Appendicular Perforation in Covid-19 Reinfection-A First Case Report
Jayakrishna Reddy Aluru*
Department of Medicine, Lifeline institute, India.
Received Date: 10/03/2021; Published Date: 22/03/2021
*Corresponding author: Joana Trigo Medeiros, Internal Medicine Department, Braga Hospital, Portugal. Sete Fontes,S. Victor, Braga, PT 4710-243. Email: jrtmedeiros@gmail.com, +351 253 027 000.
Abstract
Introduction: In the current pandemic, a cause for concern in COVID patients is reinfection after a complete recovery. This is the case report of a patient who presented with acute abdomen and with COVID infection, who initially settled with conservative management of acute appendicitis, but presented again some weeks later with a perforated appendix and COVID reinfection.
Case Presentation: A 56-year-old male presented to a rural hospital with clinical features of acute appendicitis, proved by ultrasonography of the abdomen that showed an inflamed appendix, and Reverse Transcription-Polymerase Chain Reaction screening (RT-PCR) was positive for COVID-19. In view of the pandemic, he was managed conservatively and his condition improved. He was isolated and RT-PCR was negative for COVID at discharge. He then presented after 3 months with severe right lower quadrant pain and fever, and CECT abdomen showed appendicular perforation with abscess and a large peri appendicular mass. On screening, HRCT chest showed bilateral ground glass opacities consistent with COVID pneumonia. A repeat RT- PCR was done and the patient was started on Meropenem, with some symptomatic improvement. The repeat PCR was positive, confirming a COVID reinfection.
Discussion: The concept of COVID reinfection is relatively new, with some patients not developing sufficient antibodies to stave off another viral assault. In a proportion of cases, the reinfection occurs by another strain of the virus. Needless to say, in pandemic times, patients with acute abdomen undergoing a CECT, should also have a simultaneous HRCT of the chest to screen for COVID pneumonia ground glass opacities, as these are pathognomonic of COVID infection. The two unusual features of this case are, documented reinfection with the COVID-19 virus, and perforation of the appendix with an appendicular abscess. A multi-disciplinary discussion helped to do damage control minimally invasive surgery, followed by definitive treatment after four weeks.
Conclusion: A case of COVID-19 reinfection, with exacerbation of appendicitis, and appendicular perforation, is presented here, managed by laparoscopic peritoneal lavage and drainage, with laparoscopic adhesiolysis and appendicectomy after the reinfection cleared.
A search of available English medical literature revealed no previous similar case report.
Introduction
In Wuhan, China, December 2019 the first reports of what would later be known as COVID-19 (Coronavirus Disease 2019), a disease caused SARS-CoV-2 (an RNA virus) were described. This spread at an alarming rate, leading the World Health Organization to declare a pandemic in March 2020. This has distinct clinical presentations, from critical cases to asymptomatic cases, with high lethality. However, patients with non-traumatic surgical emergencies, such as acute cholecystitis and appendicitis, continue to be treated at the emergency services [1].
In the current pandemic, a cause for concern in COVID patients is reinfection after a complete recovery. This is the case report of a patient who presented with acute abdomen and with COVID infection, who settled with conservative management of acute appendicitis, but presented again some weeks later with a perforated appendix. He was found to be RT -PCR positive once more. He was managed with drainage of the abscess, and underwent an uneventful appendicectomy laparoscopically after six weeks. The complex aspects of a perforated viscus in the presence of reinfection with COVID 19, are discussed; this article is being published for its diversity during this pandemic.
Case Details
A 56-year-old male presented to the surgery OPD of a rural hospital with clinical features of acute appendicitis, proved by ultrasonography of the abdomen that showed an inflamed appendix, and screening RT-PCR was positive for COVID-19 with no clinical symptoms. As patient and surgeons were both disinclined to proceed with surgery, he was managed by intravenous antibiotics and bed rest, the modified Oschner-Sherren regime was followed, and in one week he improved symptomatically, with resolution of pain, fever and leucocytosis.
Subsequently, he was isolated, and his repeat RT-PCR was negative.
He was discharged and advised to have an appendicectomy at the earliest, but he chose to defer the procedure.
Three months later he developed severe abdominal pain, and fever, with a tender and red swelling over the right lower quadrant of the abdomen for two days prior to presentation. After admission and antibiotics, he underwent a CECT scan of the abdomen, along with a HRCT chest screening.
This showed an appendicular perforation with an abscess, and a large appendicular mass. The chest showed bilateral ground glass opacities consistent with COVID-19 pneumonia with a severity score 15/25. (Figure 1) A repeat RT- PCR was done and the patient was started on Meropenem, with some symptomatic improvement. The repeat PCR was positive, confirming a COVID-19 reinfection.
Blood work showed a marked leucocytosis, and mild lymphopenia. His serum antibody level was only mildly elevated.
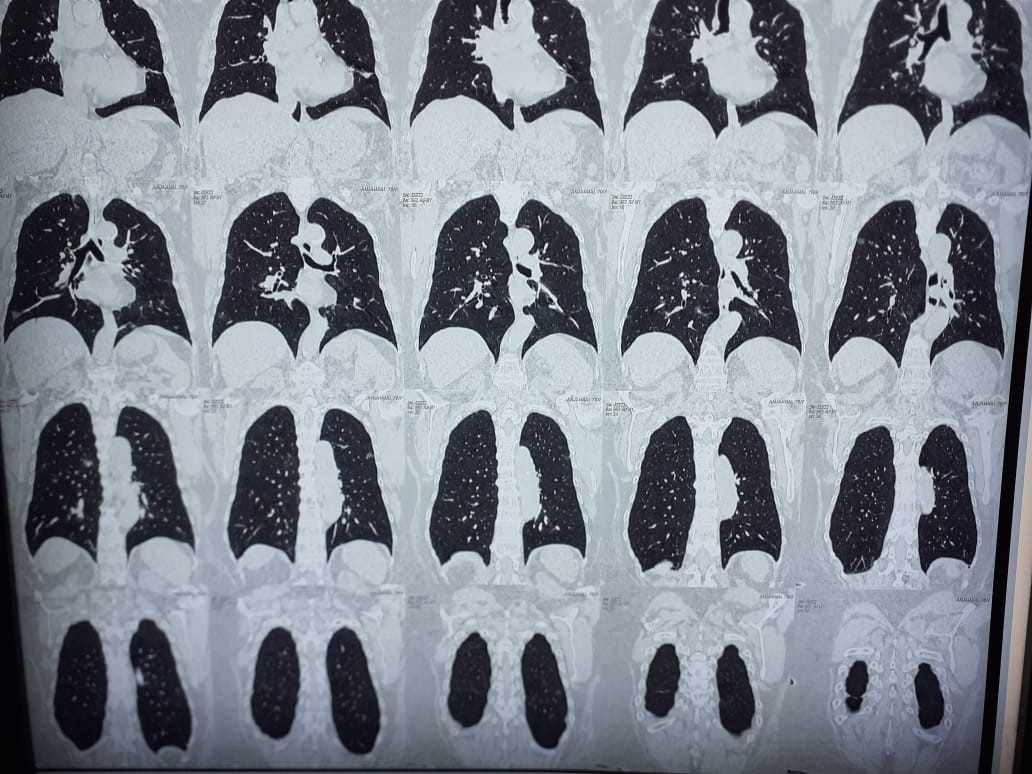
Figure-1: HRCT chest showing Ground glass opacities.

Figure-2: Purulent collection in Right ilical fossa.

Figure-3: Dissecting the adherent bowel.

Figure-4: Drain tube.
Operative Procedure
With thorough available knowledge of the pre, peri and post-operative protocols. Patient was proceeded with spinal anaesthesia, after obtaining a high-risk consent, a diagnostic laparoscopy, and thorough peritoneal lavage, of the purulent material in the right iliac fossa and pelvis was done. (Figure 2) As there was no localised collection that could be drained ultrasonographical, this option was chosen.
The abscess was drained out after releasing the adherent bowel and sigmoid colon, (Figure 3) and the area was not dissected further, owing to the dangers of using energy sources, that could potentially aerosolise the COVID virus. The right iliac fossa and pelvis were drained (Figure 4), and the procedure was completed.
The postoperative period was relatively uneventful, and the patient was once more started on Inj Remdesevir and Meropenem. By the fifth postoperative day, the patient was RT-PCR negative once more.
The antibody test was done, and this time it was significantly elevated.
The patient was discharged with the drainage tubes in situ, and removed after sonographic screening was negative on the tenth postoperative day.
One month later, after a repeat RT-PCR was negative, he was readmitted for an elective laparoscopy and underwent adhesiolysis and appendicectomy, and was discharged on the second postoperative day. Histopathology showing RT-PCR not positive in the appendicular specimen.
Discussion
According to Torres et al, about 12 months after the first cases of COVID‐19, there is still no consensus in literature of reinfection by SARS‐CoV‐2 [2]. However, there have been some reports of such cases around the world. The strongest evidence of reinfection requires documentation of an infection by a molecularly distinct form of the same virus after the elimination of the previous infection.
COVID reinfection was confirmed for the first time in Hong Kong, in August 2020, through genetic sequencing of two samples collected by nasal swab from the same patient with a time difference of 142 days. There was evidence that these viral genomes originated from different lineages, one of which is close to our modern strains, while the other closely resembles strains isolated in March and April 2020 [2].
The concept of COVID-19 reinfection is relatively new, with some patients not developing sufficient antibodies to stave off another viral assault. In a proportion of cases, the reinfection occurs by another strain of the virus. However, with aerosol-generating procedures like surgery, endoscopy, and anaesthesia carrying a higher risk of transmission and hence requiring robust measures to protect the patients and the staff, few articles have stated practical strategy to manage operative protocols during the COVID-19 pandemic [3-5].
Zheng at al has described in detail perioperative management of patients with suspected or confirmed COVID-19 [6].
These guidelines have been successfully implemented in our institute and were strictly adhered to in this particular case as well.
The acute abdomen in patients with COVID-19 has been well described. There have been a few case reports of patients with right iliac fossa pain and tenderness, known as pseudo appendicitis, who turned out to be COVID-19 positive. The acute abdomen is often due to mesenteric lymphadenitis or acute pancreatitis in patients with COVID-19. Several longitudinal studies warn of the dangers of rushing into surgery in patients presenting with exacerbation of gastro-intestinal symptoms whilst suffering from COVID-19.
Patients with COVID-19 acute abdomen are of two types. The first group of patients have an acute abdomen, and are incidentally found to be COVID positive, like the patient in this case report. The second group, which has a far worse prognosis, comprises patients who have COVID-19 disease, and progress to the development of acute surgical abdomen. Perforation of the viscus has been described in these patients, and the prognosis is dark [7].
One single case report suggested that the SARS Cov 2 infection could be the cause of the acute appendicitis, both by the highly atypical features on histology, as well as the PCR being positive in the excised appendix.
Needless to say, in pandemic times, patients with acute abdomen undergoing a CECT should also have a simultaneous HRCT of the chest to pick up the COVID-19 pneumonia ground glass opacities, as these are pathognomonic of COVID-19 infection.
A conservative management of acute appendicitis has been described in a COVID-19 patient,[8][9] and several successful laparoscopic and open surgeries for acute abdomen have been described.[10][11] An atypical presentation of appendicitis has also been reported as the presenting feature of COVID-19 infection, with the fever found to be suppressed in patients. Many of these patients are also exposed to therapeutic corticosteroids to suppress the inflammatory process, and this further confounds the clinical presentation.
The two unusual features of this case are, documented reinfection with the COVID-19 virus, and perforation of the appendix with an appendicular abscess. A multi-disciplinary discussion was held, and the team decided that the most prudent course of action was to proceed with damage control minimally invasive surgery, followed by definitive treatment after four weeks.
Conclusion
A case of COVID-19 reinfection, with exacerbation of appendicitis, and appendicular perforation,is presented here, managed by laparoscopic peritoneal lavage and drainage, with laparoscopic adhesiolysis and appendicectomy after the reinfection cleared. Emergent surgical patients will continue to present to hospitals, hence surgical departments need to resume providing a high standard of care and not allow themselves to be deterred by COVID-19 management and requirements. To authors’ knowledge no similar case has been reported in English medical literature.
References
- Parreira JG, de Campos T, de Souza Lucarelli Antunes P, Perlin-Geiro JAG, Assef JC. Management of non-traumatic surgical emergencies during the COVID-19 pandemia. Vol. 47, Revista do Colegio Brasileiro de Cirurgioes. Colegio Brasileiro de Cirurgioes; 2020; 47: p. 1–11.
- de Araujo Torres D, do Carmo Bueno Ribeiro L, de Freitas Linhares Riello AP, Horovitz DDG, Pinto LFR, Croda J. Reinfection of COVID‐19 after 3 months with a distinct and more aggressive clinical presentation: Case report. J Med Virol. 2020; jmv.26637.
- Singhal T, Dudek J, Sharmin A, Sudhanva M, Hussain A, El-Hasani S. Ground Plan for Performing Emergency Surgery for Suspected and Confirmed COVID-19 Patients. Ann Color Res. 2020; 8(3): 129–135.
- Coccolini F, Perrone G, Chiarugi M, Marzo F Di, Ansaloni L, Scandroglio I, et al. Surgery in COVID-19 patients: Operational directives. World J Emerg Surg. 2020; 15(1): 25.
- Birch B, Luo Y, Dhir A. How to minimize airborne droplet contamination while performing laparoscopy in the COVID-19 era. ANZ Journal of Surgery. Blackwell Publishing; 2020.
- Zheng H, Ebert HLH, Chatziperi A, Meng W, Smith BH, Yan J, et al. Perioperative management of patients with suspected or confirmed COVID-19: review and recommendations for perioperative management from a retrospective cohort study. Br J Anaesth. 2020; 125: 895–911.
- Neto IJFC, Viana KF, da Silva MBS, da Silva LM, de Oliveira G, da Silva Cecchini AR, et al. Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease. J Coloproctology. 2020; 40(3): 269–72.
- Conservative Management of Acute Appendicitis In The Era Of COVID 19: A Multicenter prospective observational study at The United Arab Emirates,medRxiv - Surgery - X-MOL.
- Suwanwongse K, Shabarek N. Successful Conservative Management of Acute Appendicitis in a Coronavirus Disease 2019 (COVID-19) Patient. Cureus. 2020.
- Patriti A, Baiocchi GL, Catena F, Marini P, Catarci M, Beatrice DV, et al. Emergency general surgery in Italy during the COVID-19 outbreak: First survey from the real life. World J Emerg Surg. 2020; 15(1): 36.
- Zheng C, Chen J, Yan C, Guo C. Surgical management of patients with suspected or confirmed COVID-19: preliminary experience from China. Br J Surg. 2020; 107(10): e442.

