Arterial Thoracic Outlet Syndrome: An Overlooked Cause of Arm Pain
Hajar Adil*, Khadija Laasri, Jamal El Fenni, Issam En-Nafaa
Department of Radiology, Mohammed V Military Teaching Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Received Date: 24/08/2021; Published Date: 21/09/2021
*Corresponding author: Hajar Adil, Department of Radiology, Mohammed V Military Teaching Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Abstract
Arterial thoracic outlet syndrome is a rare variant of thoracic outlet syndrome that describes arterial dynamic compression of the upper extremity arterial vessels, passing through the thoracic outlet, secondary to congenital or acquired narrowing of its spaces. This article describes the case of a young female who presented with long-standing ischemic symptoms of the right arm. ATOS diagnosis was established on a clinical and imaging basis and the patient underwent surgery with a satisfying postoperative outcome.
Keywords: Arterial thoracic outlet syndrome; ATOS; Scalenus anticus syndrome; Cervical rib
Abbreviations: ATOS- Arterial Thoracic Outlet Syndrome; CT- Computerized Tomography; TOS- Thoracic Outlet Syndrome; CTA- CT angiography; MRI- Magnetic Resonance Imaging; VTOS- veinous thoracic outlet syndrome
Case Report
A-26-years old female presented with right arm weakness and numbness associated with cold sensation and pale right hand, induced by repetitive arm movements especially after typing for a long period or lifting things above the head level. The patient was prescribed symptomatic treatment for a long time before she was referred to a vascular surgeon. Physical examination revealed positive abduction maneuvers on the right side the symptoms appeared at 90° abduction and worsened at 180° elevation. CT angiography showed narrowing of the right subclavian artery, which was impinged, above the clavicle, between the anterior and medial scalene muscles. In addition, CT examination demonstrated a mild post-stenotic dilatation associated with bilateral cervical ribs (Figures 1-4). No collateral vessels were noted and the left subclavian artery showed no anomalies. Arterial decompression was then indicated and the patient underwent surgery that consisted of resection of the cervical rib together with anterior scalenectomy as it was noted intraoperatively that the scalene muscle was compressing the subclavian artery. The postoperative ultrasound showed normal pulse waves in the right arm. The postoperative course was unremarkable.
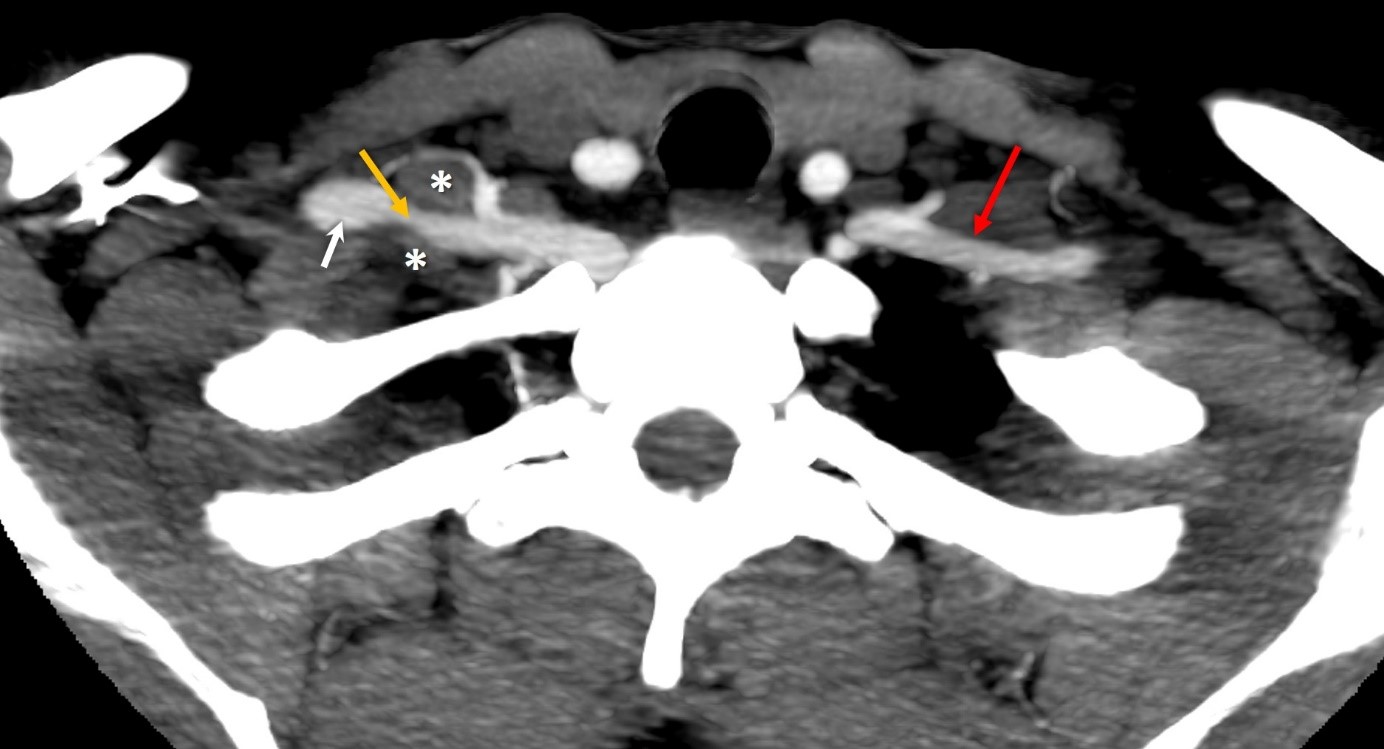
Figure 1: 26-years old female with right ATOS. Findings: axial contrast enhanced CT of the cervico-thoracic region in the arterial phase demonstrating narrowing of the right subclavian artery (yellow arrow) which is impinged between the anterior and medial scalene muscles (asterix). Note the post-stenotic dilatation marked by the white arrow. The red arrow shows the normal aspect of the left subclavian artery. CT: Siemens, 120 kV, 250 mAs, 5 mm slices, Ultravist 150 cc.
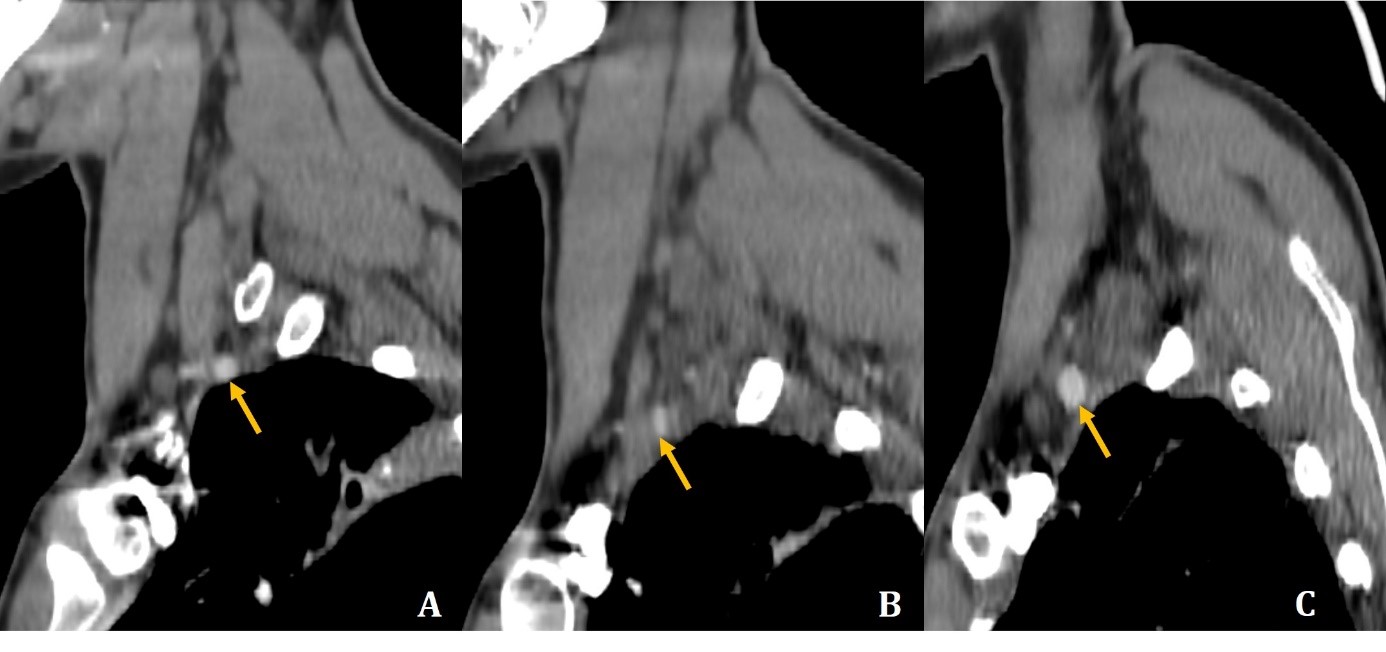
Figure 2: 26-years old female with right ATOS. Findings: sagittal contrast enhanced CT of the cervico-thoracic region in the arterial phase demonstrating normal caliber of the right subclavian artery (A), the narrowing of the impinged arterial segment (B), and the post-stenotic dilatation (C). CT: Siemens, 120 kV, 250 mAs, 5 mm slices, Ultravist 150 cc.
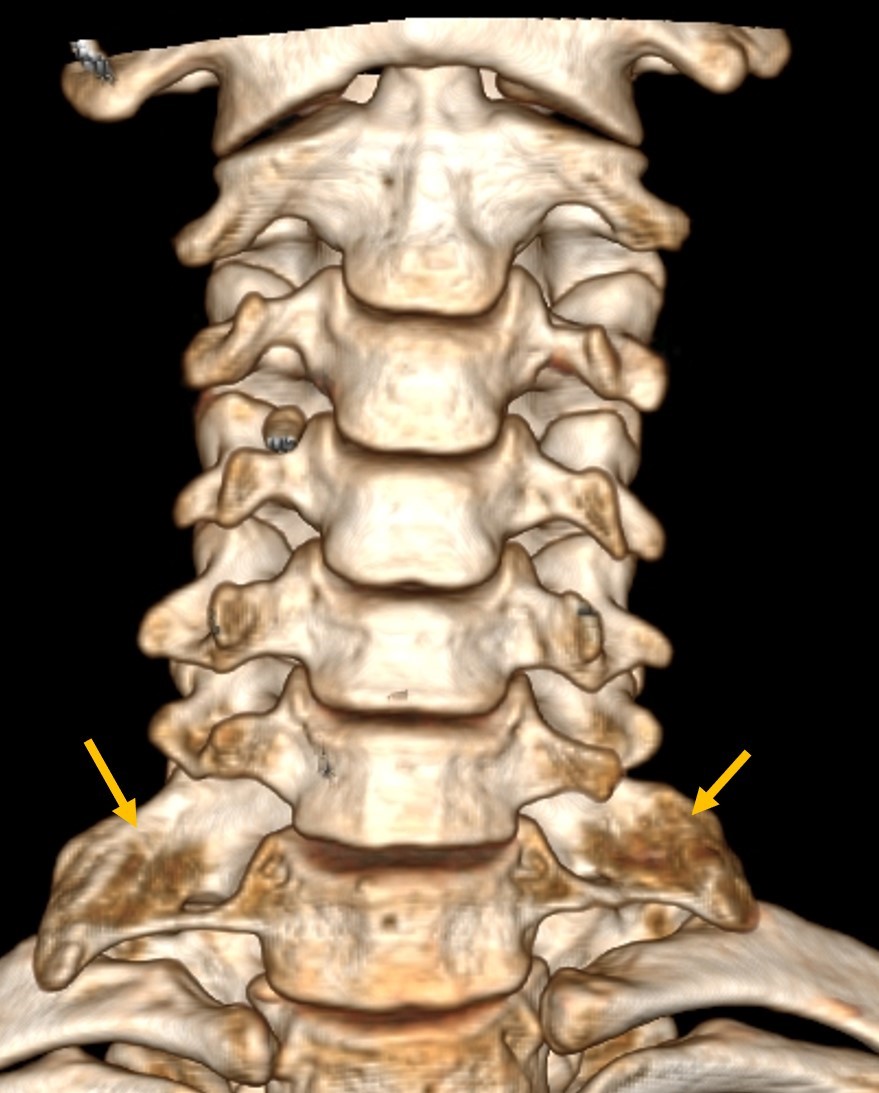
Figure 3: 26-years old female with right ATOS. Findings: 3D CT Volume rendering images of the cervical spine, showing bilateral cervical ribs. CT: Siemens, 120 kV, 250 mAs.
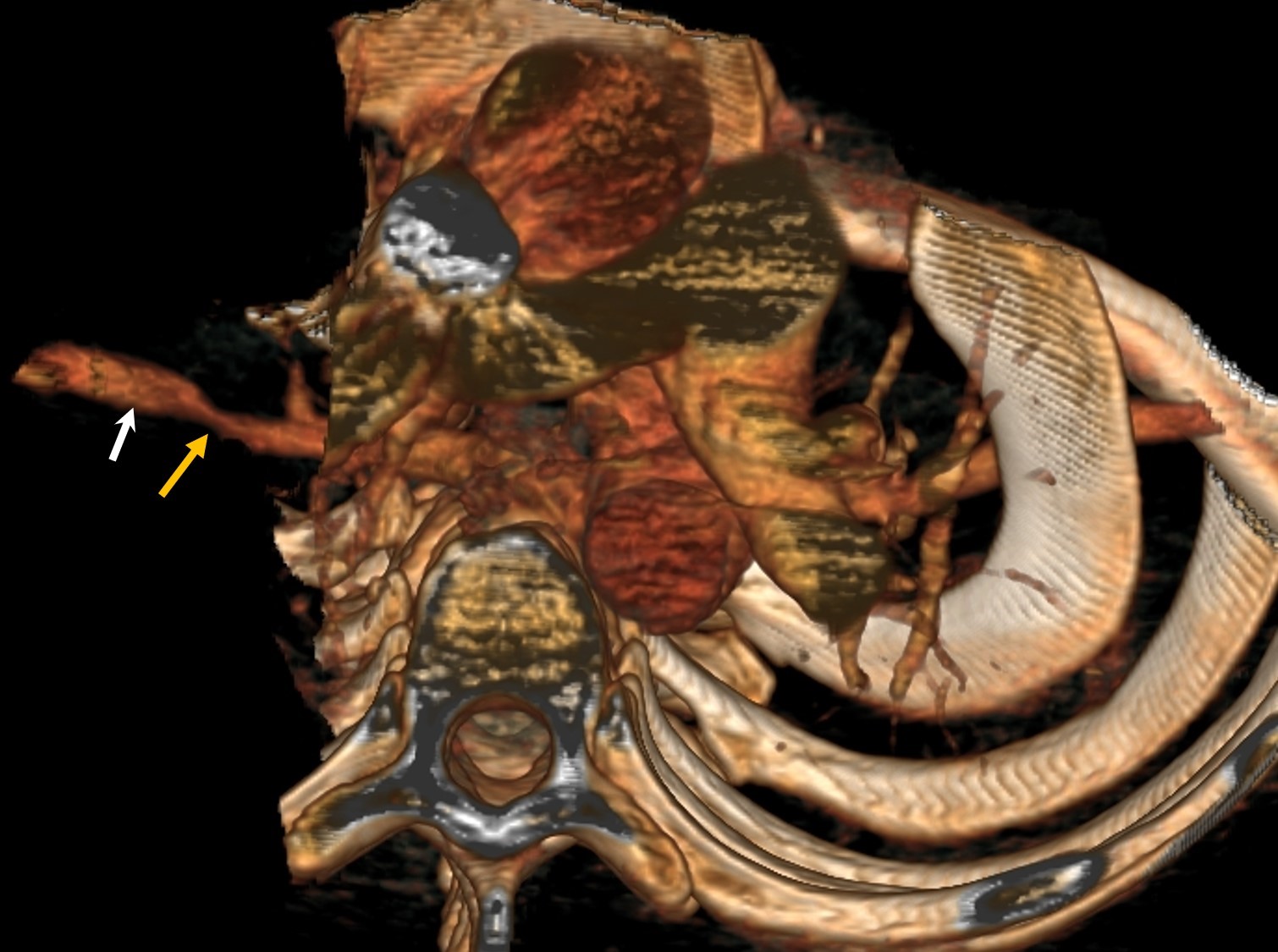
Figure 4: 26-years old female with right ATOS. Findings: 3D contrast enhanced CT Volume rendering images (inferior view) showing the narrowing of the right sub-clavian artery (yellow arrow) and the post-stenotic dilatation (white arrow). CT: Siemens, 120 kV, 250 mAs, Ultravist 150 cc.
Discussion
The term thoracic outlet syndrome (TOS) was first described by Peet et al in 1956 to indicate dynamic compression of the neurovascular bundles of the upper extremity, passing through the thoracic outlet, secondary to congenital or acquired narrowing of its spaces [1]. The most commonly involved age category for this syndrome is 20–40 years, with a predilection for female patients [2]. TOS mainly involves the brachial plexus (more than 90% of cases). Veinous involvement is less common, it was reported in 5% of patients, whereas arterial compression is rare, as it’s described only in 1% of patients [3].
Subclavian artery impingement above the clavicle level occurs in the interscalene triangle which is the most medial of the three thoracic outlet compartments. It represents the space through which the roots and trunks of the brachial plexus and the subclavian artery exit the neck area, which is bounded by the scalenus anterior muscle anteriorly, by the scalenus medius muscle posteriorly, and by the first rib inferiorly [2]. ATOS is due to a cervical rib in nearly 50% of cases, followed by soft tissue anomalies in one-third of patients and scar tissue after clavicle fracture in 5% of cases. Chronic compression and trauma to the subclavian artery may result in intimal ulceration, stenosis with post-stenotic dilatation, or aneurysmal degeneration. Distal emboli can arise after a thrombus migration from the site of the damaged intima [4].
ATOS typically manifests with weakness, cold, pallor, cyanosis, and hypersensitivity. Symptoms may be insidious until an acute thrombosis and/or embolus occurs and causes severe arterial insufficiency that presents with pain, coldness, digital ulcers, or even gangrene [3]. Clinical diagnosis is based on reproducing compression symptoms using dynamic maneuvers, such as lateral and anterior abduction of the arm [5]. However, it is often difficult; therefore, the use of imaging modalities is required to demonstrate vascular compression and to determine the nature and location of the structure undergoing compression and the cause of the impinging [2].
Plain Radiography of both the cervical spine and chest can effectively outline bony anomalies that may aid in the diagnosis of TOS such as cervical ribs, elongated C7 transverse process, degenerative spine disease, or bone destruction [2].
Ultrasonography has the advantage of being low-cost and noninvasive. It offers the possibility of analyzing the blood flow while performing the compression maneuvers. B-mode scanning detects anatomic abnormalities such as stenosis, mural thrombus, thrombotic obstruction, and aneurysmal dilatation. Color duplex sonographic examination associated with postural maneuvers may demonstrate abnormalities not present at rest, such as loss of bi-directional flow, diminution of normal phasicity, complete flow cessation, or increase of blood flow velocity through the narrowing. Unfortunately, this technique does not allow an accurate overview of the thoracic outlet region nor an analysis of the region of the pulmonary apex, hence it should always be performed complementary to other techniques [2,3,6].
CT Angiography (CTA) is performed after intravenous administration of iodinated contrast agent, first with the arms alongside the body and then with the arms raised above the head to reproduce the vascular compression, and help assess the narrowing of the various compartments. CT reformatted images of data obtained both in the neutral position and after postural maneuvers help characterize the arterial compression, indicate its location, and assess its severity. Also, volume-rendered images of the thoracic outlet before and after postural maneuvers allow simultaneous analysis of osseous and vascular structures with excellent spatial resolution. However, CTA exposes to ionizing radiation and is limited by the fact that the acquisition is done in a supine position, whereas the symptoms occur when the patient is upright [2,3].
MRI is a noninvasive and nonionizing technique. Sagittal and coronal T1-weighted images are especially helpful in depicting vascular compression. Arterial irregularity or obstruction may be detected by simply analyzing the caliber of the vessel along its course. However, comparing the images obtained with the arm in a neutral position and after arm elevation offers a better assessment of vessel compression. Also, thanks to its excellent soft-tissue contrast, MR imaging helps to depict muscle hypertrophy, abnormal muscles, and fibrous bands [2].
Conventional arteriography offers the advantage of demonstrating the entire vascular anatomy from shoulder to fingertips. It can be performed with dynamic maneuvers and offers the possibility of performing therapeutic procedures at the same time if indicated. However, it is an invasive procedure that does not allow a clear depiction of the impinging anatomic structure [2,3].
Differential diagnosis of ATOS includes venous TOS, Raynaud phenomenon, subclavian artery aneurysm, and subclavian steal syndrome.
Management of ATOS includes three steps; removing the cause of arterial compression by excising the abnormal bony structure or the compressing muscle, repairing or replacing the artery, and restoring distal circulation [7].
Conclusion
Although being rare, arterial compression is the most threatening form of TOS, as it compromises the viability of the upper limb, hence, a prompt and accurate diagnosis should be established for an adequate treatment. Clinical diagnosis is often insufficient; as physical symptoms may be insidious and hard to reproduce. Therefore, imaging modalities play a key role in demonstrating vascular compression and characterizing the nature and location of the impinging structures.
References
- Peet Robert M. "Thoracic outlet syndrome: evaluation of a therapeutic exercise program." In Proc Mayo Clin, 1956; 31: pp. 281-287. PMID: 13323047.
- Demondion Xavier, Pascal Herbinet, Serge Van Sint Jan, Nathalie Boutry, Christophe Chantelot, Anne Cotten. "Imaging assessment of thoracic outlet syndrome Imaging assessment of thoracic outlet syndrome." Radiographics 2006; 26(6): 1735-1750. PMID: 17102047.
- Sanders Richard J, Stephen J Annest. "Thoracic outlet and pectoralis minor syndromes." In Seminars in vascular surgery, 2014; 27(2): pp. 86-117. WB Saunders. PMID: 25868762.
- Qaja Erion, Sara Honari, Robert Rhee. "Arterial thoracic outlet syndrome secondary to hypertrophy of the anterior scalene muscle." Journal of surgical case reports 2017; 8: rjx158. PMID: 28928918.
- Molina J Ernesto, Jonathan D’Cunha. "The vascular component in neurogenic-arterial thoracic outlet syndrome." The International journal of angiology: official publication of the International College of Angiology, Inc, 2008; 17(2): 83. PMID: 22477393.
- Adam Garret, Kevin Wang, Christopher J Demaree, Jenny S Jiang, Mathew Cheung, Carlos F. Bechara. "A prospective evaluation of duplex ultrasound for thoracic outlet syndrome in high-performance musicians playing bowed string instruments." Diagnostics 2018; 8(1): 11. PMID: 29370085.
- Hooper Troy L, Jeff Denton, Michael K McGalliard, Jean-Michel Brismée, Phillip S. Sizer Jr. "Thoracic outlet syndrome: a controversial clinical condition. Part 2: non-surgical and surgical management." Journal of Manual & Manipulative Therapy 2010; 18(3): 132-138. PMID: 21886423.

