A Rare Case of Accessory Spleen Torsion Diagnosed by Contrast-Enhanced Ultrasound (CEUS)
Lihua Xiang1,2, Huixiong Xu1,2, Ye Jin1,2 and Liping Sun1,2
1Department of Medical Ultrasound, Shanghai Tenth People’s Hospital, Ultrasound Research and Education Institute, Tongji University Cancer Center, Shanghai Engineering Research Center of Ultrasound Diagnosis and Treatment, Tongji University School of Medicine, 301 Yanchang Middle Road, Shanghai 200072, China
2Ultrasound Research and Education Institute, Tongji University School of Medicine, No. 301, Yanchangzhong Road, Shanghai 200072, China
Received Date: 01/08/2021; Published Date: 27/08/2021
*Corresponding author: Liping. Sun, MD, PhD, Department of Medical Ultrasound, Shanghai Tenth People’s Hospital, Ultrasound Research and Education Institute, Tongji University Cancer Center, Shanghai Engineering Research Center of Ultrasound Diagnosis and Treatment, Tongji University School of Medicine, 301 Yanchang Middle Road, Shanghai 200072, ChinaUltrasound Research and Education Institute, Tongji University School of Medicine, No. 301, Yanchangzhong Road, Shanghai 200072, China
Abstract
Accessory Spleen (AS) is a congenital anomaly of the spleen due to a fusion defect during embryogenesis, frequency of which is around 10 to 30% of the human population. Torsion of an accessory spleen is a rare cause of abdominal pain mostly occurred in children, but rarely diagnosed preoperatively. Here we report an adult female with intermittent abdominal pain attributed to torsion of an accessory spleen as diagnosed by Contrast-Enhanced Ultrasound (CEUS), which was further confirmed by following surgical operation. A comprehensive analysis of accessory spleen torsion in literature is reviewed.
Keywords: Accessory spleen; Contrast-Enhanced Ultrasound (CEUS); Torsion
Introduction
The Accessory Spleen (AS) is a congenital anomaly of the spleen due to a fusion defect during the embryogenesis (1,2). It is commonly diagnosed by ultrasound examination and generally asymptomatic. The torsion of AS occur almost due to the twisted vascular pedicle, which may cause acute abdominal pain as the ischemic changes of the AS, and it is quite difficult to diagnose preoperatively. Recurrent of the torsion of AS was individually reported and surgical removal is still the first choice in clinic.
Case Report
A 26-year-old female feels intermittent abdominal pain but with no palpable incentive. Moreover, the pain was dull and no radiating. There were no other typical symptoms such as nausea and vomiting, fever, gastrointestinal or urinary symptoms based on her statement. This patient did not pay any attention to the pain until she finished the annually physical examination recently. Ultrasound examination revealed a mass with size of 47×41mm located between the spleen and the left kidney. After that, she performed CT examination in other hospitals which also identified the mass and further subjected for MRI examination. Multiparametric Magnetic Resonance Imaging (mp-MRI) clearly indicated the 50×45×53 mm round mass in left upper abdominal cavity clear with obvious peripheral bowel. In addition, her past and family history was otherwise non-contributory and there was no abnormal finding on physical exam and laboratory evaluation.
Specifically, the abdominal ultrasound showed the mass without other abnormal finding of other visceral organs. Under low frequency ultrasound condition, the mass located between the spleen with the left kidney with size of 57×44 mm, and the sharp is round, hypoechoic (similar to the spleen), well defined and homogeneous. Abundant blood flow signals were seen with lower velocity and Resistance Index (RI). When switching the probe to high frequency condition, clear vascular structures were observed within the mass (Figure 1). Furthermore, the contrast-enhanced ultrasound (CEUS) demonstrated the mass had homogeneous enhancement with later perfusion and lower intensity than the spleen (Figure 2).
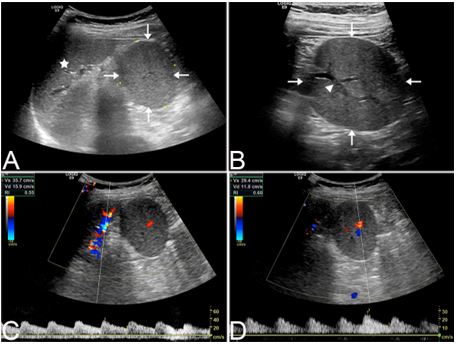
Figure 1: A 26-year-old female with torsion of accessory spleen confirmed via US examination.
(A) low frequency of US clearly showed a round, isoechoic, well-defined, homogeneous mass (arrows) adjacent to the spleen (asterisk).
(B) high frequency US revealed vascular structure (triangle) inside the mass (arrows).
(C) PW showed a higher velocity of the spleen artery.
(D) PW showed a lower velocity of the mass.
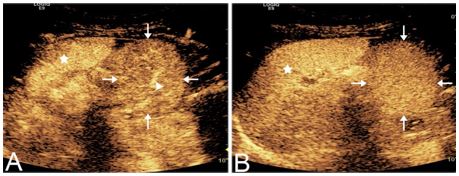
Figure 2: CEUS examination results of the identified accessory spleen torsion.
(A) In the early time the mass (arrows) showed a homogeneous enhancement with lower intensity than the spleen (asterisk) and vascular structure (triangle) inside.
(B) In the later time the mass (arrows) showed a homogeneous enhancement still with lower intensity than the spleen (asterisk).
Based on the diagnosis results, the patient underwent laparoscopic surgery, which confirmed the mass with twisted vascular pedicle, and underwent surgical resection. The histopathology finally verified the torsion of accessory spleen.
Discussion
Occurrence of accessory spleen is approximate 10-30% of human population, which is defined as one or more (from one to six) nodules of additional ectopic splenic parenchyma [1,3,4]. Locations of accessory spleens include closely next to the splenic hilum (75%), adjacent to the pancreatic tail (20%), or appeared alongside with the splenic artery such as the gastrosplenic, splenocolic, astrocolic ligament even in pancreas or rarely the mediastinum (5%) [1,5-7].
Most of accessory spleens are asymptomatic and are discovered incidentally during ultrasound examination [8,9]. Accessory spleens always have their own blood vessels which usually originated from a branch of the splenic artery [10]. The majority of accessory spleens appeared in the splenic hilum with the similar echo to the spleen, and their size are approximately 1 cm in diameter [4] whose blood supply form the splenic artery can always be detected. Nevertheless, once the accessory spleen located in other site, the vascular pedicles are always long which could not be visualized by traditional ultrasound methods, and these accessory spleens are lack of peritoneal ligament system attachments and thus vulnerable to torsion [9].
Torsion of accessory spleen is a rare cause of abdominal pain, which sometimes may induce an acute abdomen mostly reported in children population [11-14]. The sites of abdominal pain may vary individually based on the location of the accessory spleen. Moreover, patients may also suffer from other symptoms inlcuding nausea, vomiting, fever due to the intermittent torsion and even severe pain in case of infarction [6,11]. Currently, it is believed that no correlations are revealed between the size and localization of the spleen, the time of diagnosis, or the age of the patient with the torsion of accessory spleen [12,15-17].
Diagnosis of torsion of accessory spleen is difficult in clinic due to the extremely low incidence and large variation of the mass, making it very hard to be diagnosed ahead of physical operation. Ultrasound is usually the first method for diagnosis due to its convenient and safety, the ultrasonographic manifestations were different which included cases of a homogeneous oval mass with good sound transmission [17], a hypoechoic well-encapsulated oval mass [18], a nodular solid mass [19], and a small round hypoechoic mass surrounded by strongly hyperechogenic mesenteric tissue [14]. In this case, we found the mass displayed a round, hypoechoic (similar to the spleen), well defined, homogeneous lesion phenotypes, strongly suggesting that this is an accessory spleen as it is clear with periphery gastrointestinal tract. When subjected for CEUS analysis, the mass revealed lower enhancement and later perfusion than the spleen suggesting the ischemia of the mass, thus finally convincing our hypothesis of an accessory spleen twisting.
Similar to testicular torsion, the accessory spleen may show larger size than spleen due to the venous congestion, and then the artery ischemia causing infarction and necrosis which resulting in severe abdominal pain [20]. As the vascular pedicle might untwist voluntarily, and switch to twist recurrently, the abdominal pain occurred intermittently and recurrently, respectively. In our case, the size of the accessory spleen increased from 47mm to 57mm with lower velocity than the spleen. It is difficult to make a final diagnosis of accessory spleen torsion with the above ultrasonographic features. Under this condition, CEUS examination was required which revealed a homogeneous enhancement with later perfusion and lower intensity than the spleen, validating the torsion of accessory spleen. By reviewing the literature, we only found one such case diagnosed by CEUS [14] which occurred in 12-year-old male with complete lack of vascularization in CEUS. In our case the blood supply of the accessory spleen is decreasing rather than lacking that making the situation more confused.
It is difficult to make accurate diagnosis as the ultrasound examination can only give some evidences. Contrast enhanced CT and MRI and Angiography and scintigraphy can not only detect the masses but further evaluate their nature and infer its pathology which is helpful to make the correct diagnosis [4,7,9,17,19], especially for identifying the twisting vascular pedicle which is the strongest evidence of the torsion of accessory spleen. However, these methodology may be not available under emergency situations, and are useless when the afferent blood vessels are completely occluded [21]. On the contrary, CEUS is a newly developed approach for evaluating the blood supply in real time. In addition, CEUS is more convenient as compared with these above methods especially in emergency departments.
In conclusion, due to the difficulty to diagnose torsion of an accessory spleen pre-operatively, as well as awareness of this rare case are important in the differential diagnosis of abdominal pain even acute abdomen in children and young adults, we propose here CEUS as a suitable method for the evaluation of the acute abdominal pathology, which can highlight the parenchymal vascularization and evaluate the blood supply in real time.
References
- Wadham B, Adams P, Johnson M. Incidence and location of accessory spleens. The New England journal of medicine 1981; 304(18): 1111.
- Curtis G, Movitz D. The surgical significance of the accessory spleen. Annals of surgery 1946; 123 :276-298.
- Di Serafino M, Verde F, Ferro F, Vezzali N, Rossi E, Acampora C, et al. Ultrasonography of the pediatric spleen: a pictorial essay. Journal of ultrasound 2019; 22(4): 503-512.
- Mortelé K, Mortelé B, Silverman S. CT features of the accessory spleen. AJR American journal of roentgenology 2004; 183(6): 1653-1657.
- Takayama T, Shimada K, Inoue K, Wakao F, Yamamoto J, Kosuge T. Intrapancreatic accessory spleen. Lancet (London, England) 1994; 344(8927): 957-958.
- Babcock T, Coker D, Haynes J, Conklin H. Infarction of an accessory spleen causing an acute abdomen. American journal of surgery 1974; 127(3): 336-337.
- Mendi R, Abramson L, Pillai S, Rigsby C. Evolution of the CT imaging findings of accessory spleen infarction. Pediatric radiology 2006; 36(12): 1319-1322.
- Cowles R, Lazar E. Symptomatic pelvic accessory spleen. American journal of surgery 2007; 194(2): 225-226.
- Lhuaire M, Sommacale D, Piardi T, Grenier P, Diebold M, Avisse C, et al. A rare cause of chronic abdominal pain: recurrent sub-torsions of an accessory spleen. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 2013; 17(10): 1893-1896.
- Sadro C, Lehnert B. Torsion of an accessory spleen: Case report and review of the literature. Radiology case reports 2013; 8(1): 802.
- Seo T, Ito T, Watanabe Y, Umeda T. Torsion of an accessory spleen presenting as an acute abdomen with an inflammatory mass. US, CT, and MRI findings. Pediatric radiology 1994; 24(7): 532-534.
- Impellizzeri P, Montalto A, Borruto F, Antonuccio P, Scalfari G, Arena F, Romeo C. Accessory spleen torsion: rare cause of acute abdomen in children and review of literature. Journal of pediatric surgery 2009; 44(9): e15-18.
- Zhang K, Jia H. Symptomatic accessory spleen. Surgery 2008; 144(3): 476-477.
- Trinci M, Ianniello S, Galluzzo M, Giangregorio C, Palliola R, Briganti V, et al. A rare case of accessory spleen torsion in a child diagnosed by ultrasound (US) and contrast-enhanced ultrasound (CEUS). Journal of ultrasound 2019; 22(1): 99-102.
- Bard V, Goldberg N, Kashtan H. Torsion of a huge accessory spleen in a 20-year-old patient. International journal of surgery case reports 2014; 5(2): 67-69.
- Mocanu S, Sierra Vinuesa A, Muñoz-Ramos Trayter C, Castañeda Figueroa E, Garcia San Pedro A. Accessory spleen torsion in a teenager. ANZ journal of surgery 2015; 85(12): 987-989.
- Pérez Fontán F, Soler R, Santos M, Facio I. Accessory spleen torsion: US, CT and MR findings. European radiology 2001; 11(3): 509-512.
- Dahlin L, Anagnostaki L, Delshammar M, Fork F, Genell S. Torsion of an accessory spleen in an adult. Case report. The European journal of surgery = Acta chirurgica 1995; 161(8): 607-609.
- Valls C, Monés L, Gumà A, López-Calonge E. Torsion of a wandering accessory spleen: CT findings. Abdominal imaging 1998; 23(2): 194-195.
- Tang M, Liu J, Cao L, Zhang X, Gu P, Zhang M, et al. [Contrast-enhanced ultrasonography in the diagnosis of acute experimental incomplete testicular torsion]. Zhonghua nan ke xue = National journal of andrology 2010; 16(9): 799-802.
- Ozeki M, Asakuma M, Go N, Ogura T, Inoue Y, Shimizu T, et al. Torsion of an accessory spleen: a rare case preoperatively diagnosed and cured by single-port surgery. Surgical case reports 2015; 1(1): 100.

