Effectiveness Of Low-Dose Corticosteroids In The Treatment Of Marshall Syndrome – Case Report
Veronica Epure*
ENT Department, M. S. Curie Clinical Emergency Hospital Bucharest, Romania
Carol Davila University of Medicine and Pharmacy Bucharest, Romania
Received Date: 25/03/2021; Published Date: 06/04/2021
*Corresponding author: Veronica Epure, ENT Department, M. S. Curie Clinical Emergency Hospital Bucharest,Romania, Carol Davila University of Medicine and Pharmacy Bucharest, Romania, Email: veronica_epure@yahoo.co.uk, 0040722203964, Str. Pajiştei nr. 32 et. 3 ap. 15 sector 4 Bucharest, Romania
Abstract
Defined by recurrent febrile episodes af angina, adenitis and stomatitis, Marshall syndrome is frequently encountered in clinical practice in children. The diagnosis is clinical, aided by the dramatic resolution of the symptoms after administration of oral cortisone. The authors report a case of Marshall syndrome and discuss the effectiveness of low-dose weight-independent oral corticosteroids administered in this case, based on clinical datas from literature.
Keywords: Marshall syndrome; Angina; Adenitis; Oral corticosteroids
Introduction
Attacks of periodic fever, aphtous stomatitis, pharyngitis and adenitis define a childhood syndrome of unknown cause which was first described by Marshall in 1987 (PFAPA) [1]. The episodes of fever and sore throat usually start in early childhood (typically under the age of 5) and recur regularly every 2 to 12 weeks [2,3].
The treatment of PFAPA syndrome is still a matter of debate. Antibiotics and NSAIDʼs are ineffective. The use of oral corticosteroids causes dramatic resolution of symptoms and aids in the diagnosis as well [2,3]. On the long term, tonsillectomy seems to be a good option to stop the recurrence of the symptoms.
Initially, the recommended doses of steroides used in the treatment of PFAPA were quite high [4]; due to their significant side effects [5], nowadays specialists tend to decrease these doses.
We report a case of a child with Marshall syndrome in whom low doses of oral dexametasone were effective in treating the symptoms.
Case Report
The attacks of high fever, angina, stomatitis and cervical adenitis started at the age of 8 in our patient (T.O.); between december 2018 and may 2019 the episodes recurred every 4 weeks; he always presented with high fever (over 390 C), resistant to oral antibiotics and NSAIDs. On examination his tonsills were always covered with purrulent deposits, hypertrophic and during half of the attacks he also had aphtous stomatitis.
He always had dramatic resolution of symptoms on administration of oral corticosteroids; lab tests also showed dramatic subside of inflammatory markers in a few hours after corticotherapy (Table 1). In between episodes all lab tests had normal values. During this interval, the patient (weighing approx. 24kg at the age of 8) had 6 fever attacks, we always administered 2 doses of oral Dexamethasone (4mg each), 12 hours apart; the resolution of fever and angina occured every single time, sometimes even after the first dose of oral dexamethasone. During some of the attacks oral antibiotics were also associated (Cefuroxime suspension).
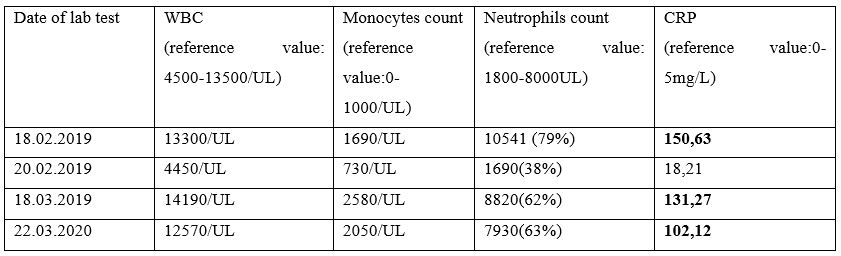
Table 1: Variation of blood cell count and CRP before (18.02) and after (20.02) administration of oral dexamethasone
Between may 2019 and march 2020 the patient was asymptomatic; the fever attacks recur in march 2020, by the age of 10, accompanied by angina, stomatitis and marked inflammation on lab tests (table 1). We administered 2 doses of oral dexamethasone (8mg each), at 12 hours interval, with perfect resolution of the symptoms for the first two fever attacks. Our patient ʼs weight was by that time 54 kg. After 2 attacks, we decided and performed adenotonsillectomy in this patient; no fever episode recurred after surgery for 9 months.
Discussion
Initially, the recommended doses of corticosteriods for treatment of PFAPA were quite high and weight-dependent: prednisone 2mg/kg per dose (one or two doses recommended); most of the practicians use today the equivalent of prednisone orally 1mg/kg/day, single dose or 2 doses, or dexamethasone orally or iv, 0,5mg/kg/day, one or 2 doses.
Reviewing the literature, there are only few authors reporting lower doses of betamethasone to be effective in aborting fever episodes in PFAPA: 0,5mg single-dose betamethasone for children under 5 and 1mg for children over 6 years old [6]. The conventional dose of betamethasone was thought to be 0,1-0,2mg/kg [7]. Other authors reported effectiveness of low doses of prednisone 0,5mg/kg/day (conventional dose 1-2mg/kg/day) [8,9] in treating the fever attacks.
Although the conventional dose for dexamethasone used to abort fever episodes in PFAPA is 0,5mg/kg/day, administered orally or intravenously, we succeded in treating the 8 fever attacks in our patient with low-dose, weight independent dexametasone: 4mg per day (at first, when the patient was under 40kg of weight) (0,15mg/kg), then 8mg per day (when the patient was over 40kg); we administered 2 doses, 12 hours apart (0,15mg/kg).
In a series of 11 patients with PFAPA diagnosed and treated in our department, we used the same low doses of oral dexamethasone, weigh-independent and the result was always good, sometimes even after the first dose was administered.
Although our case seems to by a typical Marshall syndrome case, we notice its late onset (at the age of 8 rather then under 5 years) and the long asymptomatic period in this patient.
Conclusion
Administration of corticosteroids in PFAPA syndrome dramatically improves the symptoms, but bearing in mind the threatening side-effects of steroids, we advise in favour of lowering the dose as much as possible.
References
- Marshall GS, Edwards KM, Butler J, Lawton AR. Syndrome of periodic fever, pharyngitis and aphtous stomatitis, J Pediatr 1987; 110: 43-46.
- Berlucchi M., Meini A, Plebani A, Bonvini MG, Lombardi D, Nicolai P. Update on treatment of Marshall’s syndrome (PFAPA syndrome): report of five cases with review of the literature; Ann Otol Rhinol Laryngol 2003; 112(4): 365-369.
- Feder HM Jr. Periodic fever, aphtous stomatitis, pharyngitis, adenitis: a clinical review of a new syndrome, Curr Opin Pediatr 2000; 12: 253-256.
- Padeh S, Brezniak N, Zemer D, Pras E, Livneh A, Langevitz P, Migdal A, Pras M, Passwell JH. Periodic fever, aphtous stomatitis, pharyngitis and adenopathy syndrome: clinical characteristics and outcome, J Pediatr 1999; 135(1): 98-101.
- Scimeca PG, James-Herry AG, Weinblatt ME. Atypical PFAPA syndrome in a young girl with Fanconi anemia, J Pediatr Hematol Oncol. 1996;18(2): 159-161.
- Nadim NH, Nasir N, Habib MG, Samra NG. The lowest dose of corticosteroids, which stops the episodes of PFAPA syndrome, Australasian Medical Journal May 2017; 10(4): 322-328.
- Esposito S, Bianchini S, Fattizzio M, Baggi E, Marchisio P, Rigante D. The Enigma of Periodic Fever, Aphtous Dtomatitis, Pharyngitis and Adenitis Syndrome, Pediatr Infect Dis J. 2014; 650-652.
- Tasher D, Somekh E, Dalal I. PFAPA syndrome: new clinical aspects disclosed. Arch Dis Child. 2006; 91(12): 981-984.
- Yazgen H, Gultekin E, Yazicilar O, Sagun OF, Uzun L. Comparison of conventional and low dose of steroid in the treatment of PFAPA syndrome: preliminary study. Int J Pediatr Otorhinolaryngol. 2012; 76(11): 1588-1590.

