Anomalous Origin and Path of Right Coronary Artery in a Middle-Aged Patient: A Case Report and Review of Literature
Faid S*, Mesfioui MB, Amina Samih, Britel Driss, Zakaria Lahlafi, Feliouni Hicham, Oussama Ait Kejjate, Ballouk Ramiz, Lakhal Zouhair
Intensive care unit of Mohamed V training military hospital of Rabat, Morrocco
Received Date: 06/09/2021; Published Date: 28/09/2021
*Corresponding author: Mohammed Bachir Mesfioui, Intensive care unit of Mohamed V training military hospital of Rabat, Morrocco
Abstract
Coronary Artery Anomalies (CAAs) are rare but potentially life threating abnormalities of coronary circulation. Most of them are benign; however, some may lead to severe myocardial ischemia or even sudden cardiac arrest.
We report a case of a middle-aged female who presented with angina to exercise and cardio-vascular explorations have led to diagnosis of an anomaly of birth of the right coronary artery; patient was treated medically in addition to hard exercise restriction, with good outcome during the follow-up.
Only the exact definition of the anatomic and clinical features of CAAs may allow to choose the most appropriate and effective treatment. Computed tomography may play a fundamental role in the diagnosis and treatment of CAAs.
Introduction
Coronary artery anomalies (CAAs) are diagnosed incidentally in 1.3% of cases on angiography and cardiac computed tomography (CT) [1-2]. These very rare findings present with diverse clinical manifestations in patients ranging from asymptomatic incidental findings to profound ischemia and sudden cardiac death[3]. The methods used to evaluate CAAs include echocardiography, angiography and new non-invasive methods such as coronary computed tomography (CT) and cardiac magnetic resonance imaging (MRI). The management strategy may vary based on clinical data, anatomical details and additional findings[4].
Case Presentation
A 38-year-old Caucasian female was admitted to our cardiology department for exploration of a typical angina. She had no relevant cardiovascular history and reported since last year the beginning of chest pain with blockpnea, occurring especially with emotional situations and exertion, upon walking upstairs.
The ECG performed on admission, as well as the biological workup, were normal. Echocardiography showed normal-sized chambers with preserved ejection fraction and no wall motion abnormalities. However, the diagnosis of CAA was suggested on echocardiography by a Right Coronary Artery (RCA) that was believed to originate from the left coronary sinus.
Exercise ECG was performed and patient couldn’t reach theoretical maximum heart rate according to her age; the result was litigious and inconclusive on ischemic level.
Subsequently, a coronary angiogram was performed, which did not reveal any significant stenosis but noted poor visualization of the right coronary artery due to its abnormal origin. For further evaluation, she underwent cardiac Computed Tomography (CT) which showed birth defect of the right coronary artery (Figure 1) which originates from the left sinus of Valsalva with an intraarterial course between the aorta and the pulmonary artery (Figure 2).
Because of the patient’s complex coronary anatomy, we avoided intervention and prescribed medical therapy with beta-blockers and recommended limitation of hard exercise, with outpatient monitoring. She was doing well one year later.
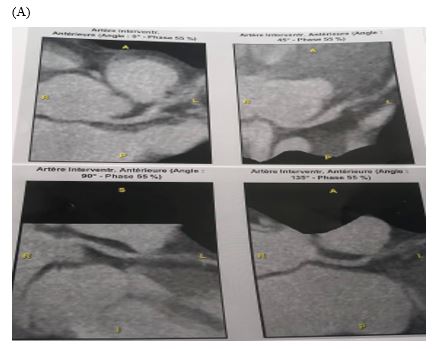

Figure 1: CT coronary artery showing through different incidences and angles, the origin of the anterior descending coronary artery (A) and the anomalous origin of right coronary artery (B) which arise from the left anterior sinus with an inter-arterial path between the aorta and the pulmonary artery.
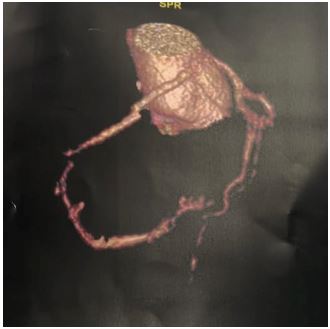
Figure 2: frontal view of a three-dimensional reconstruction of CT coronary artery, demonstrating arterial paths with the anomalous origin of right coronary artery arising from the left coronary sinus as the left anterior descending coronary artery.
Discussion
The prevalence of CAAs is close to 0.5% with coronary angiography and 1% with coronary CT [5]. The circumflex artery is the most involved (50% of cases) versus 30% for the RCA and 20% for the left main and the left anterior descending artery (LAD) [6].
The position between the aorta and the pulmonary artery puts the coronary arteries at risk for compression particularly during strenuous activity and may significantly limit the reservoir capacity of the epicardial coronary system [7]. In addition, the angulation of coronary artery at its origin from the opposite sinus causes an acute closure in its ostium responsible for the symptoms especially during hard activities [8].
The clinical presentation can include angina or equivalent, lipothymia, syncope, heart failure, documented myocardial ischemia, severe ventricular rhythm disturbances (tachycardia or fibrillation), recovered cardiac arrest and sudden death. Yet coronary anomalies may also be asymptomatic.
Adults are not well suited for coronary analysis by transthoracic echocardiogram. Only the first few millimeters of an ectopic coronary artery can be visualized and precise diagnosis cannot be made on ultrasound imaging alone.
Frequently involved in the diagnosis in adults, coronary angiography is no longer considered the gold standard for classifying CAA. It does not allow sufficient analysis of the ectopic orifice and the initial pathway.
Coronary CT has become the reference examination when a risky form is suspected or when an initial ectopic path is uncertain. CT is particularly useful in determining the path of the ectopic vessel.
Cardiac MRI has the advantage of not using contrast agents and is non-irradiating. However, because of its low spatial resolution, this technique is currently less helpful in evaluating the distal coronary system [9,10].
CAAs with an intraarterial pathway and/or intramural connection, and those with a pulmonary connection are the recognized CAAs at risk [11].
The course of action is often difficult in adults for CAAs at risk. Several decision algorithms have been proposed [12,13].
Practices are quite heterogeneous, explained by still limited knowledge on the natural or corrected history of CAAs [14,15].
The benefit/risk ratio of surgical correction has not yet been clearly evaluated. In cases of recovered cardiac arrest or symptomatic left-sided CAA, the indication for correction is clear. The current lack of a score stratifying individual risk of sudden death complicates management [16]. The same anatomic shape may be responsible for early sudden death or be perfectly tolerated until old age.
If myocardial ischemia is the main mechanism of symptoms, the place of coronary angioplasty deserves to be evaluated in adults where placing a stent seems possible without major risk.
Empirically, a beta-blocker treatment can be proposed in case of ischemic symptomatology. Monitoring alone may be an acceptable initial strategy depending on the context.
Given the current state of knowledge and uncertainty, it seems preferable that the decision to correct or not to correct a CAA be made by a specialized multidisciplinary team. There are recommendations to this effect [17].
Conclusion
CAAs are rare congenital heart disease with variable clinical presentation. Their management and choice of therapy are controversial and depend especially on the variant of anomalous coronary artery and the symptoms. The role of Heart Team in such cases is highly recommended.
References
- Laureti JM, Singh K, Blankenship J. “Anomalous coronary arteries: A familial clustering,” Cardiol., 2005; 28(10): pp. 488-490. doi: 10.1002/clc.4960281009.
- Yamanaka O, Hobbs RE. “Coronary artery anomalies in 126,595 patients undergoing coronary arteriography,” Cardiovasc. Diagn., 1990; 21(1): pp. 28-40. doi: 10.1002/ccd.1810210110.
- Medepalli LC, Medepalli VM, Scully TA. “The complementary nature of multimodal imaging in the management of an anomalous aortic origin of the right coronary artery from the left coronary cusp,” Nucl. Cardiol., 2020. doi: 10.1007/s12350-020-02209-x.
- Yurtdaş M, Gülen O. “Anomalous origin of the right coronary artery from the left anterior descending artery: Review of the literature,” J., 2012; 19(2): pp. 122-129. doi: 10.5603/CJ.2012.0023.
- Aubry P, Halna du Fretay X, Calvert PA, et al. Proximal anomalous connections of coronary arteries in adults. In: Rao P.S., ed. Congenital heart disease selected aspects. Intech; 2012.
- Aubry P, Halna du Fretay X, Dupouy P, et al. Anomalous connections of the coronary arteries: a prospective observational cohort of 472 adults. The ANOCOR registry. Eur Heart J. 2015; 36(suppl 1): 1138.
- Louis IB. Coronary artery anomalies. 2019.
- Anomalous origination of right coronary artery from left sinus in asymptomatic young male presenting with positive ischemic response on treadmill test.
- McConnell MV, Stuber M, Maning WJ. Clinical role of coronary magnetic resonance angiography in the diagnosis of anomalous coronary arteries. J Cardiovasc Magn Reson, 2000; 2: 217-224.
- ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus docu- ment on cardiovascular magnetic resonance: A report of the American College of Cardiology Foundation Task Force on Ex- pert Consensus Documents. Circulation, 2010; 121: 2462–2508.
- Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 73: e81- e192.
- Driesen BW, Warmerdam EG, Sieswerda GT, et al. Anomalous coronary artery originating from the opposite sinus of Valsalva (ACAOS), fractional flow reserve- and intravascular ultrasound-guided management in adult patients. Catheter Cardiovasc Interv. 2018; 92: 68–75.
- Mery CM, Lawrence SM, Khrisnamurthy R, et al. Anomalous aortic origin of a coronary artery: toward a standardized approach. Semin Thoracic Surg. 2014; 26: 110-122.
- Brothers J, Gaynor J, Paridon S, Lorber R, Jacobs M. Anomalous aortic origin of a coronary artery with an arterial course: understanding current management strategies in children and young adults. Pediatr Cardiol. 2009; 30: 911–921.
- Agrawal H, Mery CM, Day PE, et al. Current practices are variable in the evaluation and management of patients with anomalous aortic origin of a coronary artery: results of a survey. Congenit Heart Dis. 2017; 12: 610-614.
- Mirchandani S, Phoon CKL. Management of anomalous coronary arteries from the contralateral sinus. Int J Cardiol. 2005; 102: 383-389.
- Brothers J.A. Introduction to anomalous aortic origin of a coronary artery. Congenit Heart Dis. 2017; 12: 600-602.

