Burning Mouth Syndrome: A Case Report
Mainak Datta*, Rupam Sinha, Suman Sen, Harshvardhan Jha
Department of oral medicine and radiology, Haldia institute of dental sciences and research, India
Received Date: 17/07/2021; Published Date: 12/08/2021
*Corresponding author: Mainak Datta, Post graduate trainee, Department of oral medicine and radiology, Haldia institute of dental sciences and research.
Abstract
Burning Mouth Syndrome (BMS), a chronic oro-facial pain disorder, characterized by the presence of burning sensation of the oral mucosa. This condition mainly affects post-menopausal woman secondary to hormonal changes or psychological disorders. Beside burning sensation, patient with BMS also complains of oral mucosal pain, altered taste sensation, and dryness of mouth. This condition is probably of multifactorial origin, often idiopathic and its exact etiopathogenesis is still unclear. There is no definitive treatment protocol for this condition and most of the cases symptomatic treatment done. In Present case, a 65 years old male patient, reported with burning sensation of inner portion of the lower lip and Right and Left buccal mucosa since last 1 month with altered salivation. Complementary Diagnostic tests such as Routine blood examination performed and considering all clinico-pathological datas, it was diagnosed as BMS and treatment started with Periodic follow-up with interval of 1 month and condition improved in every appointment observed.
Keywords: Burning Mouth Syndrome; Psycosomatic; Stomatodynia; Xerostomia
Introduction
Burning Mouth syndrome (BMS), a chronic oro-facial pain disorder has been defined by the ‘International Association for the Study of Pain (IASP)’ as “Burning pain in the tongue or other oral mucous membrane associated with normal signs and laboratory findings lasting at least 4-6 months.” This Clinical entity is uncommon diagnostic dilemma of Oral Mucosa to Oral health care professional. Though it is rarely encounter in daily practice but rarely seen in geriatric age group, Numerous reviews of literature showed it has a prevalence of 0.6% to 15%. BMS exhibits significant female predilection and the ratio between females and males varies from 3:1 to 16:1.
There are various etiologic factors thought to be responsible for BMS, but no single one explains its etiopathogenesis properly. Reported etiological factors for BMS incudes.
The Predisposing factors of Burning mouth Syndrome
1. Local
Ill-fitting dentures, Parafunctional habit (Bruxism, Tongue posture, Myofascial pain etc), Allergic Contact, Stomatitis, Caustic Oral Rinses, Neuropathy – Trigeminal neuralgia, Infection- Bacterial/ Viral/Fungal , Reduced salivary secretion/ Xerostomia, Salivary gland disorders
2. Systemic
Reduced level of Hb and Vitamin B12, Folate, Zinc, Endocrinopathy – Diabates , Thyroid, Hormonal , Hyposalivation – Sjogren‘s syndrome , Sicca Sydrome, Medication- Angiotensin Converting Enzyme (ACE) inhitors, Antihyperglycemic
3. Phychological
Depression, Anxiety, Obsessive compulsive disorder, Cncerophobia, Psychological disorder.
Case Report
A 65 years old male patient reported to the department of oral medicine and radiology with the complain of burning sensation in the inner portion of the lower lip and Right and Left inner mucosa since last 1 month and absence of multiple teeth since last 2 years. Patient had a history of severe Burning sensation in the oral mucosa along with dryness of mouth with altered taste sensation. Burning sensation was Continuous in onset, Aggravated during intake of Hot and spicy along with chilly containing food and relieved by cold water intake. He also gave a history that burning sensation was present when he woke up in the morning and it even disturbed his sleep at night.
Upon Extra-oral Examination, there was no pathology present. Patient gave history of having no deleterious oral habit and he brushed once daily with toothpaste and toothbrush. Upon intraoral examination, there was generalized pallor involving both Right and left sided buccal mucosa, palatal mucosa, inner surface of lip and dorsal surface of tongue. Intra-oral examination revealed that, the patient had dry mouth as the mirror test was positive. The salivary flow was diminished. Depilation of tongue was also evident in posterior 1/3rd portion of dorsal surface of tongue. On Hard tissue examination, generalized attrition along with generalized cervical abrasion was present. 11 to 17, 26, 36, 45, 46, 47 were missing teeth. The provisional diagnosis was given as Anemic Stomatitis and Differential diagnosis was given as Burning mouth syndrome. We used the pain Visual Analog Scale (VAS) for measuring the extent of patients burning sensation. On a scale of 10 the patient gave the burning sensation a value of 8.
The patient was advised for an Orthopantomogram (OPG) and Complete hemogram. The OPG showed, Missing teeth in relation to 11 to 17, 26, 36, 45, 46, 47. There was loss of crown structure in most of the present teeth. Blood investigations was under normal limits. The OPG combined with the results of the blood investigation ruled out any kind of Pulpal or periodontal infections, and anemic stomatitis.
Since no pathological entity found, which could have cause burning sensation we gave a final diagnosis as Burning Mouth Syndrome (BMS).
Patient was advised Tablet Tricyclic Anti-Depressant Amitriptyline (TCA) 10mg once daily at the bed time, Tablet Vitamin C three to four times daily, Mouthwash Benzylamine Hydrochloride 0.15% w/v three times daily, Multivitamin capsules once daily after meal, local application of Anesthetic, Analgesic and antiseptic gel for 1 month and was recalled. In follow up, there was a significant reduction in the burning sensation and upon VAS scale gave a value of 5, which shows marked reduction in burning sensation from previous appointment and same medications were continued. In the future follow up appointment, VAS reduced to 3.
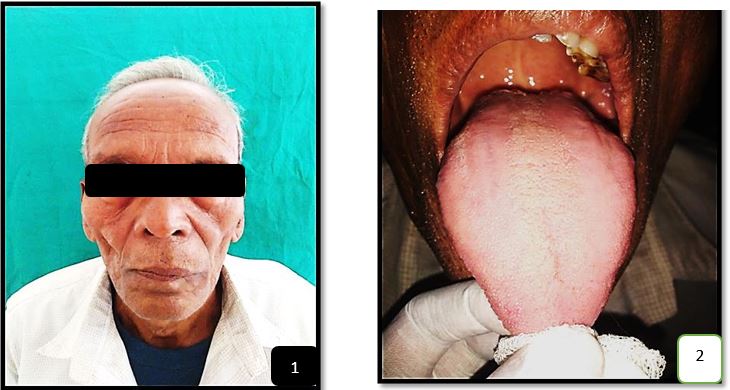
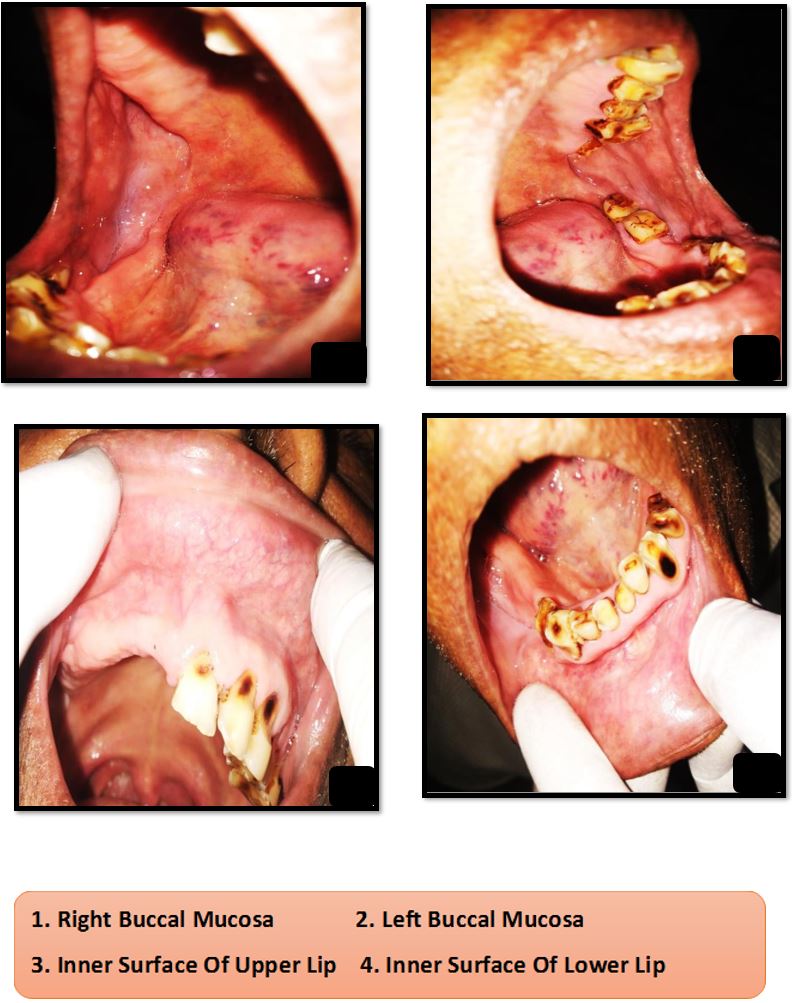
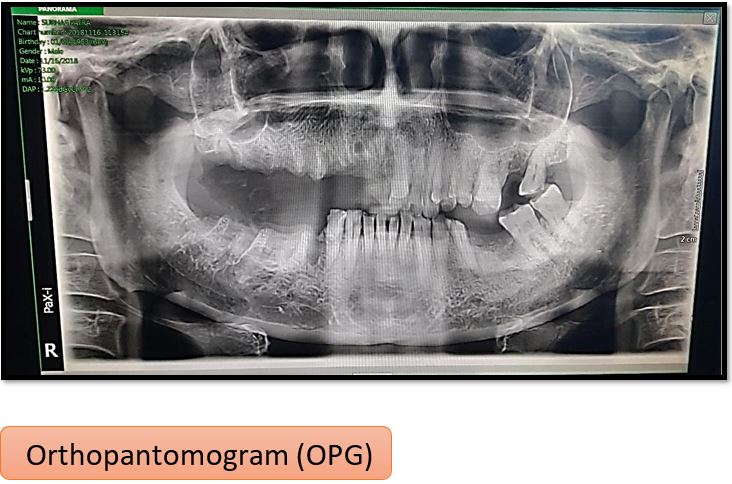
Figure 1: Facial Profile
Figure 2: Intraoral View of Dorsum of Tongue
Figure 3,4: Intra-oral view of right and left buccal mucosa
Figure 5,6: Intra-oral view of upper and lower labial mucosa
Figure 7: Orthopantomogram (OPG)
Discussion
Pain in the orofacial region has always been of profound problem to the patients as the same time certain pain disorders are very difficult to diagnose by the diagnosticians. One of one of such diagnostic dilemmas is ‘Burning mouth syndrome’. This entity has been called by various names such as stomatopyrosis, glossodynia, Stomatodynia, sore mouth etc.
There has been several classifications attributed to this disorder; the one suggested by Lamey and Lewis in 1989 is the most accepted around the world. The classification is as follows: 7
- Type 1 (35%) Patient had burning sensation daily which is absent in morning after waking but increases as the day progresses and became maximum at evening and it is associated with systemic disorder and nutritional deficiency
- Type 2 (55%) had burning sensation daily on awakening and often makes falling asleep at night This subgroup of patients often reports mood changes, alterations in eating habits, and decreased desire to socialize, which seem to be attributable to an altered sleep pattern
- Type 3 (10%) is characterized by burning sensation intermittently, affecting unusual sites such as the floor of the mouth, buccal mucosa, and throat. Generally, shows anxiety and allergic reactions, particularly to food
As per the case history of our patient, the case that we reported here comes under type 2 of the above-mentioned classification.
The clinical symptoms which are generally seen in the patient in BMS are burning sensation which generally starts in the anterior 2/3rd of the tongue, involves palate and can later on involves multiple intraoral sites. Along with these, other symptoms that are seen are Xerostomia, altered taste sensation (Dysgeusia), Difficulty in speech
Patients with BMS have also reported with difficulty in sleep. The burning sensation which is present generally starts when the patients wake up and reaches its peak by late evening. In our patient, most of these symptoms including burning sensation in tongue region and multiple oral sites, Xerostomia, difficulty in sleep, increase burning sensation in the evening were present.
There is no underlying pathology which is related to BMS, as a result we have to rule out all other possibilities and underlying reasons. Odontogenic, Non-odontogenic and Systemic causes should be ruled out and then only we can reach a diagnosis of BMS, in our Patient we did the same thing and there was no Odontogenic / Non – Odontogenic or systemic causes.
Few other oral conditions which mimic BMS includes herpes simplex virus infection, oral candidiasis, HIV, medications, Gastro-esophageal reflux disease, scleroderma, Sjogren syndrome, neuropathy, diabetes, Vitamin deficiency, multiple sclerosis, fibromyalgia, anemia, dehydration etc.
Steps that Can be used to diagnose BMS condition:
1. sensation of pain should be quantified by VAS scale
2. Thorough examination of the oral mucosa should be performed to check any local and systemic factors for burning sensation
- Investigations of any psychological stress factors
1. Monitoring salivary flow
2. Neurological imaging and examination to rule out any pathology and degenerative disorders
3. Patch test for allergic individuals
- Hematological test to rule out nutritional, hormonal, autoimmune
The different treatment modalities used in the management of BMS:
A. Pharmacological agents:
- Topical
Topical application of capsaicin (0.025% cream) 0.15% benzydamine hydrochloride Clonazepam (by sucking a tablet of 1 mg) local anesthetic agent, lidocaine
Topical application of 0.5 ml Aloe vera gel at 70%, 3 times a day Topical lactoperoxidase (biotene mouthwash)
5% doxepin
(2) Systemic
Selective serotonin reuptake inhibitor antidepressants like sertraline (50 mg/day), paroxetine (20 mg/day) for 8 weeks
Antipsychotics such as amisulpride, levosulpiride at a dose of 50 mg/day for 24 weeks
Alpha‑lipoic acid (ALA) at a dose of 600 mg/day, either alone or in combination for 2 months, acts as an antioxidant and a powerful neuroprotective agent
Systemic capsaicin (0.25% capsules, 3 times a day, for 1 month)
Benzodiazepines at low doses. Clonazepam (0.5 mg/day) and alprazolam (0.25 mg to 2 mg/day)
Hormone replacement therapy (conjugated estrogens like premarin, 0.625 mg/day for 21 days and medroxyprogesterone acetate like farlutal, 10 mg/day from day 12 through day 21
B. Non-pharmacological therapy:
- Cognitive-behavioral therapy
- Mindfulness meditation
- Other relaxation techniques
Conclusion
This entity has peculiar features that’s why most of the time it get misdiagnosed. It is the primary duty of the clinician and diagnosticians to properly know about the features of Burning mouth syndrome so that proper diagnosis can be done which will eventually lead to a correct treatment plan.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent forms from patient. In the form the patient(s) has given his consent for images and other clinical information to be reported in the journal. The patient had understood that his personal informations will not be published regardingly.
Financial support and sponsorship: Nill
Conflicts of interest: There are no conflicts of interest.
References
- Aravindhan R, Vidyalakshmi S, Kumar MS, Satheesh C, Balasubramanium AM, Prasad VS. Burning mouth syndrome: A review on its diagnostic and therapeutic J Pharm Bioallied Sci. 2014; 6(Suppl 1): S21-S25.
- Nasri-Heir C, Zagury JG, Thomas D, Ananthan Burning mouth syndrome: Current concepts. J Indian Prosthodont Soc. 2015; 15(4): 300-307.
- Feller L, Fourie J, Bouckaert M, Khammissa RAG, Ballyram R, Lemmer J. Burning Mouth Syndrome: Aetiopathogenesis and Principles of Management. Pain Res Manag. 2017; 2017: 1926269
- Cerchiari DP, de Moricz RD, Sanjar FA, Rapoport PB, Moretti G, Guerra MM. Burning mouth syndrome: etiology. Braz J Otorhinolaryngol. 2006; 72(3): 419-423.
- Sun A, Wu KM, Wang YP, Lin HP, Chen HM, Chiang Burning mouth syndrome: a review and update. J Oral Pathol Med. 2013; 42(9): 649-655
- Kamala KA, Sankethguddad S, Sujith SG, Tantradi P. Burning Mouth Syndrome. Indian J Palliat Care. 2016; 22(1): 74-79.
- Coculescu EC, Radu A, Coculescu BI. Burning mouth syndrome: a review on diagnosis and treatment. J Med Life. 2014; 7(4): 512-515.
- Teruel A, Patel Burning mouth syndrome: a review of etiology, diagnosis, and management. Gen Dent. 2019; 67(2): 24-29.
- Grinspan D, Fernandez Blanco G, Allevato MA, Stengel FM. Burning mouth syndrome. Int J Dermatol 2014; 34: 483-487.
- Grushka M. Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol 2012; 63: 30-36.
- Ship JA, Grushka M, Lipton JA, Mott AE, Sessle BJ, Dionne RA. Burning mouth syndrome; an update. J Am Dent Assoc 2015; 126: 842-853.

