Pediatric Tele Dentistry During Covid-19 Pandemic: A Case Report
Claudia Salerno*
Department of Pediatrics, University of Milan, Italy
Received Date: 03/08/2021; Published Date: 30/08/2021
*Corresponding author: Claudia Salerno, Department of Paediatrics, University of Milan, Italy
Abstract
During the COVID-19 pandemic peaks in Italy, as in other countries, most dental treatments were postponed, except for emergencies, and many private dental offices closed. This situation led many patients, with non-urgent oral problems, to enlist the help of mobile dental consultations by sending pictures or videos to their dentist or physician. This approach to diagnose and “treat” oral problems is called tele dentistry, method already validated in literature. The aim of this case-report is to present a diagnosis of an unconventional oral candidiasis case in a 9 years old child through tele dentistry. This case report shows how social platforms and modern technology have made possible to solve the case. High resolution pictures, even if at an amateur level, an anamnestic investigation by phone, a diagnostic framework and follow up digital examinations allowed to manage an unconventional case of oral pathology.
Keywords: Oral Candidiasis; Tele dentistry; Oral pathology
Introduction
The coronavirus disease (COVID-19) continues to be a major health problem in many countries around the world. During the COVID-19 peaks, dental treatments were often postponed, except for emergencies. Dental care has been affected by the well-documented evidence that also asymptomatic patients may transmit the virus during dental procedures producing aerosols [1]. This situation led many patients, with non-urgent oral problems, to resort to mobile consultations by sending pictures to their dentist. These virtual consultations gave dentists the opportunity to triage problems, and gave patients the chance to self-manage minor oral problems. This approach to diagnose and “treat” oral problems is called teledentistry [2-6].
Case Report
On April 9th at 11:44 pm the patient’s mother contacted the pediatric dentist through WhatsApp asking for help and sending a few pictures and a video of her child’s mouth and tongue. The mother reported that his son’s tongue had been hurting and stinging for the past two days and his body temperature increased to 37.5 °C. An anamnesis interview was conducted via WhatsApp: there were no history of burns on his tongue nor of exanthema on his body. The mother reported that the lesions on the tongue became less uniform and more painful throughout the last two days. The child’s tongue pain could be relieved by drinking cold water. In addition, he experienced mild neck pain. From the digital examination by the pictures a normotrophic mucosa in the genial, vestibular, palatal and lingual area of the mouth was noticed with the exception of the area of the tongue’s apex which presented an inhomogeneous aspect with erythematous areas and the absence of papillae interspersed with areas with hypertrophic papillae with pearly white characterizations.
On the basis of these elements it was possible to formulate some diagnostic hypotheses, but none perfectly fitted this case. The pictures may suggest: a burn but the latter cannot explain neck pain and fever; a strawberry tongue but there wasn’t exanthema, throat pain and an high body temperature that could be framed as an early stage of scarlet fever; a Kawasaki syndrome, that during COVID-19 pandemic could be associated to the Sars-CoV 2 virus in children [7,8], but there wasn’t a sign/symptoms of the infection and the mother assured that the child did not experience any social contact outside his family during COVID-19 lockdown. Since no certain diagnosis could be made, a “watch and wait” approach was adopted.
On April 10th at 08:05 am, the mother sent a new picture and referred to the pediatric dentist that her son had trouble sleeping because of pain. He had to sleep with his mouth open and he could relieve his pain slightly only by keeping his tongue out of the mouth. However, his body temperature dropped to normal, no exanthema was present and no new systemic signs/symptoms appeared.
An oral spray rich in Vitamin E (Vea Oris Oral Spray - HULKA s.r.l. - Rovigo, Italy) was prescribed to the patient, suggesting four local applications per day.
On April 11th at 10:53 am, the mother sent a new picture and reported that pain and burn decreased and the child woke up with a white patina on the tongue.
On the basis of the new picture, a diagnostic hypothesis was finally formulated: oral candidiasis. Oral candidiasis in children could be associated with fever and loco-regional lymphadenopathy, explaining the child’s neck pain. According to this hypothesis, throughout the initial manifestations of pain and stinging, the formation of pseudomembranes was partially hindered by the patient’s self-removal using lips and teeth. After the application of the oral spray rich in Vitamin E, which allowed the creation of a protective layer, the absence of friction allowed the development of the pseudomembranes and the attenuation of the painful symptoms. Miconazol Nitrate 2g (Daktarin 20mg/g, Janssen-Cilag S.p.A.) oral gel, 3 applications per day for ten days, was prescribed by Whatsapp.
On April 14th at 10:27 am the mother updated the pediatric dentist with a new picture that shows an improvement of the patient’s tongue.
On April 21st at 12:12 am, last day of drug medication treatment, the mother sent a picture that shows the healed tongue of her son.
On May 11th at 14:31 am, the mother updated the pediatric dentist with two pictures that show, at 1-month follow-up, the complete healing of the tongue with the papillae regrowth.
Discussion
Pseudomembranous candidiasis is one of the most frequently clinical variants of candidiasis in children. Pseudomembranous candidiasis, or thrush, is clinically characterized by white or whitish-yellow, slightly elevated spots or plaques, which may be removed by scraping, usually leaving a reddish underling mucosa [9]. Topical therapies for oropharyngeal candidiasis are considered preferable to systemic therapies and the treatment with Miconazol Nitrate is well supported by literature [10]. This case report shows how, in the era of COVID 19 pandemic, teledentistry has been a valid strategy allowing the resolution of an unconventional case of oral candidiasis. Social platforms and modern technology, through the use of high-resolution pictures even if at an amateur level, have made possible an anamnestic investigation, a diagnostic framework and the follow up of a case of oral pathology in a child, when the conventional examination was difficult to carry-out.
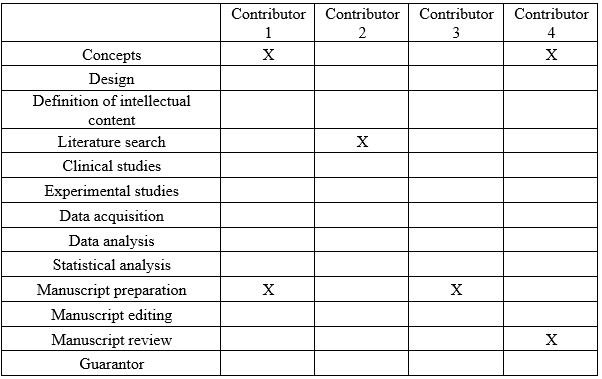
Contribution Details
Grant Information: The author(s) received no specific funding for this work.
Acknowledgement: the authors thank the mother of the little patient who authorized the publication of this case report
References
- Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic. Emerg Infect Dis. 2020; 26(7): e201595.
- Alabdullah JH, Daniel SJ. A Systematic Review on the Validity of Teledentistry. Telemed J E Health. 2018; 24(8): 639–648.
- Khan SA, Omar H. Teledentistry in practice: literature review. Telemed J E Health. 2013; 19(7): 565–567.
- Irving M, Stewart R, Spallek H, Blinkhorn A. Using teledentistry in clinical practice as an enabler to improve access to clinical care: A qualitative systematic review. J Telemed Telecare. 2018; 24(3): 129–146.
- Kopycka-Kedzierawski DT, McLaren SW, Billings RJ. Advancement of teledentistry at the university of Rochester’s Eastman Institute for Oral Health. Health Aff. 2018; 37(12): 1960–1966.
- Baliga SM. Smart pediatric dentistry: We have come a long way! J Indian Soc Pedod Prev Dent. 2020; 38(1): 1.
- Jones VG, Mills M, Suarez D, Hogan CA, Yeh D, Bradley Segal J, et al. COVID-19 and Kawasaki Disease: Novel Virus and Novel Case. Hosp Pediatr. 2020; 10(6): 537-540
- Turnier JL, Anderson MS, Heizer HR, Jone P-N, Glodé MP, Dominguez SR. Concurrent Respiratory Viruses and Kawasaki Disease. Pediatrics. 2015; 136(3): e609-614.
- Laskaris G. Color Atlas of Oral Diseases in Children and Adolescents. Thieme; 2000; 364 p.
- Zhang L-W, Fu J-Y, Hua H, Yan Z-M. Efficacy and safety of miconazole for oral candidiasis: a systematic review and meta-analysis. Oral Diseases. 2016; 22(3): 185–195.

