Metastatic Small Cell Lung Cancer: The Role of Multidisciplinary Teams in Patient Care
Austin Frisch1,*, Lindsey LeQuia1, Gustavo Cumbo-Nacheli2
1Michigan State University College of Human Medicine, USA
2Spectrum Health, Department of Pulmonary and Critical Care, USA
Received Date: 30/07/2021; Published Date: 23/08/2021
*Corresponding author: Austin James Frisch, Michigan State University College of Human Medicine, USA. 15 Michigan Street NE, Grand Rapids, MI 49503
Abstract
Small Cell Lung Cancer (SCLC) to this day remains one of the deadliest cancers despite decades of research and treatment advancements. Time of diagnosis to treatment represents a critical component that requires urgency and aggressive planning that also requires complex coordination of care. Here, we present the case of a 64-year-old woman who has widely metastatic SCLC who may benefit from a group of specialists reviewing and taking charge of her case. These Multidisciplinary Teams (MDT) could expedite the treatment planning and staging of SCLC all while providing a patient-centered approach to patient care. This report highlights the importance of establishing care quickly and starting treatment promptly through the introduction of an MDT. We stress the likely improvements these teams may have on patients such as the one presented in this review, and the need for further investigation into improved SCLC patient outcomes associated with them.
Keywords: Small cell lung cancer; Multidisciplinary; Team; Specialist; Metastatic
Introduction
Small Cell Lung Cancer (SCLC) is a highly metastatic carcinoma that comprises roughly 12-15% of all lung cancers and about 30,000 patients are diagnosed each year [1]. Patients who are diagnosed early and with confined SCLC (limited stage) could be considered candidates for surgical resection. However, it is extremely rare for patients with SCLC to demonstrate signs of metastasis at the time of diagnosis and the prognosis - generally poor with a median survival time of 1 year after the diagnosis [2]. Patients who have metastatic SCLC (Extended stage) are not eligible for surgical resection, and generally undergo chemotherapy and radiation3. The mortality of SCLC is high and prompt referral to a multidisciplinary team is encouraged. Various aggressive treatment regimens have become the standard of care [3].
Small Cell lung cancer may metastasize to many organs, common sites include adrenal glands, liver, bone, brain, and hilar lymph nodes. Metastasis to the skin is uncommon and usually indicates a poor prognosis [4]. We present a patient with widely metastatic small cell lung cancer with concerning imaging studies - with multiple metastatic foci, including cutaneous and neurological lesions.
Case Presentation
The patient is a 64-year-old female evaluated for lumps in her skin. These cutaneous areas of concern required workup that included a whole torso PET scan (Figure 1) and a skin biopsy. The biopsy results were consistent with small cell lung cancer and the patient was urgently referred to oncology. An MRI was performed (Figure 2) and was consistent with multiple metastatic foci throughout the CNS. The patient underwent chemotherapy.
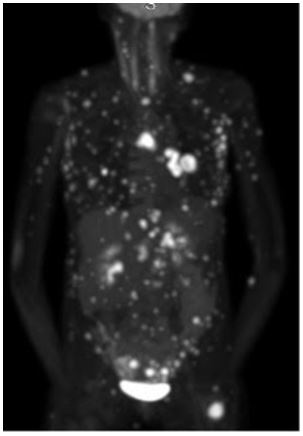
Figure 1: PET scan of patient with highly metastatic Small Cell Lung cancer.
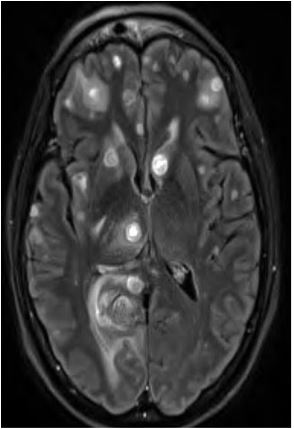
Figure 2: MRI of patient with highly metastatic Small Cell Lung cancer.
Discussion
Small Cell Lung Cancer (SCLC) is one of the most aggressive cancers and is the most aggressive subtype of lung cancer. It is a high-grade neuroendocrine tumor usually resulting from smoking and has a poor prognosis. Patients with SCLC generally present with respiratory symptoms such as cough, hemoptysis, and shortness of breath; while imaging can reveal a centrally located lung mass with thoracic lymph node involvement. Paraneoplastic syndromes including Cushing’s, SIADH, and auto-antibody derived diseases may also present in these patients. SCLC grows rapidly and metastasizes quickly resulting in most patients having extensive stage cancer at the time of diagnosis. A study on SCLC survival over three decades from 1983-2012 did identify a slight increase in 5-year survival rate with each decade, however, the median survival for each decade remained at about 7 months [5]. This highlights the true complexity of SCLC has and the need for urgent workup when this disease is suspected. Immunotherapy and small molecule inhibitors offer options for treatment, although SCLC mortality and treatment outcomes have remained relatively unchanged over the past few years [6]. SCLC patients who have the metastasis seen in Figure 1 will likely benefit from an urgent referral for diagnosis and an aggressive treatment plan. Diagnosing, staging, and treatment planning will likely improve the possibility of improved outcomes. Multidisciplinary Teams (MDTs) are composed of various healthcare specialists who regularly discuss specific individual patients and collaborate on best alternatives to diagnose, discuss treatment plans, and provide timely comprehensive care for these patients. Studies on MDTs generally focus on outcomes based on before and after the MDT interventions and there have been limited studies performed on the impact of MDTs on lung cancer specifically [7]. Other cancers such as breast, head and neck, and rectal have been shown to have more positive outcomes when associated with MDT involvement. Benefits include patient satisfaction, reduced cost, improvement in documentation, and reduction in time between first diagnosis and treatment [8-11]. The time reduction from diagnosis to treatment remains an important aspect of MDTs involvement, particularly with SCLC patients. Coordinating tissue acquisition, staging and treatment for SCLC can prove a challenging task.
There has been conflicting data and controversy surrounding the benefit of resource allocation into MDTs, aimed at improving outcomes among patients with SCLC. A study performed by Bydder et al. (2009) evaluated outcomes of inoperable SCLC patients discussed in MDT meetings versus SCLC patients who were not and found that those who were discussed at the meetings had a mean survival of 280 days versus 205 days for the patients who had no MDT [12]. However, a conflicting study reported in 2011 demonstrated that MDT discussions in SCLC patients was associated with better treatment reception which could lead to better quality of life, but the study did not demonstrate increased survival rates [13]. To date, most of the research within this area has indicated benefits of prompt referral to MDTs aimed at improving the time interval from diagnosis to treatment as well as improving quality of life. Future studies are needed to further understand the role MDTs at improving SCLC survival in patients with ES SCLC - as the one presented in this case [14]. It remains paramount to ascertain best approaches to establish care for SCLC patients, given prognosis.
Conclusion
The aggressive nature of SCLC highlights benefits of expeditious workup and prompt treatment. We highlight the role MDTs to entertain patient diagnostic workup and prompt treatment plans, likely leading to improved outcomes. Although our patient’s prognosis is poor, the added benefit of a MDT included prompt discussions and referrals to specialists. We believe that patients with SCLC will likely benefit from the heightened awareness and coordination a team of specialists.
Authorship Criteria
All three authors contributed to the literature review and case report information.
Austin Frisch (guarantor): concept/design of manuscript, drafting, editing, literature review, and case presentation
Lindsey LeQuia: editing, drafting, literature review
Dr. Cumbo-Nacheli, MD: concept/design of manuscript, editing, case presentation, acquired images
Conflicts of Interest
None.
Grant Information
The author’s received no specific funding for this work.
References
- Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA: a Cancer Journal for Clinicians. 2014; 64(1): 9-29. DOI: 10.3322/caac.21208.
- J de Castro Carpeño M, Cobo Dols M, Domine Gomez P, Ruiz Gracia L, Crama MR. Garcia Campelo, 84P - Survival outcomes in stage IV small-cell lung cancer (IV-SCLC): Analysis from SEER database, Annals of Oncology, 2019; 30(11): xi30. ISSN 0923-7534.
- Rossi A, Di Maio M, Chiodini P, et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: the COCIS meta-analysis of individual patient data, 2012.
- Dreizen S, Dhingra HM, Chiuten DF, Umsawasdi T, Valdivieso M. Cutaneous and subcutaneous metastases of lung cancer. Clinical characteristics. Postgrad Med. 1986; 80(8): 111-116. doi:10.1080/00325481.1986.11699635
- Wang S, Tang J, Sun T, et al. Survival changes in patients with small cell lung cancer and disparities between different sexes, socioeconomic statuses and ages. Sci Rep. 2017; 7(1): 1339. doi: 10.1038/s41598-017-01571-0.
- Oze I, Hotta K, Kiura K, et al. Twenty-seven years of phase III trials for patients with extensive disease small-cell lung cancer: disappointing results. PLoS One. 2009; 4(11): e7835. doi: 10.1371/journal.pone.0007835.
- Hardavella G, Frille A, Theochari C, et al. Multidisciplinary care models for patients with lung cancer. Breathe (Sheff). 2020; 16(4): 200076. doi:10.1183/20734735.0076-2020.
- Burton S, Brown G, Daniels IR, et al. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Br J Cancer. 2006;94(3):351-357. doi: 10.1038/sj.bjc.6602947.
- Westin T, Stalfors J. Tumour boards/multidisciplinary head and neck cancer meetings: are they of value to patients, treating staff or a political additional drain on healthcare resources? Curr Opin Otolaryngol Head Neck Surg. 2008; 16(2): 103-107. doi:10.1097/MOO.0b013e3282f6a4c4.
- Birchall M, Bailey D, King P; South West Cancer Intelligence Service Head and Neck Tumour Panel. Effect of process standards on survival of patients with head and neck cancer in the south and west of England. Br J Cancer. 2004; 91(8): 1477-1481. doi: 10.1038/sj.bjc.6602118.
- Gabel M, Hilton NE, Nathanson SD. Multidisciplinary breast cancer clinics. Do they work? Cancer. 1997; 79(12): 2380-2384.
- Bydder S, Nowak A, Marion K, Phillips M, Atun R. The impact of case discussion at a multidisciplinary team meeting on the treatment and survival of patients with inoperable non-small cell lung cancer. Intern Med J. 2009; 39(12): 838-841. doi:10.1111/j.1445-5994.2009.02019.x.
- Boxer MM, Vinod SK, Shafiq J, Duggan KJ. Do multidisciplinary team meetings make a difference in the management of lung cancer? Cancer. 2011; 117(22): 5112-5120. doi:10.1002/cncr.26149.
- Kowalczyk A, Jassem J. Multidisciplinary team care in advanced lung cancer. Transl Lung Cancer Res. 2020; 9(4): 1690-1698. doi:10.21037/tlcr.2019.11.33

