Tiss Int 2008; 82(2): 162-169.
- Wilder-Smith P, Otis L, Zhang J, Chen Z. Dental OCT. In: Drexler W, Fujimoto JG. Optical coherence tomography: technology and applications, 2nd edn. Cham, Switzerland: Springer International, 2015; pp. 2209-44.

