Endometrial Stromal Nodule
Şerife Özlem Genç, Aliye Nigar Serin, Burcu Yılmaz
Aksaray University, Department of Obstetrics and Gynecology, Turkey
Karamanoglu Mehmetbey University, Department of Gynecology Obstetrics, Karaman, Turkey
Karamanoglu Mehmetbey University, Department of Pathology, Turkey
Received Date: 01/05/2021; Published Date: 07/05/2021
*Corresponding author: Alireza khoshnevisan, MD. Karamanoglu Mehmetbey University, Department of Gynecology Obstetrics, Karaman, Turkey. Phone number: +90 530 580 3092, Postal code: 70200, E- mail: nserin85@hotmail.com, Orcid ID: https://orcid.org/0000-0003-0544-1115
Abstract
The Endometrial Stromal Nodule (ESN) is the rarest subtype of endometrial stromal tumors (ESTs) that’s why experience with ESN is limited. ESN could mimic highly cellular leiomyomas, usually seen in the premenopausal age. Patients present with nonspecific symptoms such as abnormal bleeding, lower abdominal pain, or maybe asymptomatic. Our patient was 46 years old women suffering from abnormal uterine bleeding and lower abdominal pain and had no desire to protect fertility. The preoperative diagnosis of ESN is very difficult. Also, no specific imaging is defined for the ESN in ultrasound or MRI examination. ESN is usually misdiagnosed as uterine fibroids, interstitial ectopic pregnancy, or stromal hyperplasia. Macroscopically, these tumors are classically well-circumscribed, solitary, encapsulated. In a curettage specimen, the distinction between an ESN and a low-grade endometrial stromal sarcoma is almost impossible, unless the tumor is too small, and the margins can be fully evaluated. In conclusion, ESN is a rare subtype of endometrial stromal sarcomas, but there is nothing to afraid of if you do the hysterectomy. So, it is important to diagnose preoperatively especially in young nulliparous women who desire to preserve fertility. Clinical presentation is nonspecific and there is no preoperative imaging that can completely rule out malignancy. It is necessary to develop new diagnostic methods or new treatment options to protect the uterus.
Keywords: Endometrial stromal tumor; Endometrial stromal nodule; Leiomyoma; Highly cellular myoma; Uterine sarcoma
Introduction
Endometrial Stromal Tumors (ESTs) are very rare mesenchyme tumors, and the Endometrial Stromal Nodule (ESN) is the least common [1]. 2014 WHO classification divides ESTs into four groups: Endometrial stromal nodule, low-grade endometrial stromal sarcoma, high-grade endometrial stromal sarcoma, and undifferentiated uterine sarcoma [2]. However, the ESN is difficult to diagnose because of its similarity to low grade endometrial stromal sarcomas [3]. The ESN is noninvasive and clinically benign type of ESTs.
There is limited information about the ESN because of its rarity. The definitive diagnosis of the ESN depends on an attentive examination of the tumor margin after hysterectomy.
Case Report
We report a 46-year-old woman as a case who had abnormal uterine bleeding and lower abdominal pain. Transvaginal ultrasound scan revealed a corpus luteum cyst in the right ovary and well-circumscribed fibromas; the bigger one of which was 6x6 cm. The intrauterine device had been applied to the patient for the treatment of abnormal bleeding but failed. After that, the endometrial curettage examination showed late proliferative endometrium. As she had no fertility desire, she underwent a hysterectomy and bilateral salpingo-oophorectomy because of menometrorrhagia. After histopathological examination, was defined as an endometrial stromal nodule.
On macroscopic examination, in the sections of the uterus, 5 nodules, the largest of which was 6 cm and the smallest of which was 0,5 cm in diameter, were detected. As in this case, the biopsy may be negative when the tumor is not associated with the endometrium. The largest nodule was intramural with well-circumscribed and 6x6x5 cm in diameter. Its cut surface was fleshy, tan, focal orange colored and had a fibrillary configuration.
Histomorphological findings showed that nodule has a non-infiltrative border and consists of uniform small cells with oval-round, blue, basophilic nucleus with chromatin which is finely granular, has an indeterminate nucleolus, and a scant cytoplasm (Figure 1,2). Tumor cells expressed diffuse CD10 and weakly SMA positivity (Figure 3).
The lesion was in cellular morphology and there was no cellular atypia, mitosis or necrosis. Hyalinized smooth muscle differentiation which expressed desmin and caldesmon (Figure 4, 5) and MTK positivity showing starburst morphology was observed in the focal areas (Figure 6). Starburst pattern is composed of smooth muscle differentiation with central hyalinisation and radiating collagen bants at the periphery encircle round cells (Figure 2). There was no lymphatic, vascular or myometrial invasion.
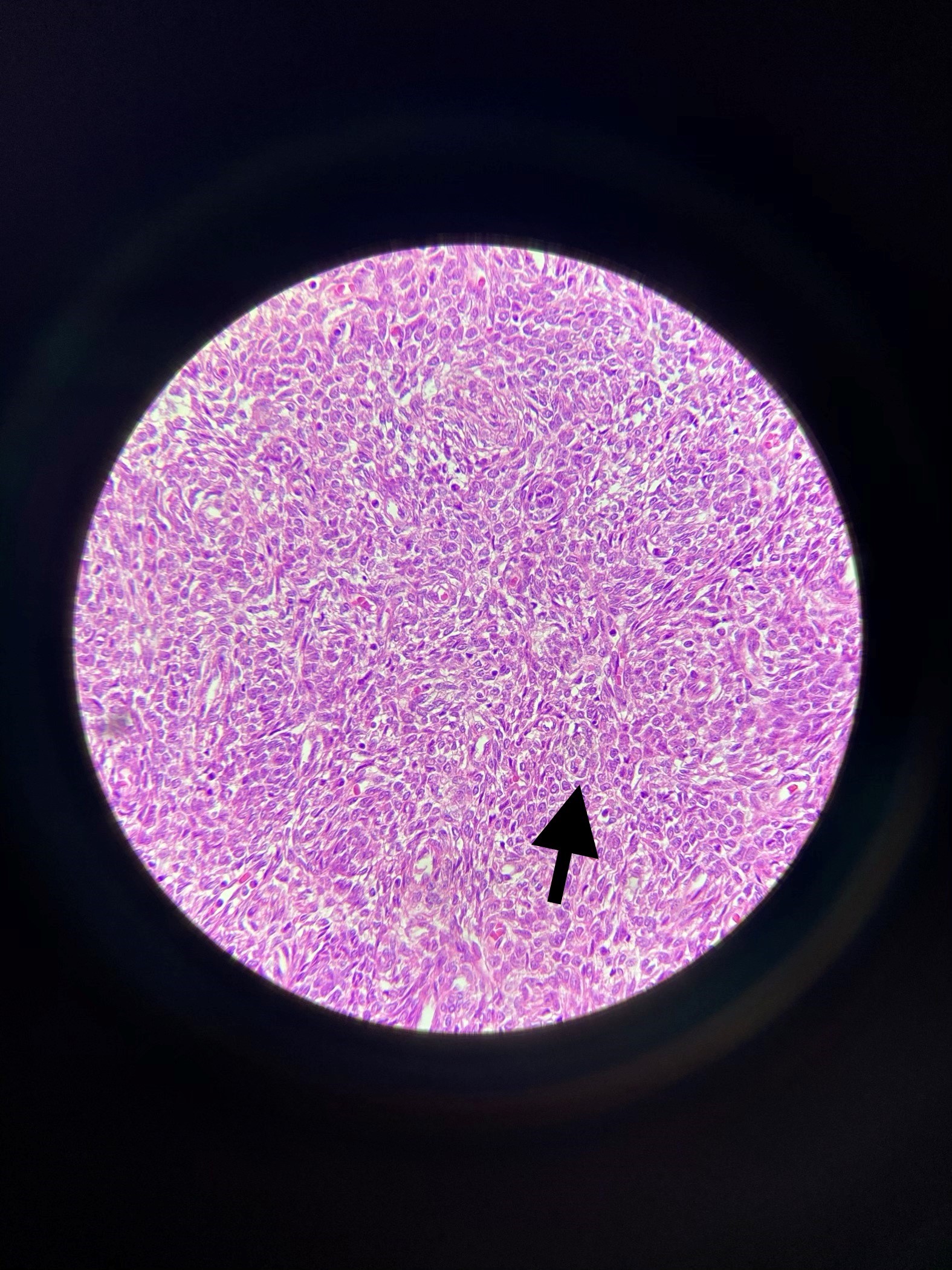
Figure1: Diffuse growht of uniform small cells that resemble proliferative-phase endometrial stroma. (x400, H&E)
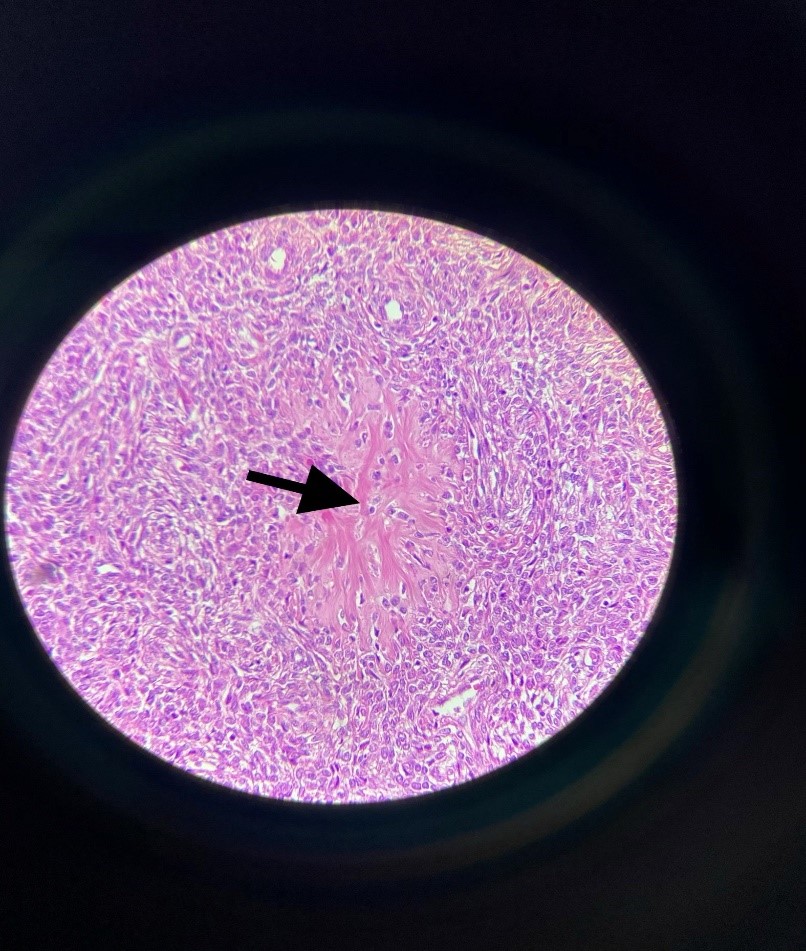
Figure 2: Smooth muscle differentiation displaying a starburst morphology (arrowed). (x400, H&E).
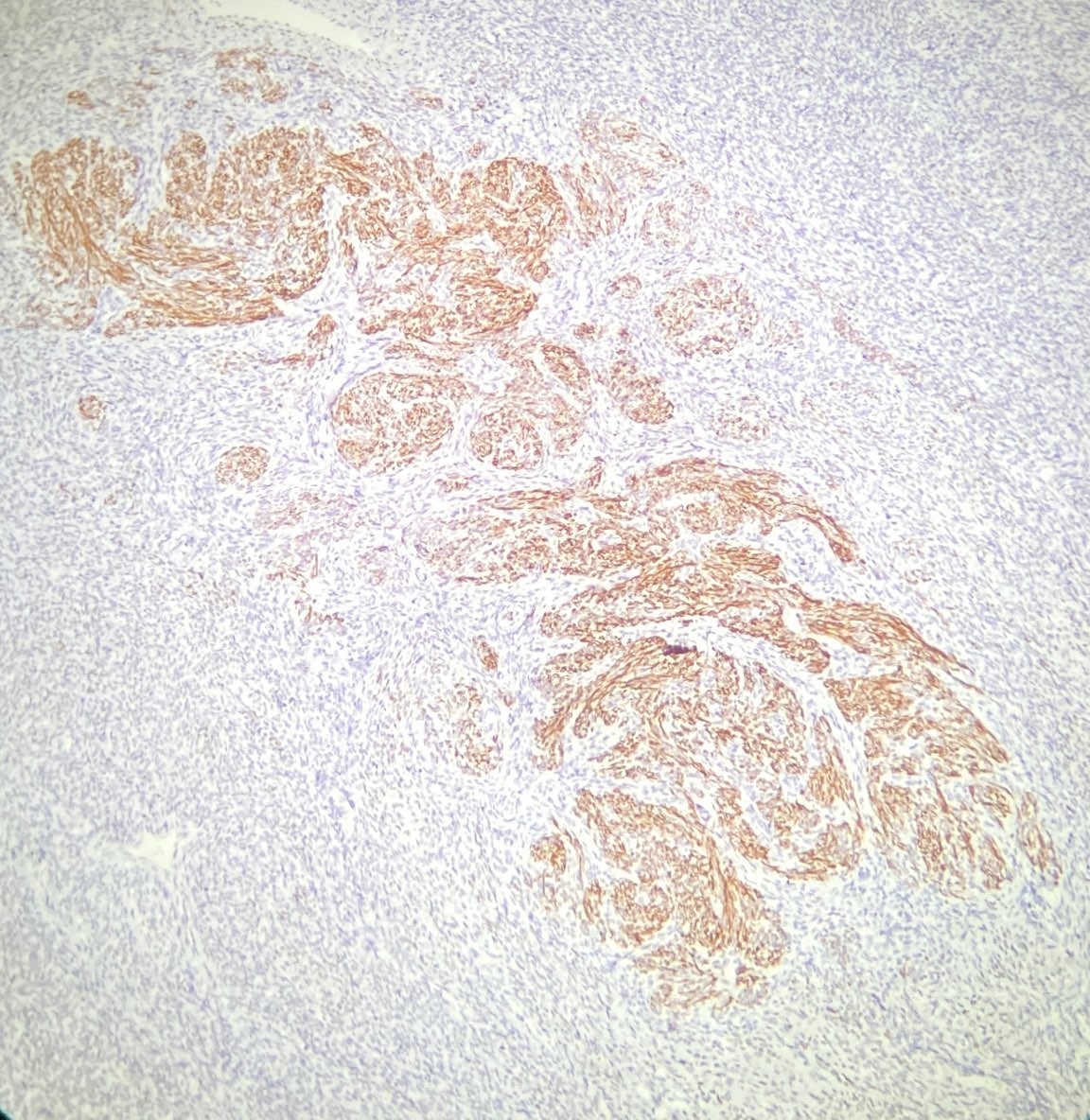
Figure 3: CD10 shows mostly positivity in uniform cells and negativity on the center which displays smooth muscle differentiation called starburst morphology (x200, CD10).

Figure 4: Focal smooth muscle differantiation shows typical Desmin expression, serially cut section of CD10 immunostaining (x200, Desmin)
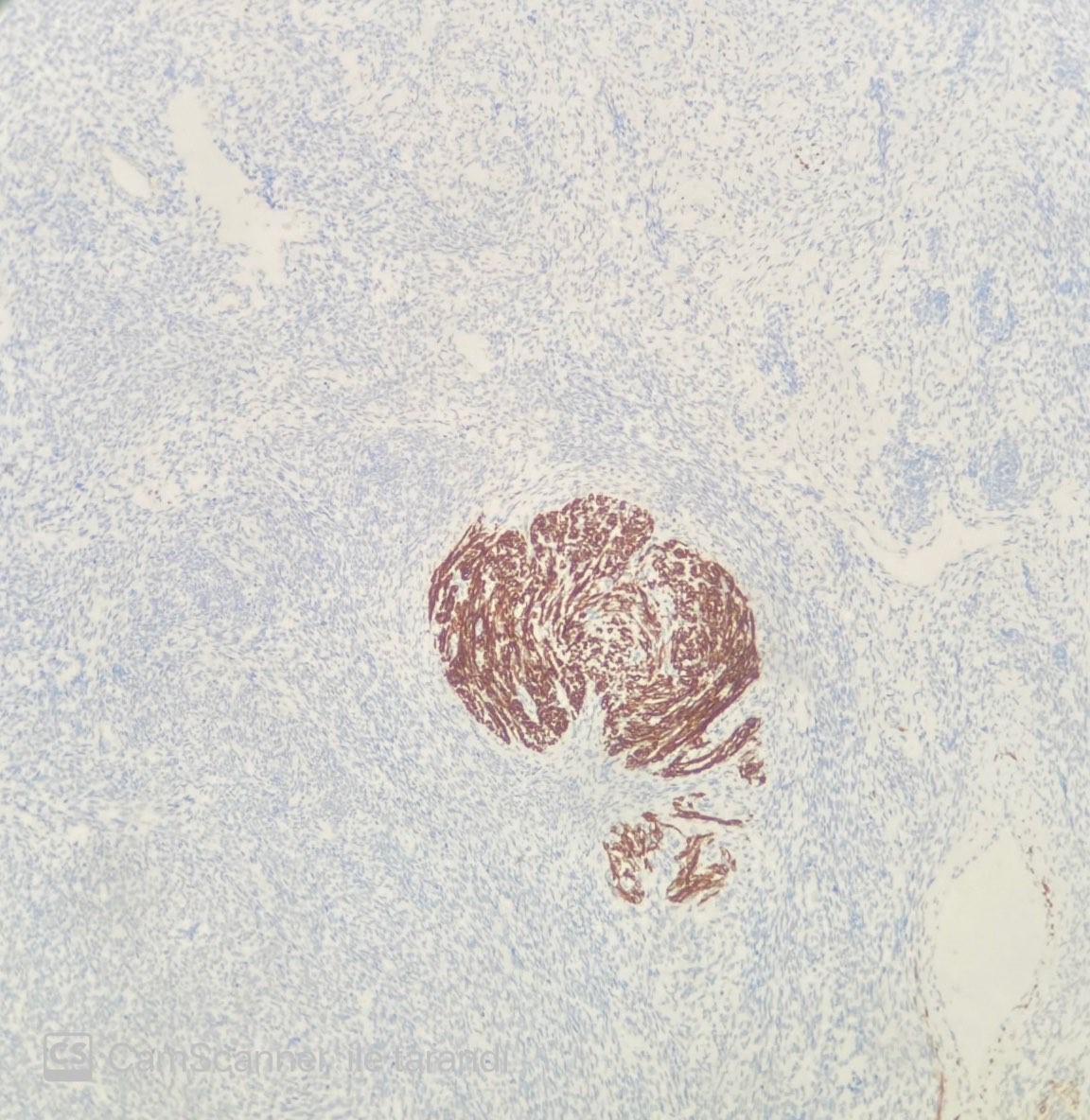
Figure 5: Caldesmon shows smooth muscle differantion of starburst morphology. (x200, Caldesmon)
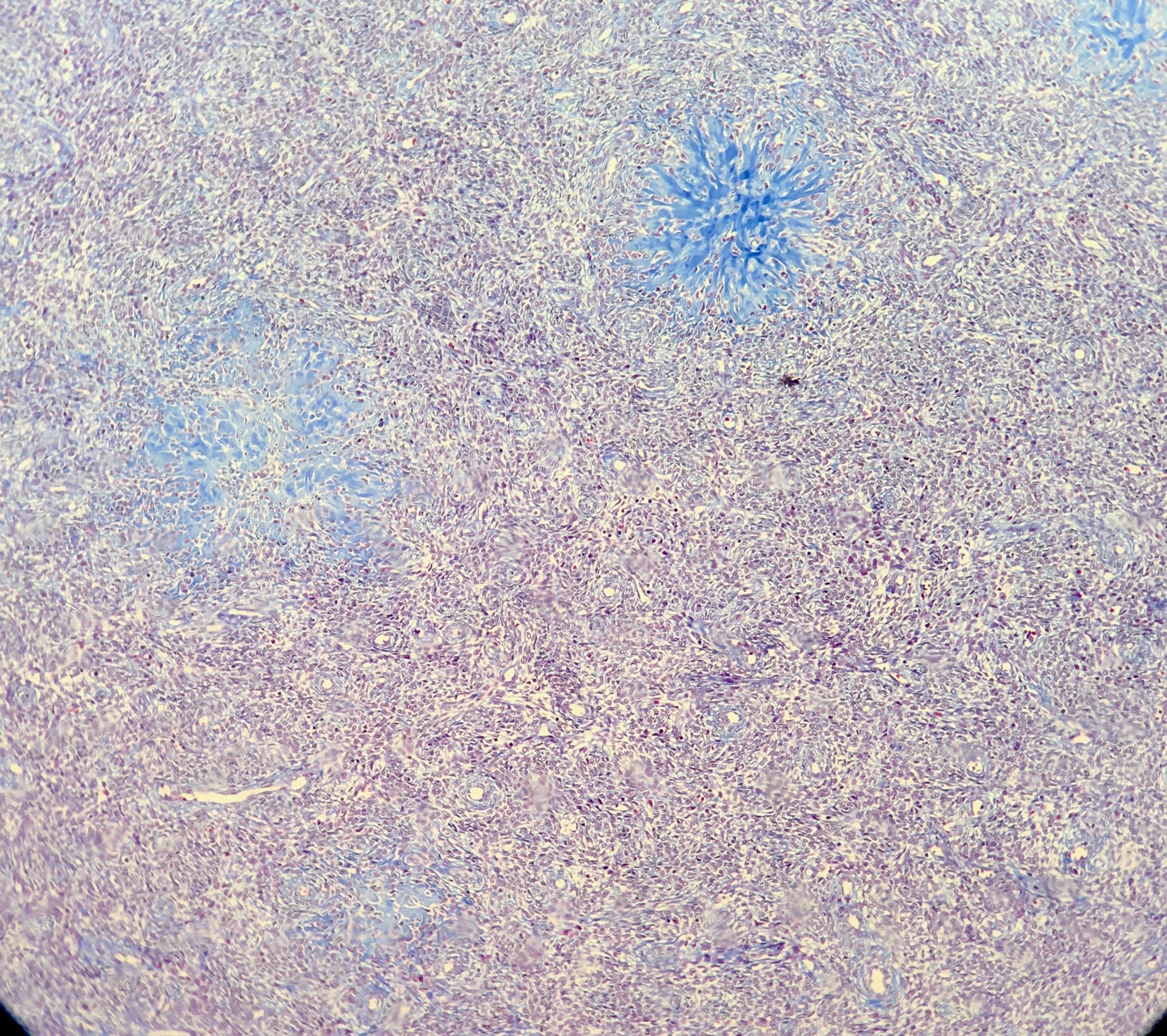
Figure 6: MTK revealed starburst morphology (X200, MTK
Discussion
Experience with Endometrial Stromal Nodules (ESNs) is limited due to less than 2% of all uterine neoplasms and the literature on these lesions is inadequate. There is only one large series of ESNs which is reported with 60 cases in 1981 [4]. Recently, Dionigi published a series of 50 cases with endometrial stromal tumors which includes only 4 ESNs [5].
ESN usually occurs at premenopausal age, but can be observed over a wide age range, such as 23 to 86 years [5]. Our case was a 46-year-old perimenopausal woman and there was no need to protect fertility.
The preoperative diagnosis of ESNs is very difficult. Patients may have abnormal bleeding, lower abdomen, or pelvic pain. However, they can sometimes be asymptomatic [5]. Our patient had lower pain and abnormal vaginal bleeding. Also, no specific medical imaging is defined for an ESN in ultrasound or MRI examination so postoperative pathology is essential for the diagnosis of an ESN. The ESN is usually misdiagnosed as uterine fibroids, interstitial ectopic pregnancy or stromal hyperplasia. These tumors are well-circumscribed, solitary, encapsulated and usually found in myometrium with a size of 1 to 22 cm and an average size of 7 cm, but may also be located across endometrium as a polypoid mass [3,4]. In this case, the transvaginal ultrasound showed a few well-circumscribed masses, the biggest of which one was 6*6cm, which might be fibroids. ESN cases are generally diagnosed preoperatively as leiomyoma and adnexal mass [6]. Our preoperative diagnosis was leiomyoma in line with the literature, but postoperative pathology confirmed the ESN. In an endometrial biopsy material, the differences between an ESN and a low grade endometrial stromal sarcoma are almost impossible unless the tumor is too small, and the borders are fully evaluated in our case endometrial biopsy was diagnosed as late proliferative endometrium.
Differantial diagnosis of endometrial stromal nodules completely depends on the histopathological findings. Multiple preparate examination and serial cut sections must be performed. These stromal nodules have expansile, non-infiltrative margins with adjacent myometrium [7]. Lymphatic and vascular invasion is absent. Immunhistochemical expression includes CD10 positivity, SMA, caldesmon and desmine negativity (or weakly positivity).
In our case, the tumor expresses diffuse CD10. Only starburst pattern showed Desmin and Caldesmon positivity. The nodule was immunonegative with desmine and caldesmon in the regions other than these starburst areas.
Although ESNs are benign tumors, hysterectomy is the gold standard for total histological examination of the uterus to rule out malignancy [8]. On the other hand, Schilder et al. published a case report involving a successful hormone therapy of the endometrial stromal nodule to maintain fertility in a young nulliparous woman [9]. As a result, local excision and hormonal therapy can be successful in women of reproductive age who want to maintain fertility. Hysteroscopy can then be used to evaluate the full myometrial interface and to monitor tumor growth [10].
In conclusion, it is not easy to diagnose the ESN preoperatively because of its similarity to cellular leiomyoma. If the postoperative result shows the ESN, the prognosis is excellent. The gold standard is to perform hysterectomy in patients diagnosed with the ESN. This rare tumor should be considered among the differential diagnoses in patients with irregular vaginal bleeding and uterine fibroma. Since there is a few ESN in the literature, lots of studies are needed, which may improve the knowledge about the preoperative diagnosis or treatment and surgery options.
Consent to Participate
The written informed consent was obtained from the patient to publish case characteristics.
Consent for Publication
Not applicable.
Availability of data and materials statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
No potential conflict of interest was reported by the author(s). The authors alone are responsible for the content and writing of the article.
Funding
None
References
- Fdili Alaoui FZ, Chaara H, Bouguern H et al. Endometrial stromal nodule: report of a case. Case Reports in Medicine, vol. 2011, Article ID 260647, 5, 2011.
- Ali RH, Rouzbahman M. J Clin Pathol 2015; 68: 325–332.
- Manuel V, Dinato FJ, Gutierrez PS et al. Cardiac metastatic endometrial stromal sarcoma 17 years after hysterectomy. J Card Surg. 2017; 32(10): 636‐638.
- Tavassoli FA, Norris HJ. Mesenchymal tumours of the uterus. VII. A clinicopathological study of 60 endometrial stromal nodules. Histopathology. 1981; 5: 1–10.
- Dionigi A, Oliva E, Clement PB, et al. Endometrial stromal nodules and endometrial stromal tumors with limited infiltration: a clinicopathologic study of 50 cases. Am J Surg Pathol. 2002; 26: 567–581.
- Elagoz S, Kıvanc F, Aker H et al. Endometrial stromal tumors—a report of 5 cases. Aegean Pathology Journal, 2005; 2; pp. 140–145.
- An, G. Ruan, X.Y. Xie et al. Endometrial stromal nodule: report of 8 cases and literature review. European Journal of Gynaecological Oncology, 2020, 41(3): 332-338.
- Ferreira J, Félix A, Lennerz JK, et al. Recent advances in the histological and molecular classification of endometrial stromal neoplasms. Virchows Arch. 2018; 473(6): 665-678.
- Schilder JM, Hurd WW, Roth LM, et al. Hormonal treatment of an endometrial stromal nodule followed by local excision. Obstet Gynecol 1999; 93: 805–807.
- Vilos GA, Harding PG, Sugimoto AK, et al. Hysteroscopic endomyometrial resection of three uterine sarcomas. J Am Assoc Gynecol Laparosc 2001(8): 805–807.

