Advances in Minimally Invasive Surgery for Excision of a Large Substernal Goiter During the Sars-Cov-2 Pandemic
Draeger TB1, Tse A1, Namburi D2, Housman B3, Datta RV4, Andaz SK5,*, Gibson VR6
1Department of Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
2Department of Surgery, MS3 Ross University School of Medicine
3Department of Surgery, Division of Cardiothoracic Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
4Chairman, Department of Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
5Director, Division of Cardiothoracic Surgery, Department of Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
6Director of Thoracic Surgical Oncology, Division of Cardiothoracic Surgery, Department of Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
Received Date: 03/09/2021; Published Date: 27/09/2021
*Corresponding author: Andaz SK, M.D. Director, Division of Cardiothoracic Surgery, Department of Surgery, Icahn School of Medicine at Mount Sinai, Mount Sinai South Nassau
Abstract
Patients with mediastinal masses often have compressive symptoms requiring urgent surgical resection. The SARS-CoV-2 pandemic has drastically affected availability of critical care and surgical beds and radically altered the ability to perform elective, urgent, and emergent surgical cases, disproportionately impacting small intuitions and community hospitals. The standard approaches used in the resection of mediastinal masses via median sternotomy can result in prolonged hospital stays and utilization of critical care beds. For this reason, utilizing less invasive procedures are of great importance during these unprecedented times. This is a case of a 62-year-old female who presented with dysphagia progressing to aphagia, due to a mediastinal mass. The Intuitive Xi Surgical Robot was used to respect the mass bypassing the complications that can arise with the standard approaches and reducing the need for a critical care bed or prolonged admission in the setting of the SARS-CoV-2 pandemic.
Keywords: Goiter; Substernal; Mediastinal; Robot; SARS-CoV-2
Introduction
The novel Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) was identified in early 2020 and since has wreaked havoc across the globe. During the peak 12 weeks of the SARS-CoV-2 pandemic, there were an estimated 28 million cancelled surgical operations worldwide with approximately 4.5 million cases cancelled in North America alone [1]. One of the major factors affecting elective surgeries was the need for post-operative inpatient beds, including critical care beds which at the time had extremely limited availability. For this reason, shortening hospital admissions and increasing bed availability had been a priority, thus requiring alternative approaches to elective, urgent, or emergent surgical procedures.
Mediastinal masses can present in a multitude of ways, ranging from asymptomatic to causing severe mass effect resulting in dysphagia, dyspnea, and vascular compression [2]. Typically, mediastinal goiters are removed via a transcervical approach when possible however a cervical approach is not always surgically feasible and, in some cases, can be dangerous when the ectopic thyroid tissue presents with an alternative blood supply requiring a more invasive approach and prolonged hospital admission [3].
Case Presentation
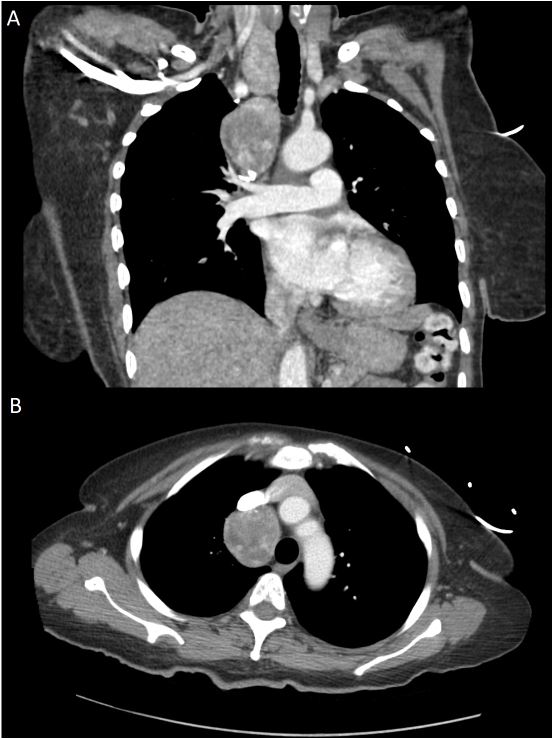
This is a case of a 62-year-old female who presented to our institution with a 3-month history of dysphagia, and a 4-day history of aphagia, lethargy, and weight loss. She had previously delayed care due to the SARS-CoV-2 crisis but given the complete inability to tolerate oral intake, she required inpatient admission and nutritional supplementation. Her history was significant for a previous left hemithyroidectomy for indeterminant thyroid nodules. Computed Axial Tomography (CT) scan demonstrated a right paratracheal mass measuring 5.4x4.5x4.1cm (Figure 1). Biopsy was performed, which was consistent with ectopic thyroid tissue. Given the current pandemic, the patient was scheduled for a cervical thyroidectomy and a robotic thoracoscopic excision of the mediastinal component, which we believed would have the best chance of keeping the patient from requiring a critical care bed and would result in the shortest length of stay for her admission, thereby reserving these limited resources for SARS-CoV-2 patients.
The procedure was initiated with the cervical thyroidectomy which began with division of the right superior pole close to the thyroid to protect the superior laryngeal nerve. Then the middle thyroid vein was ligated, and the lower pole was then dissected and divided. The parathyroid glands were identified and preserved, after which, the right thyroid lobe was rotated medially. Subsequently, using a nerve monitor, the recurrent laryngeal nerve was identified and traced, and the gland was dissected away from the trachea.
The patient was then placed in the left lateral decubitus position, and a thoracoscopy incision was made in the posterior axillary line at the 8th intercostal space. Thoracoscopy revealed the mass was in the thoracic inlet near the superior sulcus, anterior to the trachea, adjacent to the superior vena cava. Additional access ports were then placed strategically in the thorax. The Intuitive Xi Surgical Robot (Intuitive Surgical, Inc., 1020 Kifer Road, Sunnyvale, CA, USA) was then docked. The lung was then rotated inferiorly to expose the superior mediastinum. The pleura overlying the mass was opened which continued across the superior apex of the chest extending down the posterior mediastinum to the level of the azygos. The phrenic nerve was identified and avoided throughout the procedure.
The mass was in contact with the inferior vena cava, subclavian artery and vein, and azygous. The azygos vein was mobilized with blunt dissection at its insertion at the superior vena cava, and then was ligated and divided using a vascular stapler. Dissection continued in the superior mediastinum mobilizing the mass off the superior vena cava and freeing it superiorly to the level of the subclavian vein. Stay sutures were placed in the pleura overlying the mass for traction purposes. The mass was rotated anteriorly to expose the posterior mediastinum, and blunt dissection mobilized the mass off the anterior surface of the trachea extending up into the thoracic inlet. Thyroidal vessels were identified and divided via a bipolar vessel sealing device. Once the mass was able to be completely mobilized off the mediastinum, it was extracted and sent for inspection by the pathology team. A frozen section was confirmed to be consistent with a substernal thyroid goiter. The chest cavity was irrigated, and hemostasis was achieved. The lung was inflated under direct visualization and the patient was then returned to supine position, awoken from anesthesia, extubated, and taken to recovery room in a stable condition.
Histopathologic examination of the specimens was consistent with a multinodular goiter and revealed the cervical component was 21g measuring 5.1x4.7x2.2cm with multiple well-circumscribed nodules measuring up to 1.2cm in diameter and the mediastinal component was 47g measuring 6.5x4.7x3.1cm with multiple nodules measuring up to 1.1cm in diameter.
The post-operative period was uneventful, and the patient was discharged on the third post- operative day. She did not require a critical care bed during her admission.
Discussion
In addition to the restrictions on elective cases, as a result of the pandemic, significantly less patients have sought medical care in general during the pandemic. Those requiring urgent or emergent care have also avoided hospitals and healthcare facilities resulting in delayed presentation and treatment of medical emergencies [[i]]. Our patient, who had been suffering from dysphagia did not seek medical treatment until she had been unable to tolerate any oral intake for several days requiring admission to the hospital and a medical bed for management of her malnutrition.
Median sternotomies are generally required if a goiter extends below the aortic arch, large thyroid tissue extends towards tracheal bifurcation, or there is ectopic thyroid tissue in the mediastinum [2]. Although median sternotomies provide many benefits in the resection of these masses, they are inherently more invasive, and are associated with more post-operative complications [2-3]. About 0.2-3 percent of post-sternotomy patients develop mediastinitis and sternal wound infection, and dehiscence has been reported in approximately 0.5-8.4% of sternotomies [4-5]. Due to the limitations demonstrated by the transcervical approach and the morbidity of the median sternotomy, minimally invasive techniques have emerged.
Minimally invasive robotic procedures have transformed the surgical field and are being used in a variety of surgical specialties. Robotic procedures have the advantage of better visualization by providing stereoscopic vision as well as greater dexterity and precision due to the increased degrees of freedom provided by the robotic arms. They have been shown to result in shorter post-operative hospital stays, shorter duration of chest drains, lower intraoperative blood loss, and lower peri-operative complications in comparison to sternotomies [4]
Average length of stay for an open sternotomy when performed for resection of mediastinal masses has been reported as averaging 5.53 days with similarly matched patients undergoing robotic resection of mediastinal masses averaging 2.65 days, saving approximately 3 hospital days [[v]]. In our patient, having performed the less invasive robotic resection of her mediastinal mass the length of stay was on par with that which has been reported. As a result, greater bed availability was maintained for admissions of SARS-CoV-2 patients. In addition, whilst sternotomy patients spend at least one night in critical care at our institution, this scarce resource was preserved for SARS-CoV-2 patients, having avoided a median sternotomy in our patient.
Conclusion
In this patient we have demonstrated that the modern approach for the surgical removal of mediastinal masses using the Da Vinci surgical robot provides many benefits over a traditional sternotomy including decreased length of stay, thus preserving both critical care and medical/surgical hospital beds. In the time of the SARS-CoV-2 pandemic, this approach was critical in preserving limited resources necessary to serve the ever-expanding population of SARS-CoV-2 patients.
Author Contributions: All authors contributed to the writing and reviewing of this manuscript
Competing interests: The Authors declare there are no competing interests
Grant Information: No grants were obtained, nor was any additional funding furnished
References
- Negopdiev D, Collaborative C, Hoste E. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. British Journal of Surgery. 2020; 107(11): 1440-1449.
- Coskun A, Yildirim M, Erkan N. Substernal goiter: when is a sternotomy required? International surgery. 2014; 99(4): 419-425.
- Houck WV, Kaplan AJ, Reed CE, Cole DJ. Intrathoracic aberrant thyroid: identification critical for appropriate operative approach. The American surgeon. 1998; 64(4): 360.
- Hecht N, Wessels L, Werft FO, Schneider UC, Czabanka M, Vajkoczy P. Need for ensuring care for neuro-emergencies—lessons learned from the COVID-19 pandemic. Acta Neurochirurgica. 2020;1.
- To H, Karmakar A, Farrell S, Manolas S. Trans-cervical resection of a separate substernal goiter. International journal of surgery case reports. 2017; 41: 373-376.
- Hakim A, Sather C, Naik T, McKenna Jr RJ, Kamangar N. Masses of the Anterior mediastinum. Medical Management of the Thoracic Surgery Patient E-Book: Expert Consult-Online and Print. 2009; 32: 365.
- Huang W, Jiang GN. Resection of giant mediastinal liposarcoma via ‘⊣ shape’ incision. Journal of surgical case reports. 2017; 2017(1): rjw219.
- Seong YW, Kang CH, Choi JW, Kim HS, Jeon JH, Park IK, et al. Early clinical outcomes of robot-assisted surgery for anterior mediastinal mass: its superiority over a conventional sternotomy approach evaluated by propensity score matching. European Journal of Cardio-Thoracic Surgery. 2014; 45(3): e68-73.

