COVID-19 with Negative RT-PCR? The Challenge of a Hospital Occupational Health Department
Pedro Miguel Matos*, Paulo Pinho, Pedro Guedes, Francisco Carvalho, Nuno Saldanha, Pedro Norton
Occupational Health Department, Centro Hospitalar Universitário de São João. Porto. Portugal
Received Date: 31/03/2021; Published Date: 12/04/2021
*Corresponding author: Pedro Miguel Matos, Occupational Health Department, Centro Hospitalar Universitário de São João. Porto. Portugal, 4200-319 Porto, Email: pedromadeiramatos@gmail.com, +351 225 512 100
Abstract
We report a case that exemplifies the Occupational Health Department´s challenge in managing the COVID-19 pandemic among healthcare workers in a level III hospital in Portugal. It refers to a woman with clinical manifestations of acute respiratory infection and computed tomography of the chest showing ground-glass opacities in the left lower lobe that could translate COVID-19 pneumonia. However, she performed various nucleic acids amplification tests for SARS-CoV-2 detection, which were all negative. Despite this, she received an indication from the medical team for work avoidance. Due to this dubious situation, she performed rapid and conventional serologic tests, both positive for SARS-CoV2 infection. With this report, we aimed to alert the urge and importance of well-defined action protocols for high clinical suspicion COVID-19 cases to prevent or limit intrahospital outbreaks
Keywords: COVID-19; Healthcare Worker; Occupational Health; Portugal.
Introduction
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) is the 2019 novel coronavirus that was first detected in China. It´s responsible for the COVID-19, the newest pandemic recognized by the World Health Organization (WHO) on the March 11th, 2020. The virus has rapidly spread, and on the March 18th, 2021, 120 268 427 confirmed cases and 2 659 802 deaths had been reported. The clinical spectrum of COVID-19 can vary from being asymptomatic to the development of serious complications that can potentially lead to death, such as pneumonia and acute respiratory distress syndrome [1,2].
Several diagnostic tools can be used for SARS-CoV-2 detection. So far, the gold-standard for the diagnosis of COVID-19 is the Nucleic Acids Amplification Tests (NAAT), which include the real-time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) [3]. Despite RT-PCR tests are highly specific, and the probability of false positives is low, false negatives are possible, and they are associated with swab type and time since symptoms onset. The likelihood of a false negative result increases as more time has passed since the beginning of symptoms. Performing a single test on someone who had symptoms ten days ago is associated with a 25% and 47% probability of a false negative result using nasopharyngeal and oropharyngeal swabs, respectively [4]. In patients with RT-PCR false negative results, to identify COVID-19 cases with higher sensitivity, a combination of exposure history, clinical symptoms, typical chest Computed Tomography (CT) imaging, and dynamic changes should be used [5]. Antigen-detecting rapid diagnostic tests target proteins produced by replicating virus in respiratory secretions. Compared to NAAT, they have a sensibility and specificity of ≥90% and 97%, respectively, and results are often available 15-30 minutes after its realization. They are particularly useful to respond to suspected outbreaks of COVID-19 in particular settings and where NAAT isn´t immediately available [3,6]. Serologic tests are other laboratory tools that are available to evaluate immunologic response to SARS-CoV-2 [3]. The immune response in COVID-19 is detected in the second week of disease, about 9 to 12 days after symptoms onset [7].
This case report demonstrates the Occupational Health Department´s (OHD) challenge at a level III hospital in Portugal to manage potential COVID-19 cases among Healthcare Workers (HW).

Figure 1: Chest computerized tomography showing ground-glass opacities in the left lower lobe with preferentially peripheral and basal distribution and an inflammatory aspect.
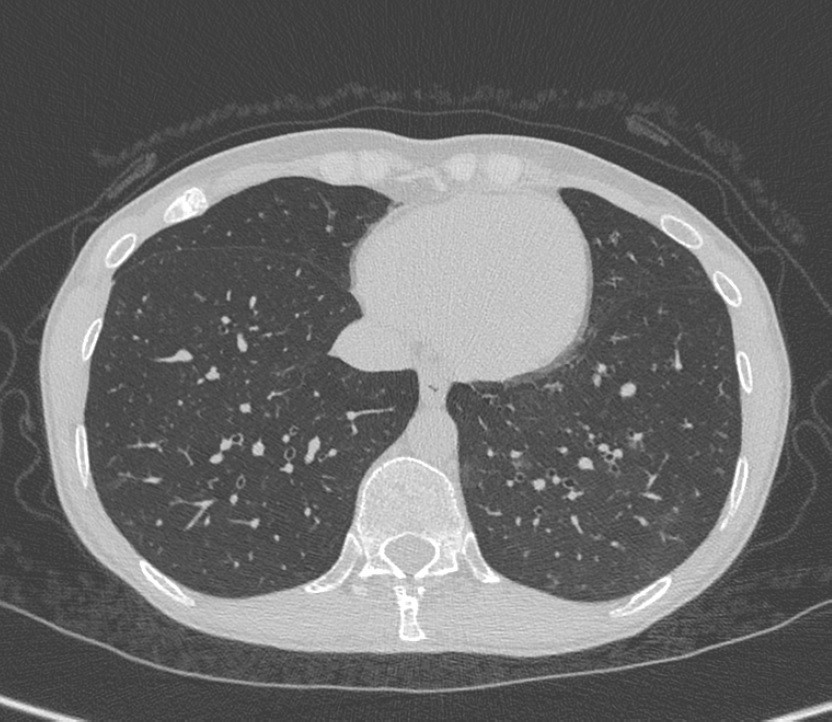
Figure 2: Chest computerized tomography showing the disappearance of almost all of the previously visible ground-glass opacities.
Case Report
A 42-years-old woman, HW in a level III hospital in Portugal, with a medical history of cigarette smoking, Helicobacter pylori gastritis, and nasal polyps, came to the OHD on December 2nd, 2020, with productive cough, muscle aches, intense fatigue, headache and fever (armpit temperature of 38oC) starting five days ago. After a medical evaluation, a RT-PCR SARS-CoV-2 test was performed, with the indication for work avoidance and self-isolation until the result is known, which was negative. However, due to persistent symptoms, she continued the self-isolation and, three days later, was admitted to the Emergency Department (ED), where were performed another RT-PCR SARS-CoV-2 test, which was negative, and a chest CT. The chest CT showed ground-glass opacities in the left lower lobe with preferentially peripheral and basal distribution and an inflammatory aspect, which may translate COVID-19 pneumonia (Figure 1). She was considered a probable case of COVID-19, and for that reason, she received the indication of the OHD to maintain work avoidance [8]. The symptoms did not improve, and on December 7th, she has repeated the RT-PCR for SARS-CoV-2, which was negative. On December 9th, she was admitted to the ED where were performed a laboratory study that showed a very slight increase of the C-reactive protein (5 mg/dL; normal range < 3 mg/dL); pneumococcal and legionella urinary antigen tests that were both negative and a normal chest radiograph. On December 15th, she returned to the OHD and was referred to an infectious disease specialist appointment for the next day. Here, she had a significant improvement of the symptoms. Due to the dubious situation, she performed a rapid serologic test that was positive for the presence of IgM and IgG for SARS-CoV-2 infection. Moreover, she repeated the chest CT with the disappearance of almost all of the previously visible ground-glass opacities (Figure 2). The next day, she performed a NAAT and antigen-detecting rapid diagnostic test for SARS-CoV-2 infection, which were both negative. Due to the difficulty in interpreting and valuing these findings, a conventional serology (Abbott SARS-CoV-2 CLIA IgG) was performed on December 18th, which was positive. The total time of work avoidance was 15 days.
Discussion
This case report exemplifies the challenge and difficulty inherent in managing the COVID-19 pandemic among HW of a level III hospital by the OHD. On the one hand, it is crucial that the OHD implements measures that minimize infection risk, including the correct use of personal and collective protection equipment. On the other hand, it is essential to develop a quick and effective intervention protocol developed by the OHD to stop the transmission of SARS-CoV-2 among HW and between HW and patients to prevent or limit a potential intrahospital COVID-19 outbreak.
In this particular case, despite the infection by SARS-CoV-2 has not been confirmed by NAAT, as there was a high clinical suspicion strengthened by the imaging evidence, the indication of the medical team was for job eviction. This decision was carefully considered, always having in mind the risk of precipitating an intrahospital outbreak in the case of permanence at work versus the hospital costs resulting from work avoidance, particularly with the possibility of the patient not having COVID-19. She repeated a chest CT eleven days later with evidence of the disappearance of almost all ground-glass opacities, which favors acute respiratory infection and not an interstitial lung disease. The HW performed a conventional COVID-19 serology (Abbott SARS-CoV-2 CLIA IgG) on the twenty-second day of symptoms, which was positive. This serological test has a specificity of 99.3% and a sensibility of 81.8% [9]. Even though the serology tests are not the gold-standard for the diagnosis of COVID-19, they are helpful to detect both active and past infections if performed within the correct timeframe, surpassing the failings of RT-PCR as a sole diagnostic method in surveillance because of its inability to detect past infection [10]. Moreover, clinical and radiological evaluations showed to be sufficiently accurate and reliable on the diagnosis of COVID-19 when there are repeated negative swabs [11]. Based on these facts, the decision was for work avoidance.
With this case report, we want to warn that all OHD should have well-defined action protocols for high clinical suspicion COVID-19 cases without NAAT confirmation to limit the spread of SARS-CoV-2 infection.
Conflicts of Interest
None
Grant Information
The authors received no specific funding for this work.
References
- World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020.
- European Centre for Disease Prevention and Control. COVID-19.
- Direção-Geral da Saúde (DGS). Estratégia Nacional de Testes para SARS-CoV-2. Norma no 019/2020 26/10/2020 atualizada a 26/02/2021.
- Wikramaratna PS, Paton RS, Ghafari M, Lourenço J. Estimating the false-negative test probability of SARS-CoV-2 by RT-PCR. Eurosurveillance. 2020; 25(50): 1–10.
- Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020; 296(2): E32–40.
- World Health Organization. Antigen-detection in the diagnosis of SARS-CoV-2 infection using rapid immunoassays: Interemim Guidance. 2020.
- Lou B, Li T-D, Zheng S-F, Su Y-Y, Li Z-Y, Liu W, et al. Serology characteristics of SARS-CoV-2 infection after exposure and post-symptom onset. Eur Respir J. 2020; 56(2): 2000763.
- Direção-Geral da Saúde (DGS). COVID-19: Definição de Caso de COVID-19. Norma no 020/2020 09/11/2020.
- Nicol T, Lefeuvre C, Serri O, Pivert A, Joubaud F, Dubée V, et al. Assessment of SARS-CoV-2 serological tests for the diagnosis of COVID-19 through the evaluation of three immunoassays: Two automated immunoassays (Euroimmun and Abbott) and one rapid lateral flow immunoassay (NG Biotech). J Clin Virol. 2020; 129: 104511.
- Winter AK, Hegde ST. The important role of serology for COVID-19 control. Lancet Infect Dis. 2020;20(7):758–759.
- Mirijello A, Zarrelli M, Miscio G, de Matthaeis A, Piscitelli P, Carbonelli C, et al. Diagnosis of COVID-19 in Patients with Negative Nasopharyngeal Swabs: Reliability of Radiological and Clinical Diagnosis and Accuracy Versus Serology. Diagnostics. 2021; 11(3): 386.

