Inducible Atrial Fibrillation and Myocardial Ischemia in a Veteran Amateur Runner
Massimo Bolognesi*
Department of Cardiology, Centre for Sports Cardiology, Italy
Received Date: 26/05/2021; Published Date: 09/06/2021
*Corresponding author: Massimo Bolognesi, Department of Cardiology, Centre for Sports Cardiology, Via Ungaretti 494 47521, Cesena (FC) Italy. Email: massimo.bolognesi@gmail.com, Mobile no: +39 0547645074
Abstract
Atrial fibrillation is the most common sustained cardiac arrhythmia and is associated with significant morbidity and mortality. Coronary artery disease frequently coexists with AF, and management of these associated conditions can be challenging. Endurance veteran athletes are a population at high risk to have episodes of paroxysmal atrial fibrillation. Herewith the author describes an original case of induced atrial fibrillation and myocardial ischemia during an Ex-ECG stress test in a veteran amateur runner.
Keywords: Atrial Fibrillation; Coronary Artery Disease; Veteran Athletes; Ex-ECG stress testing
Introduction
AF is a dangerous arrhythmia because it is associated with significantly impaired quality of life and exercise capacity, a five-fold increase in the risk of thromboembolic stroke, and a two-fold increase in overall mortality [1]. Environmental factors and state pathologies increase the risk of developing AF, including hypertension, heart failure, valvular heart disease, obesity, diabetes mellitus, and thyroid disease. Most of these risk factors are associated with Coronary Artery Disease (CAD), and clinically relevant concomitant CAD is present in 26-36% of patients with AF [2]. The population with Coronary Artery Disease (CAD), even silent coronary artery disease that suddenly has episodes of paroxysmal atrial fibrillation, is growing [3]. A strong correlation between the two conditions has been known, and the many common risk factors they share may play an essential role in their development. In addition, CAD may directly promote the onset and progression of AF by influencing re-entry formation, focal ectopic activity, and neural remodeling [4]. Indeed, AF is often an epiphenomenon of CAD that develops because of the following mechanisms and aspects: 1) atherosclerosis, 2) mismatch between blood supply and oxygen consumption, and finally 3) thrombosis. Coronary artery disease may have a unique clinical presentation through the appearance solely of paroxysmal atrial fibrillation induced by physical activity in the absence of the classic signs of angina pectoris or equivalent symptoms [5]. Herewith, the author wants to present a singular case of a veteran amateur runner who came to our sports cardiology center because he found unexplained alterations in heart rate during physical activity detected at the heart rate monitor. He did not report other symptoms like chest pain or tachycardia, but only a slight decline in his fitness.
Case Report
A 72-year-old male veteran amateur runner in apparent good health presented to our Center of Sports Cardiology for a medical checkup. He reported that his heart rate monitor detected sudden increases in heart rate during a regular, non-demanding running pace while also complaining of a general sense of fatigue. The athlete had previous medical examinations carried out for the eligibility to practice competitive athletics. He was taking antihypertensive drugs, including nebivolol, to control a form of uncomplicated arterial hypertension. The objective examination was regular, and so was the resting electrocardiogram (Figure 1). Then, the athlete proceeded to the cycle-ergometer exercise stress test. During the stress test, at the second step corresponding to 100 watts of external load, atrial fibrillation with high ventricular response started (Figure 2), which continued for over 20 minutes after stopping the stress test. The ECG showed clear signs of ventricular repolarization abnormalities, i.e., ST-segment depression by more than 2 mm with a horizontal and descending pattern on the inferior and precordial leads from V3 to V6. The athlete remained in an upright sitting position, hemodynamic stable (normal blood pressure) without chest pain or tachycardia symptoms. The athlete assumed 165 mg acetylsalicylic acid and 20 drops of Diazepam. After that, the athlete was accompanied in stable conditions walking autonomously to the emergency department for monitoring and cardiac examination. At the ED, the ECG resulted in the normal range, restoring normal sinus rhythm. The consultant cardiologist recommended only therapy with bisoprolol 2.5 mg (bis in die) plus Ramipril 5 mg per day and Xarelto 150 mg (bis in die). He also planned echo stress after a few months and suggested a consultation for transcatheter catheter ablation. However, the athlete moved on to the cath lab for coronary angiography, as we were sure of the coexistence of a critical multi-vessel coronary artery disease. Indeed, the coronary angiography showed a multi-vessel CAD(Figure 3) treated first with angioplasty for Ostial D1 significant stenosis. Also, the athlete underwent angioplasty plus DES implantation for the obstruction of the proximal CX coronary artery. Only moderate stenosis on the mid-IVA plus critical distal stenosis did not have any revascularization procedure. The athlete remained in good condition.
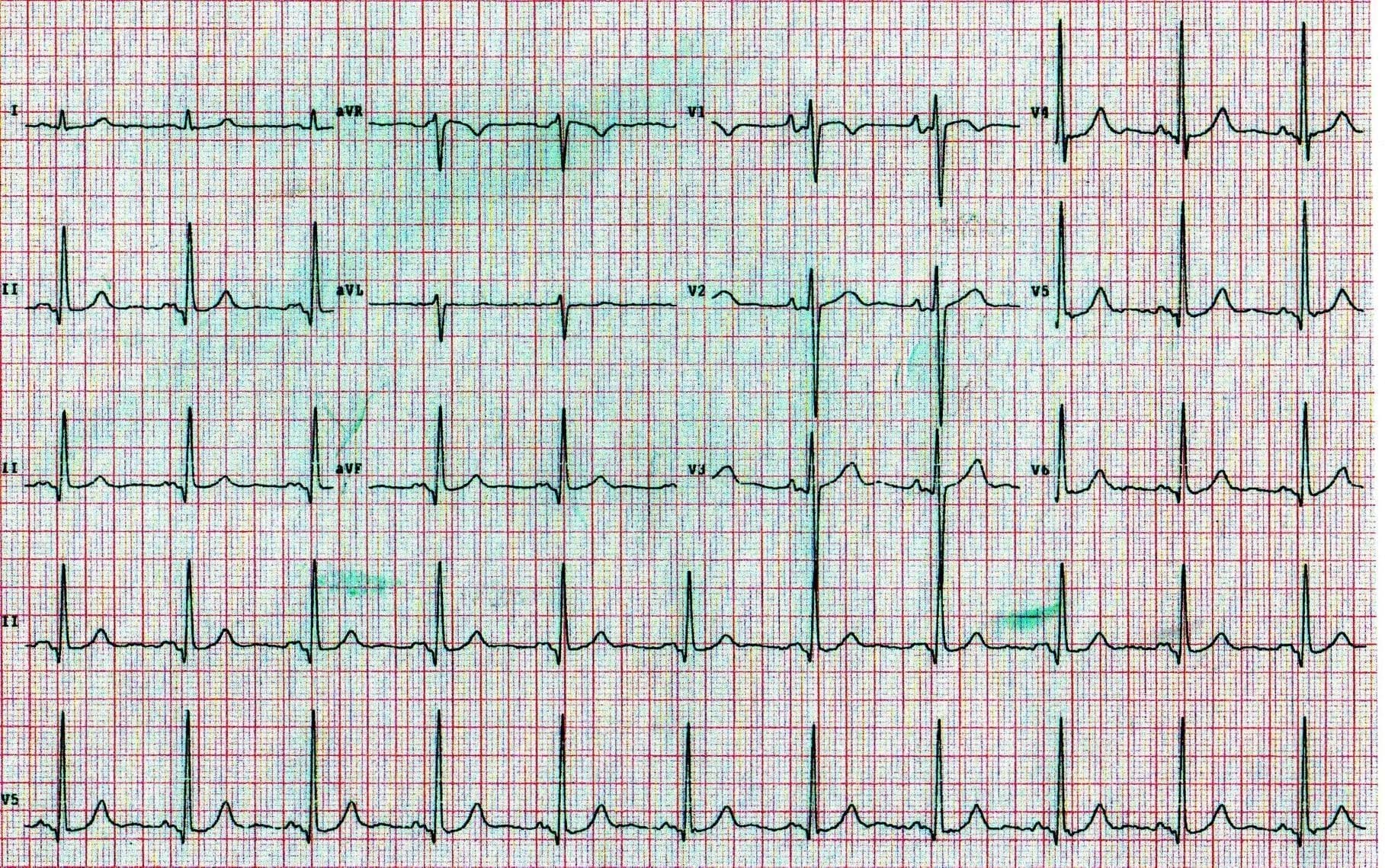
Figure 1: Shows the resting normal ECG
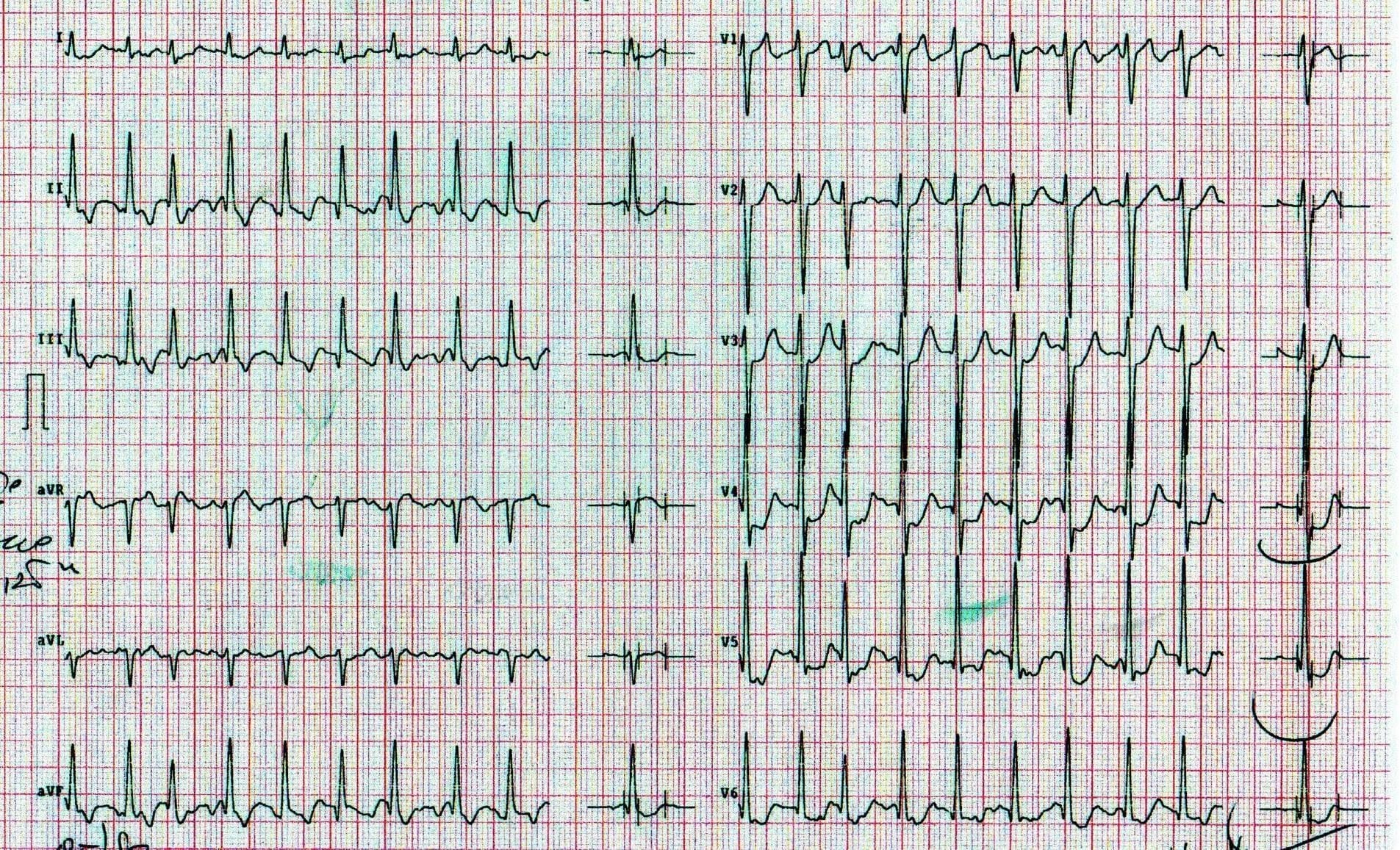
Figure 2: This ECG tracing recorded during. The Ex-ECG stress test shows atrial fibrillation with high ventricular response and marked ST-segment depression in the inferior and precordial leads from V3 to V6.
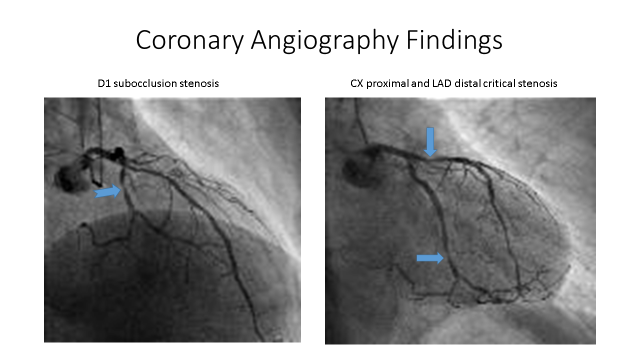
Figure 3: Show the coronary angiography findings.
Discussion
Atrial fibrillation is the most frequent arrhythmia in the general population and Master and veteran athletes, to the extent that its incidence has increased 4-5 times in recent years [3]. Considering the multiple cardiovascular risk factors, there is a risk of having AF among patients over 55 [6]. In parallel, many of these subjects are more likely to have subclinical coronary artery disease [4]. Although a 43 series of studies have extensively demonstrated the objective relationship between CAD and AF. The underlying mechanisms are not fully understood. Indeed, common risk factors for CAD and AF can provide enough elements to connect the two diseases. This case report is symbolic and significant because it offers many exciting teaching points for young doctors and practicing sports cardiology. The learning points concern the following aspects:
- The coexistence of CAD and AF inducible by stress test in Master's
- In veteran athletes, the silent ischemic heart disease is unmasked by Ex-ECG stress testing (i.e., subjects over 60).
- The inducible myocardial ischemia manifests itself instrumentally with the appearance of marked ST-segment depression in the first step of the stress test with the external workload. Then it gradually decreases until it disappears with the interruption of physical effort even in the continuity of the elevated ventricular response due to paroxysmal atrial fibrillation;
- in such cases, it is necessary to proceed immediately by subjecting the veteran athletes to diagnostic coronary angiography for the well-founded suspicion of CAD;
- not granting eligibility for competitive sport and suspending these type of athletes from any competition and training;
- Silent myocardial ischemia is frequent in veteran amateurs who practice endurance
Of note, this case report sheds light on the strategies to break the cycle of the two diseases, which may be fundamental to treat these patients and optimize the benefits.
Conflict of interest
I certify that there is no actual or potential conflict of interest concerning this article.
References
- Camm, AJ, P Kirchhof, GY Lip et al. Guidelines for the management of atrial fibrillation: the task force for managing atrial fibrillation of the European Society of Cardiology (ESC). Europace 2010; 12: 1360-1420.
- Nieuwlaat, R, A Capucci, AJ Camm et al. Atrial fibrillation management: a prospective survey in ESC member countries: The Euro heart survey on atrial fibrillation. Eur. Heart
- 2005; 26: 2422– 2434.
- Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50-year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. The Lancet 2015; 386: 154-162.
- Aronow WS, Ahn C, Mercando AD, and Epstein S. Correlation of atrial fibrillation, paroxysmal supraventricular tachycardia, and sinus rhythm with incidences of new coronary events in 1,359 patients, mean age 81 years, with heart disease. Am J Cardiol 1995; 75: 182-184.
- Wan H, Yang Y, Zhu J, Shao X, Wang J, Huang B, and Zhang H. The prognostic effects of ventricular heart rate among patients with permanent atrial fibrillation with and without coronary artery disease: a multicenter prospective observational study. Medicine (Baltimore) 2015; 94: e920.
- Weng LC, Preis SR, Hulme OL, Larson MG, Choi SH, Wang B, et al. Genetic Predisposition, Clinical Risk Factor Burden, and Lifetime Risk of Atrial Fibrillation. Circulation 2018; 137: 1027-1038.

