Pulmonary Embolism Associated with Intracardiac Thrombus Complicating the Course of Behcet’s Disease:a Case Report
Soumia FAID*,Nuance Divine TCHILOEMBA TCHIBINDA *, Maryam NADIF, Lamyaa BAKAMEL , Sofia KADDAF, Christelle MPEMBA RAPAGA , Ilyass ASFALOU , Zouhair LAKHAL, Aatif BENYASS
Intensive Care Unit, Ibn Sina University Hospital Center, Mohammed V Military Hospital, Morocco.
Non-Invasive Exploration department, Ibn Sina University Hospital Center, Mohammed V Military Hospital, Morocco.
Resident of Cardiology, assigned to intensive care unit, Morocco
Resident of Cardiology, assigned to non-invasive exploration department, Morocco
Head of the Intensive Care Unit, Morocco
Head of Non-Invasive Exploration Department, Morocco
Head of the Cardiology department of the Mohammed V Military Hospital, Morocco
Received Date: 30/03/2021; Published Date: 09/04/2021
*Corresponding author: Nuance Divine Tchiloemba Tchibinda, Resident of cardiology, assigned to intensive care unit, tnuance@yahoo.fr, 00212602260473, Morocco
Soumia Faid, Resident of cardiology, assigned to non -invasive exploration department, soumiafaid800@gmail.com, 00212665868434, Morocco
Summary
Intracardiac thrombi constitute an exceptional complication during Behçet's disease. It can be isolated or associated with pulmonary artery disease. To our knowledge, less than 50 cases have been reported in the literature.
We report the observation of a 21-year-old patient known to be carrying behcet's disease for one year diagnosed after presenting hemoptysis and bipolar aphthosis; Cardiovascular exploration revealed an intracardiac mass requiring surgical thrombectomy, the anatomopathological study of the operative specimen had revealed a constituted fibrino-cruoric thrombus. The patient had been put on corticosteroids, colchicine and antivitamin K, the evolution was marked 10 months after his first surgery by the recurrence of the intra-right Ventricle (RV) thrombus complicated by pulmonary embolism.
Keywords: Behçet's disease, intracardiac thrombosis, pulmonary embolism, complications.
Introduction
Behçet's Disease (BD) is a chronic systemic vasculitis of unknown etiology occurring mainly in young men between 20 and 40 years old. Its diagnosis is clinical and is based on international criteria, [1,2] characterized by the frequency and benignity of cutaneous, mucous and articular manifestations and the severity of ocular, central neurological, vascular and especially arterial and digestive manifestations [1].
It is a disease that progresses in spurts, sometimes spontaneously regressive, and the treatment of which is mainly symptomatic [1].
The frequency of cardiac involvement varies from less than 1 to 6% in clinical series and 16.5% in autopsy series [3]. All three cardiac tunics can be affected, with pericarditis, myocardial, valve, coronary and conduction tissue damage. Intracardiac thrombosis is very rare, predominantly in the right chambers of the heart [3] and complicated by Pulmonary Embolism (PE) which is one of the most severe complications of BD, and which could constitute a life-threatening emergency.
Case Report
We report the clinical observation of Mr OS, a 21-year-old patient, without cardiovascular risk factors, who has been followed for a year for behcet's disease which was complicated by a mass in the large-sized RV flushing chamber which was proliferating into the pulmonary artery evoking a thrombosis that has not changed in size under heparin therapy thus posing the indication for surgical thrombectomy with an optimal echocardiographic control showing the disappearance of the RV mass immediately in post-surgery and 2 months after surgery. The evolution was marked one month before his admission this time, with a worsening of his basic dyspnea going from stage II to stage III of NYHA associated with hemoptysis of average abundance with the notion of good therapeutic adherence to corticosteroids, colchicine and to AVKs but without INR control. On examination, the patient was hemodynamically stable, no signs of right heart failure; no mucocutaneous lesions, the biological assessment found an INR at 1.30, a troponin at 6 (normal), the rest of the biological assessment was no abnormalitie; transthoracic echocardiography revealed an intraVD thombus measuring 52X25mm mooring the anterior leaflet of the tricuspid valve, the RV was not dilated ,of borderline systolic function, the pulmonary artery was of normal size without visible thrombus, the thoracic CT angiography showed a proximal pulmonary embolism of the middle and inferior branch of the right pulmonary artery without arterial aneurysms. The patient was put on heparin of low molecular weight, Anti-Platelet Agent (APA) associated with antivitamin K, since the thrombus recurrence, a reinforcement of drug treatment was required combining immunosuppressors: azathioprine 150 mg / day, colchicine and oral corticosteroid therapy at the dose of 1 mg / kg per day.
The evolution was favorable with no recurrent hemoptysis. The echocardiographic Follow-up after one month of treatment showed marked regression of the right intraventricular thrombus. Currently, the patient is still followed regularly with a follow-up of 6 months until complete dissolution of the thrombus (Figures 1-5).
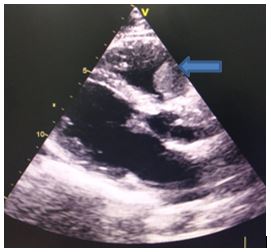
Figure 1: Large axis parasternal section: showing a thrombus in the right ventricle
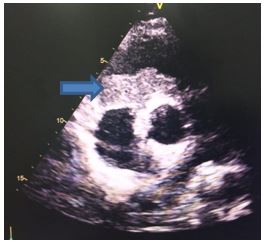
Figure 2: Small axis parasternal section

Figure 3: Apical cut 4 cavities
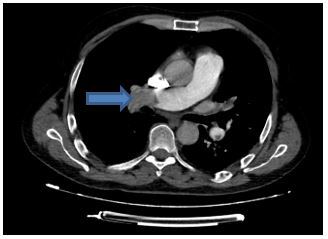
Figure 4: Pulmonary CT angiography: right proximal pulmonary embolism
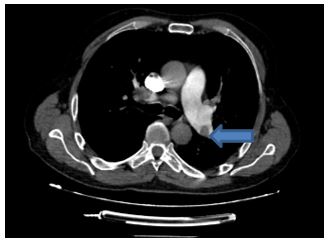
Figure 5: Pulmonary CT angiography: left distal pulmonary embolism
Discussion
Intracardiac thrombi are a very rare manifestation of Behçet's disease. This manifestation occurs with predilection in young males and rarely reveals BD. It can be isolated, but must necessarily be investigated for other vascular damage, including Pulmonary Artery Aneurysms (PAA) [4]. It usually occurs as part of an already advanced Behçet's disease and it is rarely inaugural. The right ventricle is the preferential site which can be complicated by pulmonary embolism, as is the case of our patient. Prolonged fever or an inflammatory syndrome or even chest pain, hemoptysis or dyspnea corresponding to pulmonary embolism should alert the clinician [5].
The mechanism of occurrence is not clear and would probably be secondary to ischemia’s and endothelial lesions promoting platelet aggregation, or the presence of antibodies directed against an enolase, a target protein on the surface of endothelial cells. [6] Antiphospholipid antibodies found in 18% or the presence of other prothrombotic plasma factors such as protein C and or S deficiency [7], increase in factor VIII, homozygosity for Leyden factor V or mutation of the prothrombin gene [7,8].
Moderate hyperhomocysteinemia has been reported a risk factor for venous or arterial thrombosis in the general population and is associated with deficiencies of vitamins B9, B6, B12. Several publications mentioned higher plasma homocysteine values in patients with active BD compared to control groups, with a significant correlation between hyperhomocysteinemia and possible vascular and ophthalmic damage [9, 10].
The diagnosis is based on imaging, firstly with cardiac ultrasound showing an intracardiac mass more echogenic than blood, heterogeneous and adherent to the wall. The differential diagnosis can arise with primary tumors of the right heart, especially with myxomas. Chest CT angiography, or even cardiac MRI, can also help in the diagnosis. Iridium cardiac scintigraphy can determine the acute or chronic nature of the thrombus. The resolution of the thrombus under anticoagulants constitutes a retrospective diagnostic argument [11]. In fact, in our patient, the regression of the intraventricular thrombus under treatment was an element supporting our diagnosis retrospectively.
Arterial involvement is much rarer; Pulmonary artery aneurysms are most often diagnosed if presenting repeated hemoptysis. Chest radiography is rarely normal and shows rounded parahilar opacities, usually bilateral, sometimes distal [12]. Pulmonary angiography and better yet, CT angiography of the chest can be used to visualize them. The PET-scan can also be indicated in these forms [13], but it remains very expensive. These aneurysms have a very poor prognosis with a mortality of 50% the first year. They can be complicated by rupture leading to death by massive hemoptysis and also aneurysmal thrombosis exposing the patient to a significant risk of pulmonary embolism. In our patient, CT angiography did not demonstrate PAA; pulmonary embolism and right ventricular thrombus did not result in right heart failure, as has been reported in other observations.
Medical treatment is conventionally based on immunosuppressive agents, corticosteroids, colchicine and anticoagulants which have been shown to be effective in several cases with resolution of the thrombus. [14] If medical treatment is ineffective or there is a massive or extensive thrombus, a surgical thrombectomy can be proposed as the case of our patient during his first episode of unresolved intracardiac thrombosis even under medical treatment. Recurrences after surgical treatment are possible and require reinforcement of drug treatment. In certain cases, thrombolysis can constitute an interesting alternative to surgical treatment [15]. In our patient, adding immunosuppressors to the rest of the treatment allowed a complete resolution of the thrombus with good outcome.
Conclusion
Intracardiac thrombosis is a rare complication of Behçet's disease that can simulate an intracardiac tumor. Arterial involvement in this disease is rare with higher mortality. The prognosis is unpredictable due to the onset of severe hemoptysis. In our patient, pulmonary embolism and right ventricular thrombus did not result in right heart failure, with good response and evolution after the strengthening of medical treatment.
References
- International Study Group for Behçet’s disease. Criteria for diagnosis of Behçet’s disease. Lancet. 1990; 335(8697): 1078-1080.
- B’chir Hamzaoui S, Harmel A, Bouslama K, Abdallah M, Ennafaa M, M’rad S, et al. Behçet’s disease in Tunisia. Clinical study of 519 cases. Rev Med Interne. 2006; 27(10): 742-750.
- Darie C, Knezinsky M, Demolombe-Rague S, Pinède L, Périnetti M, Ninet JF, et al. Pseudotumeur cardiaque révélant une maladie de Behçet. Rev Med Interne. 2005; 26(5): 420-424.
- Elqatni M, Sekkach Y, Abouzahir A, Ghafir D. Right atrium thrombus and pulmonary artery aneurysm in a man with Behc¸et’s Disease. Intern Med 2011; 50: 263-264.
- Hammani S, Addad F, Kaoubaa N, Golli M, Chebbi W, Hamzaoui A, et al. Pulmonary embolism and Behc¸et’s disease. Arch Mal Coeur Vaiss 2006; 99: 786-790.
- Hamza M. Physiopathologie de la maladie de Behçet. Sem Hop Paris. 1987; 63: 1195-200.
- Leiba M, Seligsohn U, Sidi Y, Harats D, Sela BA, Griffin GH, et al. Thrombophilic factors are not the leading cause of thrombosis in Behc¸et’s disease. Ann Rheum Dis 2004; 63: 1445-1449.
- Silingardi M, Salvarani C, Boiardi L, Accardo P, Iorio A, Olivieri I, et al. Leiden and prothrombin gene G20210A mutations in Italian patients with Behc¸et’s disease and deep vein thrombosis. Arthritis Rheum 2004; 51: 177-183.
- Lee KH, Chung HS, Kim HS, Oh SH, Ma MK, Baik JH, et al. Human alpha- enolase from endothelial cells as a target antigen of anti-endothelial cell antibody in Behçet’s disease. Arthritis Rheum. 2003; 48(7): 2025-2035.
- Borson-Chazot F, Guadagnino L, Bernard S, Moulin P. Hyperhomocystéinémie et risque vasculaire. Act Med Int. 1999; 3: 31-34.
- Marc K, Iraqui G, Jniene A, Benamor J, Bourkadi JE. Thrombose intracardiaque et anévrismes de l’artère pulmonaire au cours de la maladie de Behc¸et. Rev Mal Respir 2008; 25: 69-72.
- Tazi-Mezalek, Ammouri W, Maamar M. Les atteintes vasculaires au cours de la maladie de Behc¸et. Rev Méd Interne 2009; 30: 232-237.
- Wenger M, Baltaci M, Klein-Weigel P, Donnemiller E, Moncayo R, Schirmer M. 18F-FDG-positron emission tomography for diagnosis of large vessel arteritis in Behc¸et’s disease. Adv Exp Med Biol 2003; 528: 435-436.
- Zaghba N, Ech-cherrate A, Benjelloun H, Yassine N, Bakhatar A, Bahlaoui A. Cardiac thrombosis, pulmonary artery aneurism and pulmonary embolism revealed Behçet’s disease. Revue de Pneumologie Clinique, 2012; 68: 307-310.
- Dincer I, Dandachi R, AtmacaY, Erol C, Caglar N, Oral D. A recurrent right heart thrombus in a patient with Behcet’s disease. Echocardiography. 2001; 18(1): 15- 18.

