Cerebral Abscesses Complicating Tetralogy of Fallot in a 20-Year-Old Patient: About A Case and Literature Review
Sayarh Salma*, Bouazaze Marouane, Harmouch Hicham, Amri Rachida and Cherti Mohammed
Internal Medicine, Ibn Sina Hospital of Rabat, Mohammed V University of Rabat, Morocco
Received Date: 24/08/2021; Published Date: 16/09/2021
*Corresponding author: Sayarh Salma, Department of Medicine, University Mohamed V of Rabat, Morocco
Summary
Tetralogy of Fallot is the most common cyanogenic congenital heart disease with an incidence of 1/10,000 birth whose complications are potentially serious, ranging from hyper cyanosis attacks to cerebrovascular events.
Brain abscess is a relatively unusual but potentially fatal infection of the cerebral parenchyma, which can occur in about 5-18.7% of the population with congenital heart disease. A number of theories have been put forward to explain why congenital heart disease is so closely associated with brain abscesses.
Here we discuss a case of corrected Tetralogy of Fallot presenting as brain abscesses of right temporal localization in a 20-year-old patient. The patient was conservatively managed with intravenous antibiotics and then referred for a development and surgical management of her congenital heart disease to cardiovascular surgeons.
Brain abscesses are a complication of cyanogenic heart disease whose outcome is fatal in the absence of adequate management, hence the interest of early diagnosis and management of these heart diseases.
Introduction
The so-called paradoxical brain abscess appearing as a complication of congenital heart disease has been the subject of particular attention in the medical literature over the last century.
This is a relatively unusual but potentially fatal infection of the cerebral parenchyma, which can occur in about 5-18.7% of the population with congenital heart disease [1,2], the tetralogy of Fallot is the most concerned CC in this context. This classic complication is the consequence of the polycythemia observed in these patients, responsible for a blood hyper viscosity, favoring stasis that constitutes an area conducive to the development of septic embolisms [3].
Tetralogy of Fallot is the most common cyanogenic congenital heart disease with an incidence of 1/10,000 birth, it is defined by a wide interventricular communication (IVC), an aorta straddling the CIV, an obstruction on the hunting route of the right ventricle (VD), sub valvular, valvular, or supravalvular, and a right ventricular hypertrophy. It can be fraught with life-threatening complications, ranging from hyper cyanosis attacks to cerebrovascular events. Infectious neurological complications are well known, but their prevalence has decreased significantly in developed countries, thanks to early diagnosis and rapid surgical correction of congenital cardiaque malformation.
Clinical Case
A 20-year-old patient admitted to the medical resuscitation department and then transferred to internal medicine at Ibn Sina Hospital in Rabat, complaining of shortness of breath, high fever, headache and vomiting in jet with impaired general condition. The malade was diagnosed with a tetralogy of Fallot at the age of 02 years having undergone no surgical correction due to financial constraints. It also reports a notion of dyspnea since childhood, palpitations and generalized weakness.
The general physical examination found a conscious patient, dyspneic saturating 83% in the ambient air, her temperature was 38 ° C, her pulse has 100 beats / minute; and a blood pressure of 110/75 mmHg with the presence of a digital hippocratism.
No peripheral signs of infectious endocarditis were found.
The cardiovascular examination, objectified a systolic breath at the left sternal edge rated 4 / 6th, and the rest of the examination was without peculiarities.
The patient was neurologically well oriented but had an IMD motor deficit. The rest of the exams were within normal limits.
Biology found hemoglobin at 15 g / dl and hematocrit at 49%, white blood cells and a high CRP level, having decreased significantly after administration of ATB.
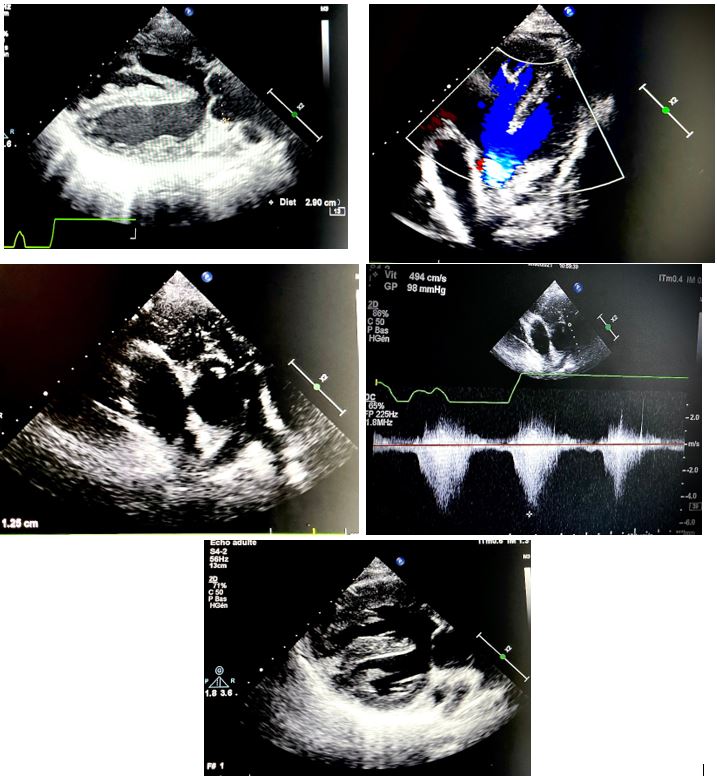
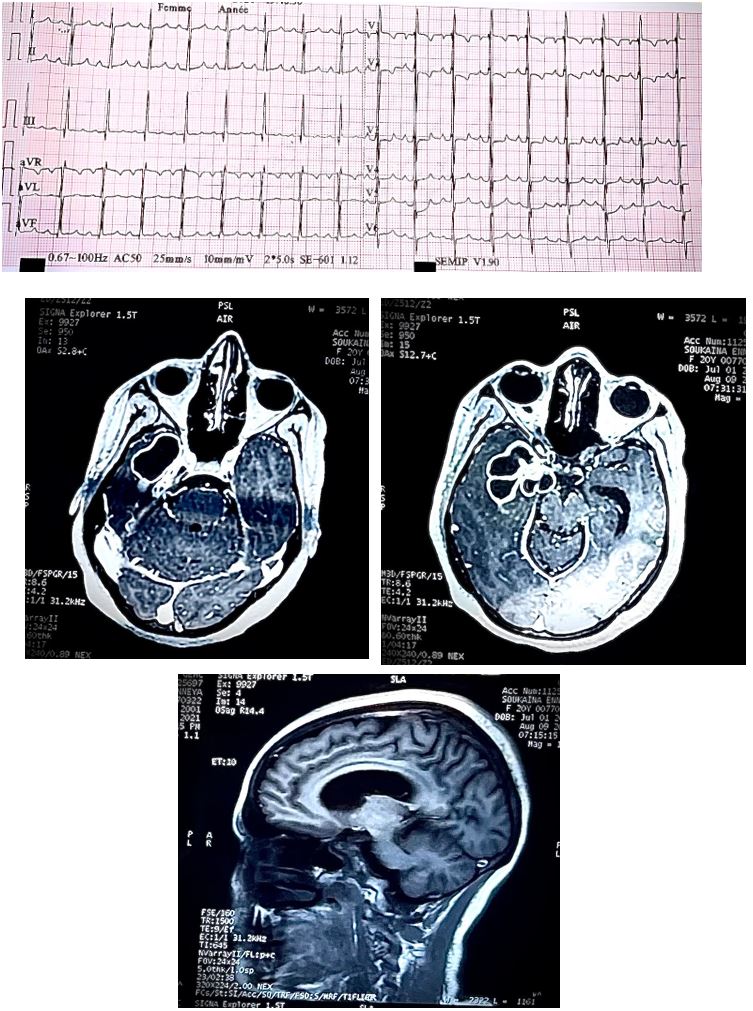
A brain scan was carried out objectifying a cerebral process making suspect a cerebral abscess with engagement, prompting to be completed by a brain MRI revealing the presence of brain abscesses of right temporal localization associated with a ventriculitis complicated by aseptic thrombosis of the right transverse sinus. Cardiac Doppler ultrasound had shown a non-restrictive conoventruclar CIV with a med septal trabeculated micro shunt, a dilated extraposed aorta, infundibular pulmonary stenosis with valvaire and annular participation and a frankly hypertrophied VD, without signs suggesting infectious endocarditis.
The patient was treated conservatively with intravenous antibiotics and showed a marked improvement in her symptoms within three days of treatment a new brain scan was done after two weeks objectified a regression in the size of brain abscesses.
The patient was presented for cardiovascular surgery for possible surgical correction of her congenital cardiopathy.
Discussion
Cyanogenic congenital heart disease is a predisposing factor for the occurrence of brain abscesses, their incidence in these patients varies from 5 to 18.7%, and tetralogy of Fallot is the C.C most concerned in this context [4].
This malformation was previously described by the Marseilles Fallot in 1888, under the name of "tetralogy", and which is fundamentally due to a single anatomical anomaly, namely the forward and right displacement of the infundibular septum, which leads to an uneven partition of the right and left hunting routes. This results in narrowing of the pulmonary pathway, interventricular communication by misalignment, and overlapping of the aortic orifice [5-8]. To this anatomical definition must be added another, physiological one, i.e., the equalization of pressures in the two ventricles and the existence of an exclusive or predominant right-left shunt.
A distinction is usually made between tetralogies of Fallot of classic form which are said to be regular and those of atypical form which are said to be irregular. These last forms correspond to the combination of other malformations which can also compromise surgical repair: abnormalities of the coronary arteries in 5% of cases [9];with in particular the particular case of the right coronary which crosses the anterior face of the hunting chamber of the right ventricle; Multiple CIVs; VD-AP obstacle that may confine to pulmonary aristos is; as well as anomalies of the pulmonary arteries (PA): abnormality in number (e.g. single PA), size abnormality (uni or bilateral or hypoplastic stenosis) or birth defect. The following heart defects are also frequently associated with tetralogy of Fallot: atrial communication, multiple muscular interventricular communications, a right aortic arch in 25% of cases [10], bacterial canal still permeable in less than in less than 10% of cases [11]. Most often the Fallot’s tetralogy is isolated, but sometimes it can integrate into syndromes such as trisomy 21, microdeletion syndrome 22q1.1, bike-cardio-facial syndrome and Goldenhar syndrome.
The regular form is most often asymptomatic at biotreating a clinical picture often called "Pink Fallot". The initial presentation varies, of course, depending on the severity of the obstruction of the pulmonary pathway. Clinically only a systolic Mormon, usually 2-3/6 at the pulmonary focus, can evoke the diagnosis. The first months of life often go quite well, with good food tolerance and good weight gain. This situation may persist until the first operating time or may gradually evolve towards cyanosis corresponding to the clinical form called "Blue Fallot".
The child with a "Blue Fallot" whether from birth or after a slow evolution from an initially pink form, presents a Right-Left shunt through the CIV which enters slowly progressive cyanosis (central cyanosis that affects both mucous membranes and integuments and increases with effort and crying). Cyanosis, if respected, is then accompanied by a digital hippocratism that develops gradually over many months with a deformation of the corners that curve and an enlargement of the phalangists. In these patients, there is also a frequent squatting attitude called squatting, patients instinctively tend to adopt this genu-pectoral position to fight against hypoxia that occurs after exercise. This allows an increase in venous return and an increase in abdominal pressure favoring the recovery of the left-right shunt.' Fallot's discomfort or hypoxic malaise is more common in blue forms that have a pulmonary obstacle more important the discomforts are favored by moments of agitation or dehydration. They are characterized by acute and complete obstruction of the subpulmonic ejection pathway in general to exertion.
There is a sudden and obvious drop in oxygen saturation. The systolic murmur disappears on auscultation, which testifies to a closure of the infundibulum which more or less completely interrupts the passage of blood through the pulmonary arteries and accentuates the passage of desaturated blood to the aorta. Patients are severely cyanosed, polypneic and if the malaise continues rapidly hypotonic. With the development of metabolic acidosis, a vicious circle is created by promoting an increase in pulmonary vascular resistance and a decrease in systemic vascular resistance, which compromises cardiac output promoting loss of consciousness and can sometimes lead to death.
Once the diagnosis is made, a cardiac ultrasound is performed quickly to confirm the diagnosis but also to assess the severity of the sub pulmonary obstruction, its dynamic component (saber blade appearance), the size of the right and left pulmonary arteries, the degree of dextroposition of the aorta, the size of the interventricular communication, as well as the presence of other associated lesions such as abnormal positioning of the coronaries which should modify the surgical technique.
The rx thorax shows a boot-shaped heart with a concave pulmonary arterial arch and a decrease in pulmonary vascularization. A butt of the right aorta is present in 25% of cases.
The Electrocardiogram (ECG) will show severe VD hypertrophy with wide and ample QRS complexes in V1-V2, an aspect qR or an exclusive R wave in V1 and a transition zone generally incalculable a right axis or a hyper droit axis, a completely right block is common and, in this case, R' is much wider than R, repolarization can reveal signs of right ventricular overload, atrial arrhythmias or rillette disease is common during evolution.
Cardiac catheterization is now rarely necessary due to the high sensitivity and specificity of echocardiography but retains all its value for irregular forms mainly when stenosis of the pulmonary arteries or abnormal implantation of the coronaries is suspected. The latter is an invasive examination and for this reason the cardiac scanner is replacing it because of its effectiveness in the exploration of extracardiac structures.
Diagnosed late or non-treated they can become complicated. Depending on the type of heart disease, it can be: heart failure, infectious endocarditis, severe polycythemia, stroke or brain abscess.
The cerebral abscess in particular is a collection of pus in the cerebral parenchyma. It is a classic complication of C.C cyanogen’s, described since 1814, the most important risk factor in the development of abscess is polycythemia. They are more common in the parietal lobe followed by the frontal and temporal lobes, multilocular abscesses are quite common too.
The clinical picture is dominated by febrile convulsions, headache and vomiting. The diagnosis is confirmed by the crania encephalic scanner.
A number of different theories have been put forward to explain why congenital heart disease is so closely associated with brain abscesses. Some authors postulate that due to the right-left shunt, venous blood passes into the arterial system without being filtered through the pulmonary circulation, where bacteria are intercepted by phagocytes [13,14,15,16,17]. It is also thought that the brain itself may be predisposed to offer a focus of infection as a result of halomalacia encep secondary to embolism or polycythemia. Germs can then be seeded in this infarcted area, forming a brain abscess [13,17].
Berthrong and Sabiston [l] stressed the importance of polycythemia in the production of intravascular thrombosis leading to infarction. Possible sources of embolus are the formation of thrombus in a peripheral vein, giving rise to a paradoxical embolus, as well as the formation of thrombus in a cardiac chamber. Bacterial endocarditis can also give rise to embolisms [12,13,14,15,17]. The delay in the diagnosis and subsequent management of brain abscesses in patients with CCHD leaves the underlying condition untreated for some time to complicate the disease process. Mortality in untreated patients ranges from 27.5% to 71% [1].
Larger or deeper abscesses should be sucked in immediately and repeatedly. After aspiration, the patient should begin appropriate antibiotic therapy specifically targeting the organism discovered in culture. Empirical medical therapy is an exclusive treatment for cases where the size of the abscess is less than 2 cm in diameter, the patient is neurologically stable and monitored by repeated CT scans [4,18].
Treatment is medical (antibiotic therapy) and / or surgical (by puncture drainage). Prevention requires the completion of the complete cure of congenital heart disease.
Conclusion
Early diagnosis of Congenital Heart Disease (C.C) has a positive impact on their course. Indeed, diagnosed late or untreated they can be complicated,
Brain abscess is a formidable and potentially serious infection that is still a challenge for the medical world despite the introduction of updated radiological diagnostic procedures, a newer and more effective antibiotic regimen and better neurosurgical techniques.
A corrective surgical cure for these heart defects would be a definitive way to prevent this disaster.
References
- Pandian JD, Moosa NV, Cherian PJ, Radhakrishnan K. Brainstem abscess complicating tetralogy of Fallot successfully treated with antibiotics alone. Neurol India 2000; 48: 272–275.
- Sethi S, Kapil Scalp block for brain abscess drainage in a patient with uncorrected tetralogy of Fallot. World J Clin Cases 2014; 2: 934-937. http://dx. doi.org/10.12998/wjcc.v2.i12.934.
- Sadoh W E, Ikechukwu N A. Cerebral abcess in uncorrected tetralogy of Ann Biomed Sci. 2012; 11(1): 25–28.
- Yves N'da Kouakou N'goran, Micesse Tano, Fatoumata Traore, Inès Angoran, N'guetta Roland, Aké Evelyne Traboulsi, et al. Brain abscess complicating congenital heart disease: about 7 cases at the Abidjan Heart Institute.
- Bartelings MM, Gittenberger-De-Groot Morphogenetic considerations on congenital malformations of the outflow tract. Int J Cardiol 1991; 32: 213-230. Part 1: Common arterial trunk and tetralogy of Fallot.
- Becker AE, Anderson RH. Pathology of congenital heart disease. London: Butterworth; 1991; 1–91.
- Binet JP, Hvass U, Bruniaux J, Langlois J, Planche C, Dreyfus G, et al. Complete correction of the tetralogy of Fallot without opening of the right ventricle. Arch Mal Coeur 1980; 73:1185-1192.
- Bove EL, Byrum CJ, Thomas FD, Kavey RE, Sondheimer HM, Blackman MS, et al. The influence of pulmonary insuffi- ciency on ventricular function following repair of tetralogy of J Thorac Cardiovasc Surg 1983; 85: 691–696.
- Bonnemains L, Mandry D, Marie PY, Micard E, Chen B, Vuissoz Assessment of right ventricle volumes and function by cardiac MRI: quantification of the regional and global interobserver variability. Magn Reson Med. 2012; 67: 1740-1746.
- Optimal timing for pulmonary valve replacement in adults after tetralogy of Fallot Am J Cardiol. 2005; 95:779-782.
- Dodge-Khatami A, Büchel EV, Knirsch W, Kadner A, Rousson V, Dave HH, Bauersfeld U, Prêtre RBrain natriuretic peptide and magnetic resonance imaging in tetralogy with right ventricular dilatation. Ann Thorac 2006; 82: 983-988.
- Berthrong M, and Sabiston DC Cerebral lesion in congenital heart disease. A review of autopsies on 162 cases. Bul1 Johns Hopkins Hosp 1951; 89: 384.
- Brandt M, et al. Bram abscess in children with congenital heart disease. Adv Neurosurg 1981; 9: 86.
- Fischbein CA, et al. Risk factors for abscess in patients with congenital heart disease. Am J Cardiol 1974; 34: 97.
- Kagawa M, et al Bram abscess in congenital cyanotic heart dis- case. J Neurosurg 1983; 58: 913.
- Newton Haematogenous bram abscess in cyanotic congenital heart disease. Q J Med 1956; 25: 201.
- Shaher RM, Deuchar DC. Hematogenous brain in cyanotic con- genital heart disease. Am J Med 1972; 52: 349.
- Ashraf M, Ahmed S, Ahmad S, Hussain M. Burr hole aspiration of brain abscess in children with cyanotic heart disease. J Coll Physicians Surg Pak 2017; 27: 483-485.

