Intracholedochal Metal Clips Migration: Case Report and Literature Review
Noureddine Njoumi*, Facial Mouhafid, Abdelmounaim Ait Ali, Aziz Zentar
Department of visceral Surgery, Mohamed V University Training Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Received Date: 23/06/2021; Published Date: 12/07/2021
*Corresponding author: Noureddine Njoumi, Department of Visceral Surgery, Mohamed V Hospital, Hay Ryad 10100, Rabat, Morocco. E-mail: njouminoureddine@gmail.com
Abstract
Laparoscopic approach is considered as the "gold standard" for the surgical treatment of gallbladder lithiasis. The hemostasis and bilistasis are often achieved using metal clips. If the most feared complications are bile duct injury and bleeding, Post-cholecystectomy clips migration is a rare late complication of this common procedure.
We report here a case of a 59-year-old woman who was presented with cholestatic jaundice following migration of six metal clips in the common bile duct six months after surgery. This event has been initially managed by endoscopic retrograde cholangiopancreatography extraction (ERCP) and it was only after failure of this therapeutic option that we adopted the open surgery.
Every surgeon should know that metal clips can migrate and cause serious iatrogenic complication for an initially benign affection. This Complication can be preventable by the use of absorbable materials in contact with the bile duct.
Keywords: Laparoscopic cholecystectomy; Endoclips Migration; Common bile duct
Introduction
Endoclips migration into Common Bile Duct (CBD) after Laparoscopic Cholecystectomy (LC) is a rare iatrogenic complication unlike bleeding and bile duct trauma. Its exact incidence and physiopathological mechanism are also unknown [1,2]. Until today, very few sporadic cases have been reported in the world literature. The clinical manifestations are related to biliary obstruction, stenosis, choledocholithiasis, acute pancreatitis and cholangitis [3].
We report a new case of cholestatic jaundice related to the metal endoclips migration into CBD with literature data reviewing.
Case Report
A 59-year-old woman presented with recurrent epigastric abdominal pain and intermittent cholestatic jaundice for two weeks. Her medical history included laparoscopic cholecystectomy performed for chronic lithiasis cholecystitis six months previously. The surgery was difficult in an inflammatory environment on the operative report. The patient’s postoperative course was uneventful and the histology showed chronic cholecystitis without any signs of malignancy. Physical examination revealed moderate tenderness in the Right-upper quadrant of the abdomen, generalized itchiness, conjunctival jaundice with dark urine and discolored stools. There was no fever. Laboratory analysis revealed elevated direct bilirubin to 25 mg/dl (normal up to 5); mildly elevated liver transaminase levels with aspartate transaminase of 180 IU/l (normal up to 34) and alanine transaminase of 260 IU/l (normal up to 55); moderate cholestasis with alkaline phosphatase of 306 IU/l (normal up to 150) and gamma-glutamyl transferase of 160 IU/l (normal up to 36); C-reactive protein of 22mg/l (normal up to 5). Leucocytes, Serum amylase and lipase were normal. Abdominal ultrasound showed intra and extra hepatic ducts dilatation without obstacle characterization. Magnetic resonance imaging showed a dilatation of the intrahepatic bile ducts and the common bile duct upstream of a 15 mm hypointense cupiliform arrest probably indicating a calculus (Figure 1). Initially, the patient was approached by endoscopic retrograde cholangiopancreatography extraction (ERCP). After failure of the endoscopic removal, the patient was operated via the right subcostal laparotomy. Through a transverse choledochotomy (Figure 2), six metal clips impacted in the bile duct were successfully removed (Figure 3). Intraoperative cholangiography control objectified vacuity of the bile duct and the postoperative course was uneventful.
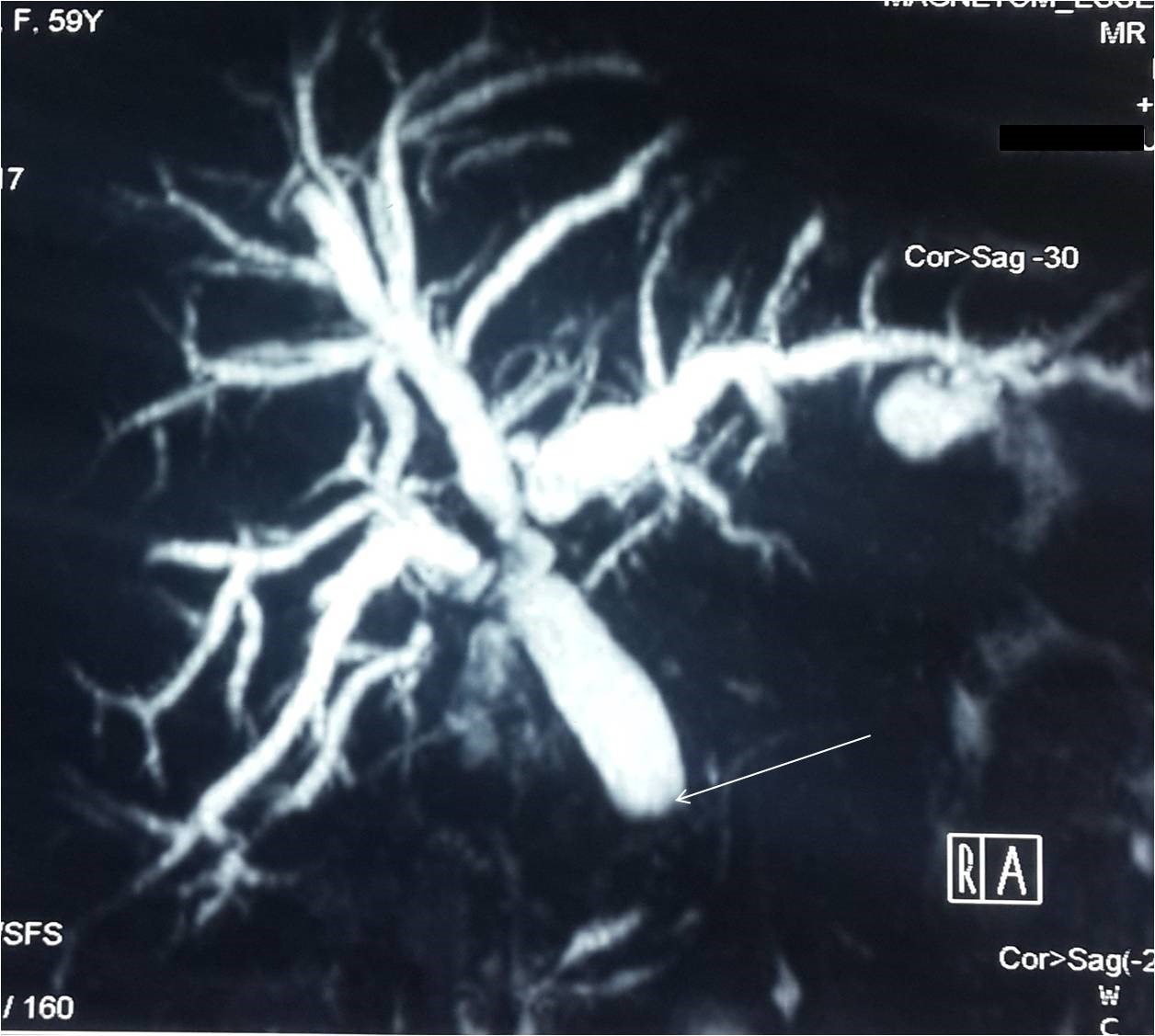
Figure 1: Magnetic resonance cholangiography (MRC) showing an important bile duct dilatation upstream of a cupiliform arrest in the distal common bile duct.

Figure 2: metal clips extracted from the common bile duct. Notice that in addition to the exaggerated number, there was an incomplete or an incorrect closure for most clips.
Discussion
Laparoscopic Cholecystectomy (LC) is a common procedure often using metallic or polymer clips to ligate the cystic artery and the cystic duct [4]. Intracholedochal non-absorbable endoclips migration (ECM) is a rare and unpredictable event after LC with fewer than 100 cases reported [3,5,6]. The first endoclips migration following LC was observed in 1992 by Onghena et al. [7]. It occurs between two weeks and up 35 years after biliary surgery [4].
The pathophysiological mechanism of ECM remains unclear. In fact, two main factors are implicated in the genesis of this complication: the first is the local infective process with the locoregional inflammation secondary to bile leak, cholecystitis, Cholangitis or pancreatitis. The second is the Poor surgical technique linked to ineffective closing (bile leak) or very tight closing clips (tissue necrosis), excessive use of clips on the cystic duct stump (more than four), and placement of clips flush with the common bile duct (erosion over time) [2,6,8].
The clinical presentation is that of any partial or total obstruction of the common bile duct causing abdominal pain, fever and jaundice. Endoclips migration can lead to several complications, such as choledocholithiasis, cholangitis, acute pancreatitis, choledocoduodenal fistula and duodenal ulcer which will reveal the diagnosis [4, 6]. Noninvasive morphological exploration can be made by ultrasound, CT scan, or Magnetic Resonance Cholangiopancreatography (MRCP) [6].
Endoscopic retrograde cholangiography with sphincterotomy and clip removal is the gold standard approach for treating Intracholedochal clips migration, it is effective in 85% of cases. Laparoscopique or open Surgical extraction should be reserved for unsuccessful endoscopic treatment [2,3,9,10].
The use of absorbable endoclips, maximal reduction of the applied clips, intracorporeal ligation of the cystic duct and artery, accurate placement of clips a little away from the bile duct wall, are useful measures to prevent this iatrogenic complication [10-12].
Conclusion
Intracholedochal endoclips migration is a rare but a serious late complication that should be evoked in front of any jaundice following laparoscopic cholecystectomy using metal clips. Even if few, the number of cases is increasing which should sound the alarm to switch exclusively to absorbable material. In fact, the application of absorbable clips or the use of ligature and intracorporeal knots can prevent or even avoid this complication.
Authors’ Contributions: NN and FM wrote the paper, AAA and AZ provided data; NN, AAA, and AZ revised the manuscript. All authors read and approved the final manuscript. NN is the guarantor of this manuscript.
Conflicts of Interest: The authors declare that they have no competing interests.
Grant information: The authors received no specific funding for this work.
Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
References
- Rawal KK. Migration of surgical clip into the common bile duct after laparoscopic cholecystectomy, Case Rep Gastroenterol. 2016; 10(3): 787-792.
- Mizouni A, Ammar H, Said MA, Harrabi F, Farhat W, Ghabry L, et al. Surgical clip migration following laparoscopic cholecystectomy: A rare cause of acute Cholangitis. Ann Med Surg, 2020; 59: 21-23.
- Diana APP, Marco AB, Alejandro MD, and Fernando AA. Titanium clip migration after cholecystectomy: original technique for laparoscopic transcystic extraction when endoscopic retrograde cholangiopancreatography fails. J Surg Case Rep, 2020; 9: 1-4.
- Daniel YLN, Wilson P, Michael DK. Clip as Nidus for Choledocholithiasis after Cholecystectomy—Literature Review. JSLS, 2020; 24(1): e2019.00053.
- Théophile G, Ugo SC, Valentin L, Pierre CO, David JB. Unfortunate adverse event resulting from clip migration after cholecystectomy, Surgery 2019; 165: 851-852.
- Sukanta R, Sankar PB. Endoclip Migration into the Common Bile Duct with Stone Formation: A Rare Complication after Laparoscopic Cholecystectomy, 2013; 17(2): 330-332.
- Onghena T, Vereecken L, Van den Dwey K, Van Loon C. Common bile ductforeign body; an unusual case. Surg Laparosc Endosc, 1992; 2(1): 8-10.
- Seung-Ik A, Keon-Young L, Sei JK, Eung HC, Sun KC, Yoon SH, et al. Surgical clips found at the hepatic duct after laparoscopic cholecystectomy: a possible case of clip migration. Surg Laparosc Endosc Percutan Tech, 2005;15(5): 279-282.
- Daniel S, Oren G, Baruch O, Yael K. Cholangitis caused by surgical clip migration into the common bile duct: a rare complication of a daily practice. BMJ Case Rep, 2020; 13(1): e231201.
- Hytham KSH, Anna F, Jamaleldin S, Sean MJ. Late biliary endoclip migration after laparoscopic cholecystectomy: Case report and literature review. Int J Surg Case Rep, 2020; 74: 205–208.
- Vui HC, Chee FC. Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg, 2010;14(4): 688-696.
- Francisco JG, Elias D, Angel L, Portela J, Piñon M. Migration of vessel clip into the common bile duct and late formation of choledocholithiasis after laparoscopic cholecystectomy. Am J Surg, 2011; 202(4): e41-43.

