Pulpal Response After Fragment Reattachment of Uncomplicated Fractured Incisors
Dhoum S, Khamlich K, Dakkaki J, Elmerini H, Sidqui M
Department of conservative dentistry and endodontics, School of Dental Medicine, Hassan II University, Casablanca,Morocco
Department of orthodontics School of Dental Medicine, Hassan II University, Casablanca, Morocco
Head of Department of conservative dentistry and endodontics, School of Dental Medicine, Hassan II University, Casablanca, Morocco
Head chief of Dental Diagnosis and Emergencies department, School of Dental Medicine, Hassan II University, Casablanca, Morocco
Received Date: 01/07/2021; Published Date: 20/07/2021
*Corresponding author: Dhoum Sara, Department of conservative dentistry and endodontics, School of Dental Medicine, Hassan II University, Casablanca, Morocco. Email: saradhoum@hotmail.com
Abstract
Coronal fractures of the anterior teeth are common consequence of traumatic dental injuries. Reattachment of fractured tooth fragments using dental adhesive techniques remain the golden choice and offering some advantages, including restoration of the function, esthetics, shape, texture, and brightness of the surface.
This article presents a clinical protocol to reconstruct accidentally damaged maxillary permanent central incisor using composite resin material and a fractured tooth component. The article’s aim is to show, through this clinical case, the pulpal response following an enamel-dentin uncomplicated fracture.
Introduction
Dental fractures due to trauma in the anterior region of the maxilla are very common. The maxillary central incisors are the most commonly injured teeth for both the primary and secondary dentitions [1]. Moreover, uncomplicated crown fractures: enamel-dentin fracture without pulpal involvement; are the most prevalent injury to the permanent dentition [2,3].
If the fragment is retrieved after the trauma, reattachment could be a viable treatment option. This technique is considered to be a very conservative and cost-effective approach. In many situations where this technique is possible, its simplicity and functional and aesthetic successes make it preferable to other treatments, such as composite build- ups or crown restorations [2,3].
Previous studies have reported different results regarding the amount of bond strength recovered by this type of restoration. Bond strengths range from less than half of that of the original tooth, up to strengths close to that of intact teeth. These results depend upon a number of factors. Dehydration and rehydration of the fragment, and the duration of the rehydration phase are some of the factors that, when modified, have been shown to affect the final strength of the restoration. Some researchers have recommended storing the fragment in water for 24 hours prior to bonding, whereas others have reported 30 minutes to be sufficient storage time for rewetting the dental tissue [4].
Therefore, education to increase public awareness of dental emergencies and their management has now become essential.
The pulp reactions of traumatized teeth have been the subject of many investigations, and have been for years a topic of interest. The healing of the pulp is multifactorial and depends on what is done (intrinsic to the neurovascular bundle, pulpal immune potential) and severity and multiplicity of trauma, therapeutic management, bacterial contamination.
This article presents a clinical protocol to reconstruct accidentally damaged maxillary central incisor using composite resin material and the fractured component of the tooth. The purpose of this study was to show, through a 2 years clinical and radiographic follow-up, the pulpal response following a permanent traumatized tooth: enamel-dentin fracture without pulpal involvement.
Methods
A 22-years old woman was referred to the Dental Consultation and Emergency Department (SCUD) for treatment, reporting trauma to the maxillary right central incisor (11). The history revealed that the trauma was the result of a fall. No previous treatment had been provided and the crown fragment was stored in milk.
The intraoral examination revealed an uncomplicated crown fracture in the middle third of the tooth involving the enamel and dentin with no pulp exposure with signs and symptoms of contusion. The patient also suffered higher lip laceration due to the accident.

Figure 1: Initial state after the first appointment.

Figure 2 : Coronal fragment preserved in sterilized milk by the patient, examination of its integrity and the good adaptation of the fracture line.
Radiographic examination of the lip and maxillary central incisors were conducted. Analysis of the maxillary central incisor’s radiographs revealed no abnormalities such as damage of the remaining roots or supporting tissue. The higher lip radiograph was taken and revealed the absence of fragments of the fractured crown.
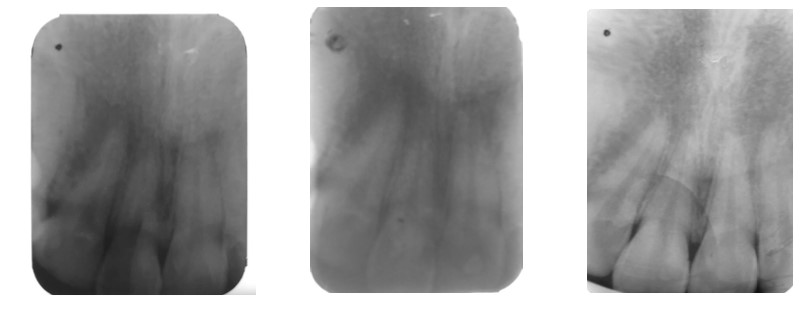
Figure 3: Radiological examination showing no associate fracture or trauma.
The patient was healthy and presented an overall satisfying oral health and the operative area was free of visible plaque.
The plan was to replace the missing part of the maxillary right central incisor by adhesive attachment of the fractured fragment of the tooth.
The fracture component and tooth structure of the maxillary right central incisor were cleaned and dried. Both surfaces of connection were etched with 37% orthophosphoric acid gel, rinsed, and gently dried.

Figure 4: Etching after putting the rubberdam.
A bonding agent was applied to the etched surfaces and gently blown. A thin layer of flow composite was applied to both surfaces, and the fragment was precisely repositioned and polymerized using an LED curing unit for 40 seconds buccally and palatially.

Figure 5 : Reattachment of the fractured fragment.
The position of the attached component was controlled in the patient’s mouth. The last step was polishing, and checking the occlusion.

Figure 6 : Post-op aspect of the reattached fragment.
1 week, 3 months (Figure 8), 18 months (Figure 9,11) and 36 months (Figure 10,12) Follow up, has showed no pulpal or periapical complications.
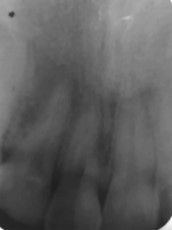
Figure 7: Post-op radiological examination.

Figure 8: Radiological examination after 3 months.

Figure 9: Radiological examination after 18 months.

Figure 10: Radiological examincation after 36 months

Figure 11: Clinical examination after 18 months

Figure 12: clinical examination after 36 months showing
Discussion
Coronal fracture by trauma accounts for 92% of traumatic injuries affecting permanent dentition. Most cases of trauma involve the maxillary central incisors [5,6].
There are many treatment options for fractured teeth, and it is possible to restore function and esthetics using very conservative restorative techniques [7,9-11].
This case report shows that fractured tooth fragments can be successfully used for tooth restoration.
A full recovery of fractured anterior teeth requires restoration of the color, dental anatomy, translucency, curvature of the smile line, and harmony with the other teeth in the arch. The restored fractured tooth must be well adapted, esthetic, functional, and accepted by the patient [8,9,12,14].
An acceptable alternative to traditional direct composite restoration of a fractured tooth is original fractured fragment reattachment, which is conservative, very esthetic, and cost reductive. The technique of reattaching a tooth fragment was first described by Chosack and Eidelman in 1964 and developed in Copenhagen as a routine treatment for coronal fractures with and without pulp exposure in 1984 [15,16].
The Pulpal Response:
If the neurovascular bundle is intact or partially damaged and in case of bacterial infection, pulpal survival is possible. Within the pulp, regressive changes are nonetheless observable, notably with hyalinization and the deposition of diffuse and amorphous calcifications.
Canal obliteration, also known as PCO (Pulp Canal Obliteration) or calcifying metaplasia, is a frequent consumption of trauma, auto transplantation or orthodontic treatment. It can be partial or total. In the retrospective study of Oginni et al. on the exposed teeth of the canal obliterations, 56.9% of the traumatized teeth, on a partial obliteration and 43.1% a total obliteration. The etiology is currently unknown. Several hypotheses have been put forward. It could be related to an alteration of the blood circulation caused by the uncontrolled formation of calcified tissue along the canal walls.
The pulp bleeding and blood clots were pathological mineralization zones. This must be considered as a response to severe damage to the vasculo-nervous bundle. According to Andreasen [7,8,13], this would be an uncontrollable response of the sympathetic nervous system in response to trauma, resulting in particular from the loss of inhibition of the parasympathetic nervous system. Finally, according to Torneck, pulp calcification would come from a simple stimulation of pre-existing odontoblasts increasing their secretion rate.
Pulp necrosis can occur immediately when the trauma is responsible for the section of the vascular bundle without the possibility of pulpal revascularization.
Effect of dehydration and rehydration intervals on fracture resistance:
Rehydration2 was shown, in several studies, to be an important step for the reattachment strength of tooth fragments regardless of the periods tested. A 15-minute tooth fragment rehydration before multimode universal adhesive bonding maintained sufficient moisture to increase reattachment strength. Different dehydrations periods did not influence the reattachment strength whenever rehydration was performed.
Moreover, preservation of the tooth in hypertonic 50% dextrose solution for 2 hours results in a higher strength of the bond between the restoration and the tooth compared to storage in water, milk, or dried conditions [17,18,19,20].
Conclusion
Reattachment of the fractured fragment is a conservative procedure that can preserve aesthetics, restore masticatory function, and provide an immediate positive emotional response from the patient.
Radiographic follow-up of trauma is an essential tool for the visualization of small alterations in the space of the periodontal ligament, suggestive of resorptive processes.
The medium/long-term follow-up is imperative for a thorough evaluation of the pulp condition of the traumatized tooth.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
References
- International Association of Dental Traumatology DENTAL TRAUMA GUIDELINES, AAE, revised version 2012.
- Rodrigues Campos Soares T, de Andrade Risso P, Cople Maia L. Traumatic dental injury in permanent teeth of young patients attended at the federal University of Rio de Janeiro, Brazil. Dent Traumatol, 2014; 30(4): 312-316.
- Koch G, Poulsen S. Pediatric Dentistry: A Clinical Approach. 2e éd. Willey-Blackwell, 2009.
- R Lam. Epidemiology and outcomes of traumatic dental injuries: a review of the literature Australian Dental Journal 2016; 61: 4-20.
- Atabek D, Alaçam A, Konakoglu G. a retrospective study of traumatic dental injuries. Dent Traumatol, 2014; 30(2): 154-61.
- Ravn JJ. Follow-up study of permanent incisors with enamel fractures as a result of an acute trauma. Scand J Dent Res. 1981; 89(3): 213-217.
- Robertson A, Andreasen FM, Bergenholtz G, Andreasen JO, Munksgaard C. Pulp reactions to restoration of experimentally induced crown fractures. J Dent. 1998; 26(5-6): 409-416.
- Farik B, Munksgaard EC, Andreasen JO, Kreiborg S. Fractured teeth bonded with dentin adhesives with and without unfilled resin. Dent Traumatol. 2002; 18(2): 66-69.
- Reis A, Francci C, Loquercio AD, Carrilho MR, Rodrigues Filho LE. Re-attachment of anterior fractured teeth: fracture strength using different techniques. Oper Dent. 2001; 26(3): 287-94.
- Demarco FF, Fay RM, Pinzon LM, Powers JM. Fracture resistance of re-attached coronal fragments – influence of different adhesive materials and bevel preparation. Dent Traumatol. 2004; 20(3):157-63.
- Loguercio AD, Mengarda J, Amaral R, Kraul A, Reis A. Effect of fractured or sectioned fragments on the fracture strength of different reattachment techniques. Oper Dent. 2004; 29(3): 295- 300.
- Bhargava M, Pandit IK, Srivastava N, Gugnani N, Gupta M. An evaluation of various materials and tooth preparation designs used for reattachment of fractured incisors. Dent Traumatol. 2010; 26(5): 409-412. Erratum in: Dent Traumatol. 2010; 26(6): 532.
- Munksgaard EC, Højtved L, Jørgensen EH, Andreasen JO, Andreasen FM. Enamel-dentin crown fractures bonded with various bonding agents. Endod Dent Traumatol. 1991; 7(2): 73-77.
- Reis A, Kraul A, Francci C, de Assis TG, Crivelli DD, Oda M et al. Re-attachment of anterior fractured teeth: fracture strength using different materials. Oper Dent. 2002; 27(6): 621-627.
- Chosack A, Eidelman E. Rehabilitation of a fractured incisor using the patient’s natural crown- case report. J Dent Child 1964; 71: 19-21.
- Stellini E, Stomaci D, Stomaci M, Petrone N, Favero L. Fracture strength of tooth fragment reattachments with postpone bevel and overcontour reconstruction. Dent Traumatol. 2008; 24(3): 283-288.
- Stellini E, Stomaci D, Zuccon A, Bressan E, Ferro R, Petrone N, Favero L, Mazzoleni S. Tooth fragment reattachment through the use of a nanofilled composite resin. Eur J Paediatr Dent. 2010; 11(2): 77-81.
- Chazine M, Sedda M, Ounsi HF, Paragliola R, Ferrari M, Grandini S. Evaluation of the fracture resistance of reattached incisal fragments using different materials and techniques. Dent Traumatol. 2011; 27(1): 15-8.
- Garcia FCP, Poubel LND, Almeida JCF, Toledo IP, Poi WR, Guerra SNE, et al. Tooth fragment reattachment techniques-A systematic review. Dent Traumatol. 2018; 34(3): 135-143. doi: 10.1111/edt.12392.
- Szmidt M, Górski M, Barczak K, Buczkowska-Radlińska J, Hab N Med. Direct Resin Composite Restoration of Maxillary Central Incisors with Fractured Tooth Fragment Reattachment: Case Report. 2017; 37(2), 249-253.

