Open fracture with massive ulna loss. Case presentation
Luis Crescencio Bretón Espinosa, Claribel Plain Pazos, Lázaro Martin Martínez Estupiñan, Sergio Virgilio Morales Piñeiro, Roberto Mata Cuevas and Leonardo Domínguez Plain
I Degree Specialist in Orthopedics and Traumatology, Provincial General University Hospital “Mártires del 9 de Abril”, Cuba
Specialist of I and II Degree in Comprehensive General Medicine, Faculty of Medical Sciences of Sagua la Grande,Cuba
II Degree Specialist in Orthopedics and Traumatology, Provincial General University Hospital “Mártires del 9 de Abril”, Cuba
I and II Degree Specialist in Orthopedics and Traumatology, Provincial General University Hospital “Mártires del 9 de Abril”, Cuba
Resident of 3rd year of Orthopedics and Traumatology, Provincial General University Hospital “Mártires del 9 de Abril”, Cuba
Received Date: 18/03/2021; Published Date: 31/03/2021
*Corresponding author: Claribel Plain Pazos, Specialist of I and II Degree in Comprehensive General Medicine, Faculty of Medical Sciences of Sagua la Grande, Cuba. Email: claribelpp@infomed.sld.cu
Abstract
Introduction: Post-traumatic segmental bone defects in long bones can be secondary to exposed fractures; their management is a challenge for the professionals who attend to them.
Presentation of the patient: We present a patient with an open fracture of the right ulna with massive loss of bone, product of an AK rifle shot treated in three stages at the Main Military Hospital of Luanda, People's Republic of Angola, in the intermediate stage with the linear monopolar external fixator. General Distractor-Compressor (DCG) of Professor Dr. Sc. Rodrigo Álvarez Cambras. Young patient. The procedure imposed was the fibula graft, placed using the Henry approach, with an evolution and follow-up of 22 weeks. The result was good from a clinical, radiological and functional point of view. Function of the forearm, elbow and wrist was achieved.
Keywords: Exposed fracture; Ulna; Fibula; External fixation
Introduction
The external fixators in modern orthopedic and trauma surgery constitute, together with the internal compression system and endoprostheses, fundamental pillars of the surgical treatments of the specialty [1].
Their indications are specific, they are used mainly in open injuries. Open fractures can result from a variety of injuries. Common direct mechanisms include high-energy trauma (the most common) such as traffic accidents, firearm injuries, and falls from a height. They occur more frequently in men than in women, with a mean age of 40 and 56 years, respectively [2].
Among the most feared complications is pseudoarthrosis [3,4]. Post-traumatic segmental bone defects in long bones can be secondary to infection of exposed fractures. Associated with absolute bone loss at the level of the fracture site, relative bone deficits may appear that extend several centimeters proximally and distally; and rebuilding it is a challenge [5].
The most important principle for obtaining consolidation in all fractures, including non-unions, is the stability of the bone fragments [4], supported by good biological induction, with the autologous cancellous graft being the most frequently used biological stimulator [6].
A cancellous bone graft has three functions: to provide osteo induction, which induces bone production locally by recruiting bone-forming cells; promote osteo conduction, providing support for bone deposition, and lastly, constitute the source of bone cell formation. Bone graft incorporation is a sequential process that begins with inflammation and goes through different stages of revascularization and osteogenesis until a mechanically valid structure is achieved [6].
The purpose of this work is to present a patient, with a serious injury, the behaviors before this type of affection, his post-surgical evolution and final result, highlighting the benefits of external fixation and the application of the autologous peroneal graft.
Case Presentation
Information of the patiente: 21-year-old patient, an infantryman of the Angolan armed forces, who suffered an open fracture of the right ulna with massive loss of bone, as a result of an AK rifle shot.
Clinical findings:
Diagnostic evaluation: A clinical diagnosis of rupture of the long head of the biceps was made, corroborated by ultrasound of the area, and a provisional posterior brachial splint was placed.
Complementary pre-operative:
- Hematocrit: 0.41 L / L
- Hemoglobin: 12.3 g /%
- Bleeding time: 1.5 min
- Clotting time: 9 min
- Platelet count: 240x109 / L
The admission for study and surgical treatment is decided, informed consent is signed by the patient and family, where they leave their approval of the intervention. A pre-operative consultation is carried out and three days later it is taken to the operating room.
Therapeutic intervention. Initially, the wound was debrided and healing was achieved without local infection. He was re-operated 5 weeks later, applying a massive free fibula graft according to the bone defect and secured with an intramedullary wire, finally the general distracting-compressor monopolar linear external fixator (DCG) of Professor Dr. Sc. Rodrigo Álvarez was applied. Cambras. at the remaining ends of the ulna.
Monitoring and results. System compression at the end of the surgical intervention and periodically for 1 month.
After 3 months, complete clinical and radiological consolidation was achieved, removing the fixator with recovered function of the forearm at 5 months.
The patient was fully reintegrated to his previous social and work environment.
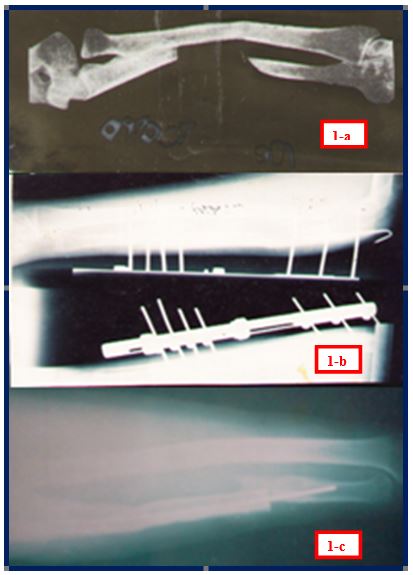
Figure 1: a- Radiological image of the lesion, after the initial debridement. b- Radiological image of the lesion with the fibula graft, intramedullary wire and RALCA external fixator. c- Radiological image of consolidation but without removing the wire.
Discussion
The development of industry, motorized transport and armed conflicts have led to an increase in the incidence of injuries that affect young people and people of working age.
Severe upper limb injuries with tissue loss produce significant disability. Their treatment aims to provide stability and restore an adequate biological environment, to allow the growth and incorporation of bone tissue, and to restore the continuity of the affected bone.
Orthopedic trauma surgery requires the regular use of bone grafts to contribute to the timely healing of musculoskeletal injuries. Autologous iliac crest graft continues to be the gold standard, although the morbidity associated with obtaining the bone graft has prompted professionals to seek methods to increase healing with bone graft substitutes (a term that describes various products that exert different effects). on bone healing) [7].
Another valid alternative would be the Masque let technique or induced membrane technique, a surgical procedure used to treat pseudoarthrosis, diffuse osteomyelitis with large sequestration and bone defects, it represents a good alternative in the management of segmental bone defects, with adequate rates of consolidation, low complications, tolerable by the patient and reproducible in hospitals in our environment [8,9].
Vascularized bone grafts are also a valid alternative for the treatment of large bone defects [8,10].
Cancellous bone is revascularized faster than cortical bone, since its more porous structure favors the penetration of vessels that gradually grow into the medullary spaces, leading to complete revascularization in a period of time between 2 and 3 weeks [4]. External fixation requires little surgery time and produces very little blood loss. It is applied remotely from the injury site and therefore does not interfere with wound management [1].
In our case, a free fibula graft was used, which has the advantage of being similar in structure to the ulna, due to its tubular shape and is sufficiently long for the reconstruction of large defects of the upper limb. Extra-focal external fixation provides advantages, such as the guarantee of stability at the fracture site, uniform compression at the site of the injury, and facilitates early and immediate mobilization of the affected limb, as well as neutralization of local forces and ease of care, of the soft tissues, the fixation medium used in the case was the RALCA external fixator. In addition, anticipating a possible displacement of the fibula graft, taking into account that there was never local infection in the forearm, the short time of evolution and the good physical condition of the young man, it was decided to use the intramedullary wire.
In the case presented, bone consolidation occurred within an adequate period, however it was decided as a group to leave the fixator in place until 20 weeks, to avoid the possibility of a fatigue fracture at the level of the injury.
A wide variety of complications secondary to the open fracture can occur, such as compartment syndrome, nonunion, loss of function, neurovascular injury, infection, osteomyelitis and amputation.2 In our patient we did not face any complications, or deformities, the possibility of We believe that fatigue fractures can be minimized by prolonging the use of the external fixator until the bone corticalizes.
The application of this technique (autologous fibula graft in forearm bone defects of any etiology with their respective osteosynthesis) is considered a good therapeutic option, since the results in most cases are good [1]. We consider the technique Cuban External Fixator by Professor Álvarez Cambras, very effective for traumatic forearm injuries and excellent for exposed fractures caused by firearms.
Conflicts of Interest
The authors have no conflict of interest regarding the information or procedures used in this article.
References
- Ferrer Lozano Y, Morejón Trofimova Y, Oquendo Vázquez P. Use of RALCA® external fixator in open fractures. 14-year experience. Medisur [Internet]. 2021; 15(5): 647-655.
- Brenes Menéndez M. Manejo de fracturas abiertas. Rev Med Sinergia 2020; 5(4): e440
- Bornot Duránd Y, Ferrer Matos G, Font Ávila ME, Ferrer Matos M. Pseudoartrosis no viable de tercio distal del cúbito. Correo Científico Médico de Holguín [Internet]. 2017; 21(4): 1240-1245.
- Velázquez Moreno JD, Casiano Guerrero G. Algoritmo del tratamiento de la seudoartrosis diafisaria. Acta ortopédica mexicana [Internet]. 2019; 33(1): 50-57.
- Gentile L, Iglesias Santiago L, Lobos Centeno E, Vanoli F, Allende Nores CA. Defectos óseos diafisarios postraumáticos en la extremidad superior de niños. Rev. Asoc. Argent. Ortop. Traumatol. [Internet]. 2017; 82(4): 277-293.
- Léniz P, Forriol F. Estudio de la incorporación de tres tipos de hueso esponjoso (autoinjerto, aloinjerto congelado y liofilizado). Modelo experimental en corderos. Rev. Esp. de Cirugia Ortopédica y Traumatología [Internet]. 2016; 60: 286-95.
- De Long WG, Einhorn TA, Koval K, McKee M, Smith W, Roy Sanders R, et al. Injertos óseos y sustitutos de injerto óseo en la cirugía traumatológica ortopédica. Análisis crítico. JBJS. [Internet]. 2017; 7(3): 649-664.
- Lara-Villca R, Undurraga-Carmona N. Técnica de membrana inducida en la reconstrucción de defectos óseos postraumáticos. Gac Med Bol. [Internet]. 2018; 41(2): 18-20.
- Micev AJ, Kalainov DM, Soneru AP. Masquelet technique for treatment of segmental bone loss in the upper extremity. J Hand Surg Am [Internet]. 2018; 40(3): 593-598.
- Zaidenberg EE, Martínez E, Pastrana M, Juarez Cesca F, Olazarri F, Zaidenberg CR. Injerto óseo vascularizado pediculado del radio distal para tratar la seudoartrosis recalcitrante del cúbito. [Vascularized bone graft of the distal radius for recalcitrant ulnar pseudoarthrosis.]. Rev. Asoc. Arg. Ort. y Traumatol [Internet]. 2018; 83(1):31-37.

