Right Internal Carotid Artery Thrombectomy with Microsurgical Endarterectomy
Adrian BODIU*, Danu GLAVAN, Andrei PECIUL, Vlad TCACI, Roman SMOLNITCHII, Doina ROPOT, Alexandra CONDREA
Institute of Emergency Medicine, Chisinau, Republic of Moldova
Department of Dentistry, University of the West of Santa Catarina, Brazil
Received Date: 06/05/2021; Published Date: 15/05/2021
*Corresponding author: Adrian BODIU, Institute of Emergency Medicine, Chisinau, Republic of Moldova, Nicolae Testemitanu State University of Medicine and Pharmacy, Chisinau, Republic of Moldova. Address: Republic of Moldova, Chisinau, Institute of Emergency Medicine, Toma Ciorba, 1 street. E-mail: adicbodiu@gmail.com, Mobile: +37369054868
Abstract
Tandem lesions are the cause of acute ischemic stroke in one third of stroke patients. It is related with more severe long-term consequences and raises questions about the approach of these patients. We present the case of a 54 years old male patient with acute ischemic stroke with tandem lesion in right internal carotid artery and M1 segment of right middle cerebral artery, having the contralateral internal carotid artery occluded.
Keywords: Stroke; Tandem lesion; Thrombectomy; Endarterectomy
Introduction
Tandem lesions occur in almost 30% of anterior circulation acute ischemic stroke (AIS) [1]. Patients with tandem lesions have poorer outcomes than patients with isolated intracranial lesions, with bigger rates of disability and death [2]. Optimal management of carotid lesions in this group of patients during endovascular thrombectomy is still controversial [3].
Case Report
Patient, male, 54 years old, was admitted to our hospital on 26.04.2021 with right middle cerebral artery (MCA) AIS with left hemiparesis,
The patient's complaints: left side weakness and numbness, facial asymmetry and dizziness.
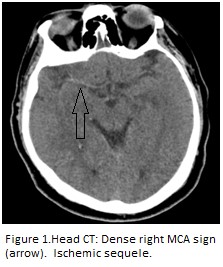
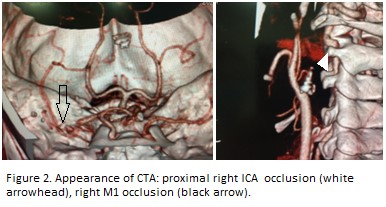
History: Sudden onset at 9 a.m., while working around the house, the above-mentioned complaints appeared. The 112 service was requested, the patient transported to the Institute of Emergency Medicine from Chisinau with the diagnosis of acute stroke. In the emergency room he was examined by neurologist: National Institutes of Health Stroke Scale (NIHSS) 5 points, central type left facial paresis, mild dysarthria, left mild hemiparesis. Blood tests, brain Computer Tomography (CT) (Figure 1) and cerebral CT angiography (Figure 2) performed.
For several years he has been suffering from hypertension. He had a left MCA AIS in 2020. Left Internal Carotid Artery (ICA) stenting with subsequent occlusion. Cerebral CT angiography in January 2021 revealed right ICA 65% stenosis, left ICA nonfunctional stent occlusion. He was on treatment with Clopidogrel 75 mg, Aspirine 75 mg, Rosuvastatin 10 mg. A few days ago, he stopped the treatment.
Approach: Intravenous systemic thrombolysis was started. After thrombolysis patient had negative dynamics with worsening of paresis and drowsiness. NIHSS score at that moment- 15 points. The patient was transferred to the angiography room for endovascular treatment. On DSA severe preclusive stenosis was found in proximal right ICA. Balloon angioplasty with 4.0X40 mm balloon was performed with a residual stenosis of about 80%. At this time patient improved clinically with a NIHSS score of 4 points and, at repeated angiography, permeabilization of right M1 segment was noted with a TICI score 2B. Considering this, we decided to stop the intervention. The patient was transferred to Stroke unit for further evaluation.
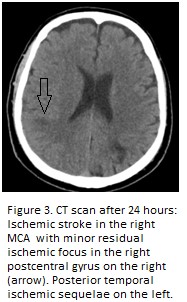
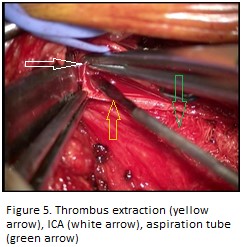
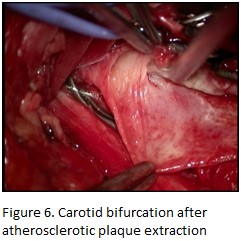
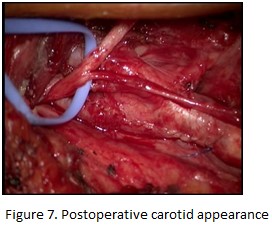
On the second day, repeated head CT scan was performed (Figure 3). Also, carotid duplex was performed. It revealed occlusion with thrombosis of right ICA. Considering the fact that left ICA occluded after stenting last year and the risk of hemorrhagic transformation on dual antiplatelet, we proposed thrombectomy with microsurgical endarterectomy to patient and his relatives. ICA thrombectomy with microsurgical endarterectomy was performed after patient consent. It revealed severe stenosis with unstable partially calcified plaques with distal thrombi (Figures 4-7). The procedure was associated with thrombus extraction from ICA, until obtaining the retrograde flow, with good technical result.
After the procedure, the patient was given Low Molecular Weight Heparin for two days, after that it was passed on Clopidogrel.
NIHSS at the seventh day after stroke onset - 2 points, modified Rankin scale- 1 point.
Postoperative diagnosis: Right MCA AIS with mild left sided hemiparesis. Intravenous thrombolysis. Right ICA percutaneous transluminal balloon angioplasty (26.04.2021). Acute right ICA occlusion with thrombosis. Right ICA thrombectomy with microsurgical endarterectomy. Chronic left ICA in-stent occlusion.

Discussion
Right ICA thrombectomy with microsurgical endarterectomy was a good choice in this patient poststroke management, taking into consideration that the left ICA was occluded after stenting and anterior circulation was supplied only by collaterals. It also allowed us to reduce the risk of hemorrhagic transformation, by avoiding double antiplatelet therapy. Our approach has been effective so far. We will follow this patient further.
References
- Feil, Katharina, et al. "Tandem Lesions in Anterior Circulation Stroke: Analysis of the German Stroke Registry–Endovascular Treatment." Stroke 2021; 52(4): 1265-1275.
- Kim, Yo Sik, et al. "Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion." Stroke 2005; 36(4): 869-871.
- Poppe, A. Y., et al. "Tandem carotid lesions in acute ischemic stroke: mechanisms, therapeutic challenges, and future directions." American Journal of Neuroradiology 2020; 41(7): 1142-1148.

