Allograft Reconstruction of Humeral Head Defect in Treatment of Chronic Locked Posterior Shoulder Dislocation: A Case Report
Soong JW*, Silva AN, Lie D and Lee KH
Singapore General Hospital, Outram Road, Singapore 169608
Received Date: 29/07/2021; Published Date: 19/08/2021
*Corresponding author: Soong Junwei, Singapore General Hospital, Outram Road, Singapore 169608
Abstract
Introduction: Posterior fracture-dislocation of shoulder is a rare injury commonly missed and associated with poor functional outcome when treatment is delayed. We aim to present a case of chronic locked posterior shoulder fracture-dislocation treated with use of allograft reconstruction for humeral head articular defect.
Methods: The clinical case is reviewed prospectively in terms of clinical and functional outcomes. Clinical outcomes include pain score (Numerical Pain Rating Scale) and range of motion (ROM) of shoulder. Functional outcomes include Constant-Murley Shoulder score (CSS), UCLA Shoulder Rating Scale and Oxford Shoulder Score (OSS). In contrast to other scores, OSS score is inversely proportional to outcome.
Results: We report a case of 58-year-old man who presented with persistent pain and limitation in ROM of his right shoulder after a mechanical fall. He was diagnosed and treated surgically for chronic posterior shoulder fracture-dislocation 3 months post-incident. Post-operative X-ray revealed anatomical reduction of the glenohumeral joint with allograft restoration of the humeral head defect. At 1-year post-operation, patient had improvement in isometric strength (from 0lb to 10lb) and in ROM of his right shoulder (from passive flexion of 49˚ to 70˚). There were also improvements in functional outcomes in terms of CSS (from 30 to 36.5), UCLA Shoulder Rating (from 16 to 27) and OSS (from 32 to 23).
Conclusion: Chronic locked posterior shoulder dislocation is a complex injury associated with poor outcome. Allograft restoration of humeral head defect as a salvage procedure can be considered before subjecting the patient to arthroplasty treatment.
Keywords: Posterior shoulder dislocation; Allograft reconstruction; Humeral head defect
Introduction
Posterior dislocation of the shoulder is a rare injury that accounts for less than 2% of all shoulder dislocations [1,2]. It is often attributed to injuries resulting from forceful involuntary muscle contractions such as in in seizures and electrocution. The overpowering strong internal rotators (latissmus dorsi, pectoralis major, subscapularis and teres major) versus the weaker external rotators (teres minor and infraspinatus) leads to the posterior dislocation of the shoulder [3,4]. It is also sustained in major traumatic injuries such as road traffic accidents which involved axial loading of an adducted, flexed and internally rotated arm [5].
The involvement of fracture in posterior shoulder dislocation makes it an even more uncommon clinical entity with an overall incidence of 0.6 per 100,000 population per year [6]. Of the proximal humeral fracture patterns associated in posterior shoulder dislocation, articular fracture of the humeral head with reverse Hill-Sachs lesion is notably the most common fracture type involved [7].
Ciack et al has described chronic ‘locked’ posterior dislocation of shoulder as a missed acute posterior dislocation unrecognised for more than three weeks with associated articular fracture involving the humeral head. This is in contrast to recurrent posterior subluxation of the shoulder which is not associated with trauma and warrants different management [8].
Due to the subtle clinical presentation and radiographic abnormalities, posterior shoulder dislocation is a commonly missed diagnosis resulting in its delayed treatment. It has a missed rate up to 79% on initial examination [9,10]. Delayed treatment can result in unfavourable outcome when it is beyond 4 weeks and salvage procedures may be considered with delay beyond 3 months [11,12].
Research endeavours were made to address the humeral head defect in the chronic locked posterior shoulder dislocation. Treatment options include open reduction, defect filling procedures, rotational osteotomy and arthroplasty. The literature has delved on formulating a guideline in the management of the chronic locked posterior shoulder dislocation based on the size of the humeral head defect [8,12]. Defect filling procedures include non-anatomical and anatomical techniques. McLaughlin procedure is a non-anatomical technique with the transfer of subscapularis tendon to the humeral head defect [13]. Anatomical techniques involved the use of autologous bone graft with iliac crest, or allograft femoral head to restore the sphericity of the fractured humeral head [14,15]. There was also anatomical technique described with elevation of the articular depression and filling of the subchondral defect with allograft bone chips [16]. To date, there is no gold standard or clear consensus in the management for chronic locked posterior shoulder dislocation.
In our case report, we present a clinical case leading to the diagnosis of a chronic locked posterior shoulder dislocation and the surgical management with allograft reconstruction of the humeral head defect. The patient has consented to the presentation of his case for submission to the journal.
Clinical Case
A 58-year-old right hand dominant man presented with pain and limitation in range of motion in his right shoulder after a mechanical fall. He was attended in the emergency department of a tertiary hospital and was diagnosed with an enlocated shoulder with a mildly displaced fracture of the greater tuberosity of right proximal humerus. The initial radiographs taken were anteroposterior and lateral views (Figure 1). No axillary or valpeau views were taken. The patient was treated for the proximal humeral greater tuberosity fracture conservatively for two months.
Although the pain has subsided, the patient still complained of persistent limitation in the range of motion of his right shoulder on subsequent clinical follow-ups. On physical examination, the patient has deformity on his glenohumeral joint with prominent humeral head posteriorly. His right shoulder was limited to 49˚ flexion and 79˚ abduction passively. He was unable to external rotate his right shoulder due to a mechanical block. He had no regimental patch paraesthesia to suggest axillary nerve injury. The neurovascular status of his right upper limb was intact. Hence, radiograph with axillary view was then performed which detected the posterior dislocation of the right shoulder (Figure 2).
The patient decided to seek a second opinion and further imaging of the patient’s right glenohumeral joint was arranged. Computed tomography of the right shoulder performed 3 months after the injury revealed partial union of an impacted fracture involving the greater tuberosity of the proximal right humerus. The posterior dislocation of the glenohumeral joint was associated with a reverse Hill-Sachs lesion which was trapped into the posterior lip of the glenoid cavity. Focal, well corticated bone fragments were visualized posterior to the glenoid process adjacent to the humeral head (Figure 3).
The patient was advised for surgical intervention with open reduction of the chronic locked posterior dislocation of right shoulder with allograft reconstruction of the humeral head defect, keeping in view a possible arthroplasty of humeral head. Prior to surgery, patient was counselled extensively about the potential complications of this challenging surgery. In addition to the usual surgical and anaesthesia complications, we have highlighted to patient the following pertinent possible complications:
1. Iatrogenic humeral head fracture needing additional plate fixation
2. Inability to reduce and secure the humeral head, needing to resort to arthroplasty procedure
3. Persistent posterior shoulder instability post-operatively, due to tight posterior capsule, needing further operations in the future.
4. Permanent reduction in range of motion of the shoulder joint (external rotation) due to contracted anterior capsule
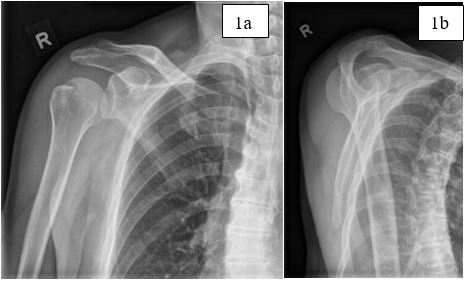
Figure 1:
(1a) AP view: Fracture of greater tuberosity of right proximal humerus. The posterior subluxation is not easily appreciated in this view, leading to delayed diagnosis.
(1b) Lateral view: Slight posterior subluxation of the humeral head on the glenoid cavity.

Figure 2:
(2a) AP view: Healing greater tuberosity fracture of proximal humerus with no displacement.
(2b) Lateral view: Posterior subluxation of the proximal humerus.
(2c) Axillary view: Posterior dislocation of the glenohumeral joint.
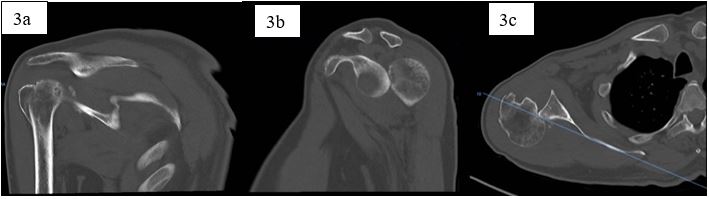
Figure 3:
(3a) Coronal cut: Fracture of greater tuberosity and articular defect of the humeral head
(3b) Sagittal cut: Humeral head dislocated posteriorly to the glenoid cavity
(3c) Axial cut: “Locked” posterior dislocation of humeral head with reverse Hill-Sach lesion engaging on posterior aspect of glenoid
Surgical Procedure
The surgery was performed under general anaesthesia with the patient positioned on the beach chair propped up at 40 degrees. The right shoulder joint was exposed via the deltopectoral approach, and the cephalic vein was identified and protected. The greater tuberosity fracture was noted to have healed (Figure 4). The lesser tuberosity with subscapularis tendon was tagged with Ethibond sutures and an interval was created between the greater and lesser tuberosities to gain access to the shoulder joint. After exposing the shoulder, extensive scar tissue was noted within the joint capsule.
The humeral head was found to be “locked” posteriorly to the glenoid fossa, and extensive release had to be performed to reduce the humeral head. On further evaluation, there was an elliptical depression measuring 3 x 2 cm over the anterior articular margin of the humeral head (40% of articular surface). The articular defect on the humeral head was fashioned with rongeur and curettage, thereby removing the dense fibrous tissue and creating a healthy subchondral tissue bed.
The dimensions of the articular defect were measured, and a fresh frozen femoral head allograft was prepared using an oscillating saw. The surgical team was mindful to avoid harvesting from the superior portion of the femoral head as there might be suboptimal osteochondral bone quality in the weightbearing zone of the femoral head (Figure 5). By harvesting from the non-weight bearing zone of the femoral head, the team was keen to obtain the best quality osteochondral graft for the recipient site. The anterior aspect of the femoral head allograft that would best fit the concavity of the articular defect was harvested (Figure 4). Two 3.5mm headless compression screws were used to secure the osteochondral graft on the articular defect. The sutures from subscapularis and supraspinatus tendons were tied onto each other, and the repair was further reinforced with the use of 4.5mm suture anchor.
Post operatively, the patient was placed in an abduction brace, with no internal rotation allowed for 6 weeks. The post-operative radiograph revealed reduction of the glenohumeral joint with restoration of the humeral head with allograft and the headless compression screws in-situ (Figure 6). The patient was allowed for passive range of motion 6 weeks after the surgery. The subsequent follow up radiographs revealed anatomically reduced humeral head with healing and incorporation of the allograft (Figure 7). The clinical outcomes and functional outcomes were recorded pre-operatively, 6 months and 1 year post-operatively (Figure 8). At 1-year post-operation, the patient has subjectively rated the result of the surgery as “good”. There were no further episodes of posterior dislocation of the shoulder.
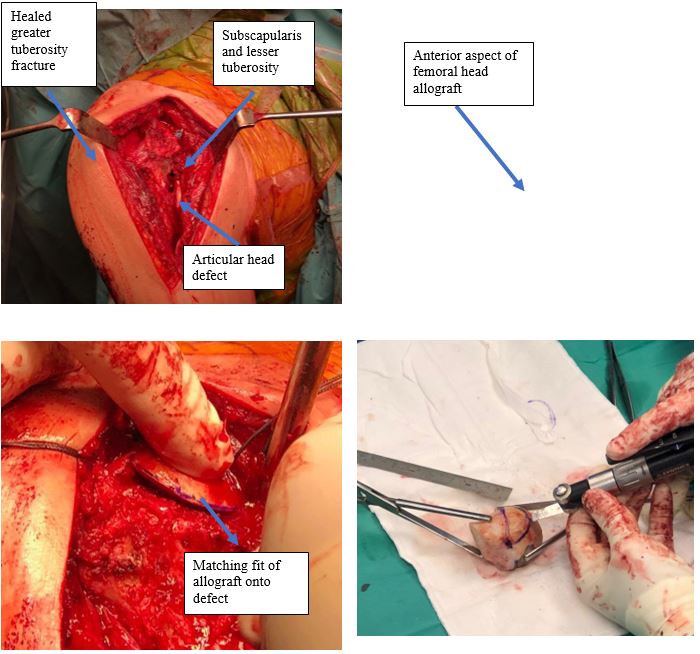
Figure 4: Intra-operative images.
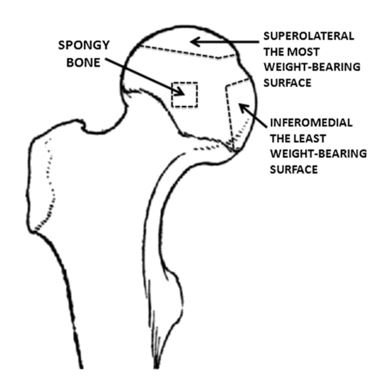
Figure 5: image adopted from Buchwald et al [21].
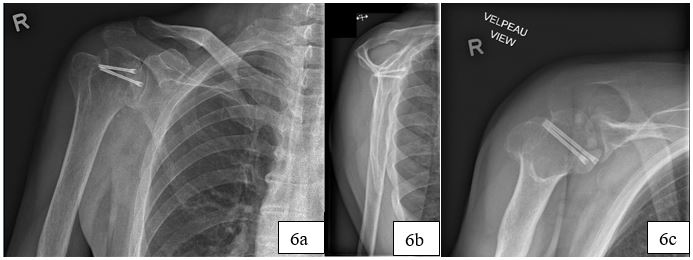
Figure 6: Post-operative X-rays
(6a, 6b, 6c): Glenohumeral joint reduced with allograft reconstruction of the humeral head with 2 headless compression screws in-situ.

Figure 7: Follow up X-rays.
(7a, 7b, 7c): Anatomically reduced humeral head with healing and incorporation of the allograft. No evidence of avascular necrosis of the right humeral head.
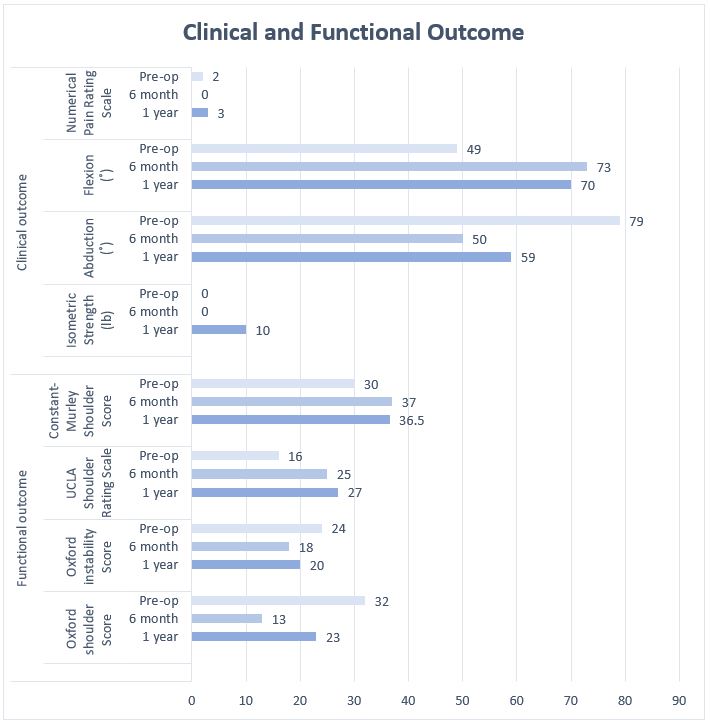
Figure 8:
Constant-Murley Score (range: 0 – 100; best = 100)
UCLA (University of California-Los Angeles) shoulder scale (range: 2 – 35; Best = 35)
Oxford Shoulder Score (range: 12 – 60; best = 12)
Oxford Instability Score (range: 12 – 60; best = 12)
Discussion
This presented case illustrated the difficulties in diagnosing as well as in managing a posterior dislocation of the shoulder in the presence of greater tuberosity fracture and articular head defect. With the low incidence of posterior fracture-dislocation of shoulder and its subtle clinical presentation, the chance of missed diagnosis during initial presentation can be up to 79% [9,10].
Careful and thorough clinical assessment is paramount to ensure a prompt diagnosis. The mechanism of injury involving an epileptic fit, electrocution or a high-velocity injury should raise a suspicion for a posterior dislocation. The clinical manifestation with the shoulder locked in internal rotation with block in passive external rotation is important to suggest the presence of posterior dislocation.
We recommend an orthogonal view of the glenohumeral joint for every shoulder injury complicated with blocked passive external rotation. The X-ray radiographs of the glenohumeral joints in anteroposterior, Y-scapular, axillary views are essential. If the axillary view cannot be performed, we would advise for a valpeau view which allows us to view the congruency of the glenohumeral joint [17].
While the instability of the locked posterior shoulder dislocation is attributed to the attenuation and laxity of the posterior capsulolabral complex, the degree of instability also depends on the size of the humeral defect as it re-engages with the posterior glenoid rim [14]. The literature has recommended the different options of management based on the size of humeral defect [8,12]. In a small defect of less than 25% of humeral head, open reduction can be performed with transfer of upper one-third of subscapularis tendon to the defect with transosseous non-absorbable suture [8]. A moderate defect of 25% - 50% can managed with defect filling procedures which include McLaughlin procedure [13], reconstruction with allograft or autograft. For large defect of more than 50%, hemiarthroplasty has to be considered while total shoulder arthroplasty is used when there is erosion in glenoid [18,19].
Several studies have reported the use of humeral head or femoral head as al allograft for filling the moderate articular defect of the recipient site. The key in achieving favourable clinical outcome in the reconstruction of the humeral head is to achieve the sphericity of the humeral head [12,15]. Gerber et al has introduced the concept of allograft reconstruction of humeral head with good results. The study used fresh frozen femoral or humeral head allograft with 3.5mm cancellous lag screw fixation to reconstruct the articular defect in the humeral head. A total of 19 patients were followed up for a mean of 10.7 years. In the long-term study, Gerber et al has reported a favourable outcome with average Constant-Murley score of 77 point and average Subjective Shoulder Value of 88%. 2 out of 19 patients needed arthroplasty surgery after at least 180 months after the allograft reconstruction surgery [15]. In another long-term study with mean follow up of 122 months, Martinez et al has reported good clinical results in 50% of patients. The other 50% of patients needed arthroplasty surgery. Frozen humeral head allografts were used and headless compression screws were used for fixation of the allograft [20]. Diklic et al reported 70% of the patients with femoral head allograft reconstruction had no pain or restriction of activities of daily living. Their mean Constant-Murley shoulder score was 86.8. No patient had symptoms of instability of the shoulder at mean follow up of 54 months [14].
As for our study, we used femoral head allograft with 3.5mm headless compression screws for fixation on the recipient site. We have harvested from the anterior articular surface of the femoral head allograft. It is important to note that the superolateral and inferomedial region of the femoral head are the most and least weight bearing region respectively (Figure 5) [21]. While avoiding the superolateral region of the femoral head allograft, we have selected the anterior surface of the femoral head in attempt to achieve the best fit for the articular defect.
Our case has demonstrated slight improvement in the functional outcome. However, this was not comparable with the outcomes reported in the literature. The Constant-Murley Score for our case at post-operation 1 year was 36.5 (Figure 8). However, Geber et al reported an average score of 77 at mean follow up of 10.7 years and Diklic et al reported an average score of 86.8 at mean follow up of 54 months. The differences in outcome in our case is likely attributed to the significant delay of 3 months for the treatment. The prolonged “locked” posterior shoulder dislocation have led to scarring of the joint capsule resulting in secondary adhesive capsulitis. This has demonstrated the importance of the prompt diagnosis and correct treatment of “locked” posterior shoulder dislocation to reduce the risk of adverse outcome.
Pre-operative imaging and planning is paramount for surgeons to prepare and to decide on the choice of surgical option. However, intra-operative findings may differ from the findings of the pre-operative imaging and influence a change in surgical plan. For this case, we would recommend keeping arthroplasty options on standby when performing the surgery in case the humeral head is evaluated to be unsalvageable for restoration.
Conclusion
Chronic locked posterior shoulder dislocation is a complex injury associated with poor outcome. A high index of suspicion is needed for prompt diagnosis and treatment to avoid complications like avascular necrosis of humeral head, shoulder stiffness and secondary osteoarthritis. Treatment with restoration of the humeral head as a salvage procedure can be a viable option before subjecting the patient to arthroplasty procedure.
Compliances with Ethical Standards:
The authors declare that they have no conflict of interest.
There is no funding for this project.
Informed consent was obtained from the participant included in our study.
References
- Kowalsky MS, Levine WN. Traumatic posterior glenohumeral dislocation: classification, pathoanatomy, diagnosis, and treatment. Orthop Clin N Am; 2008; 39(4): 519-533.
- Cave EF, Burke JF, Boyd RJ. Trauma management. Chicago: Year Book Medical Publishers; 1974; 437.
- Alhgren O, Lorentzon R, Larsson SE. Posterior dislocation of the shoulder associated with general seizures. Acta Orthop Scand; 1981; 52: 694-695.
- Matsen FA, Thomas SC, Rockwood CA, et al. Glenohumeral instability. In: Rockwood CA, Matsen FA, editors. The shoulder. 2nd Volume 2. Philadelphia, USA: WB Saunders: 1998; 611-754.
- Sheehan S, Gaviola G. Traumatic shoulder injuries: a force mechanism analysis—glenohumeral dislocation and instability. Am J Roentgenol; 2013; 201(2): 378-393.
- Robinson CM. Complex posterior fracture–dislocation of the shoulder: epidemology, injury patterns, and results of operative treatment. J Bone Jt Surg; 2007; 89(7): 1454.
- Rouleau DM, Hebert-Davies J. Incidence of associated injury in posterior shoulder dislocation: systematic review of the literature. J Orthop Trauma; 2012; 26(4): 246-251.
- Cicak N. 2004. Posterior dislocation of the shoulder. J Bone Joint Surg Br. 2004; 86(3): 324-332.
- Rowe CR, Zarins B. 1982. Chronic unreduced dislocations of the shoulder. J Bone Jt Surg Am; 1982; 64(4): 494-505.
- Casado-Sanz E, Barco R, Antuna SA. 2014. Complex fractures of the proximal humerus. Complex fractures of the limbs. Springer, Cham, 2014; 1-8.
- Schliemann B, Muder D, Gessmann J, et al. Locked posterior shoulder dislocation: treatment options and clinical outcomes. Arch Orthop Trauma Surg; 2011; 131(8): 1127-1134.
- Kokkalis ZT, Iliopoulos ID, Antoniou G, et al. Posterior shoulder fracture-dislocation: an update with treatment algorithm. Eur J Orthop Surg Traumatol; 2017; 27(3): 285-294.
- McLaughlin HL. Posterior dislocation of the shoulder. J Bone Jt Surg Am; 1952; 24A(3): 584-590.
- Diklic ID, Ganic ZD, Blagojevic ZD, et al. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Jt Surg Br; 2010; 92(1): 71-76.
- Gerber C, Catanzaro S, Jundt-Ecker M, et al. Long- term outcome of segmental reconstruction of the humeral head for the treatment of locked posterior dislocation of the shoulder. J Shoulder Elb Surg; 2014; 23(11):1682-1690.
- Khayal T, Wild M, Windolf J. Reconstruction of the articular surface of the humeral head after locked posterior shoulder dislocation: a case report. Arch Orthop Trauma Surg; 2009; 129(4): 515-519.
- Bloom MH, Obata WG. Diagnosis of posterior dislocation of the shoulder with use of Velpeau axillary and angle-up roentgenographic views. J Bone Joint Surg Am; 1967; 49(5): 943-949.
- Page AE, Meinhard BP, Schulz E, et al. Bilateral posterior fracture-dislocation of the shoulders: management by bilateral shoulder hemiarthroplasties. J Orthop Trauma; 1995; 9:526-529.
- Hawkins RJ. Unrecognised dislocations of the shoulder. Inst Course Lect; 1986; 258-63.
- Martinez AA, Navarro E, Iglesias D, et al. Long-term follow-up of allograft reconstruction of segmental defects of the humeral head associated with posterior dislocation of the shoulder. Injury; 2013; 44(4): 488-491.
- Buchwald T, Niciejewski K, Kozielski M, et al. Identifying compositional and structural changes in spongy and subchondral bone from the hip joints of patients with osteoarthritis using Raman spectroscopy. J Biomed Opt; 2012; 17(1): 017007.

