Delayed Diagnosis and Surgical Management for Gluteus Medius/Minimus Calcific Tendinopathy with Heterotopic Ossification: A Case Report
Lasley RJ*, Brismée JM,
Deaprtment of Orthopedics, Spooner Physical Therapy Inc, USA
Deaprtment of Orthopedics, International Academy of Orthopedic Medicine – United States, USA
Deaprtment of Orthopedics, Center for Rehabilitation Research, Texas Tech University Health Sciences Center, USA
Received Date: 29/10/2021; Published Date: 11/03/2021
*Corresponding author: Lasley RJ, Deaprtment of Orthopedics, Spooner Physical Therapy Inc, International Academy of Orthopedic Medicine – United States, USA. Address: 20830 N. Tatum Blvd. Suite 170. Phoenix, AZ 85050, Phone:(480) 502-5510, E-mail:r.lasley@spoonerpt.com
Abstract
A 72-year-old female experienced acute onset right lateral hip pain after repetitive golf swings that a physical therapist originally diagnosed as Greater Trochanteric Pain Syndrome (GTPS). The patient experienced positive gains with physical therapy techniques but eventually reached a plateau in gains and was unresponsive to all physician-based interventions aimed at treating the spine and hip during an 18-month period. An open surgical procedure was performed and revealed calcific tendinopathy of the gluteus medius and minimus and a heterotopic ossification. This finding contradicted numerous imaging studies and physician’s opinions prior to the surgical procedure. The surgical procedure resulted in immediate symptoms’ relief that surpassed all previous interventions and with the help of physical therapy the patient returned to normal as was seen via her Numeric Pain Rating Scale (NPRS) responses and the Hip Disability and Osteoarthritis Outcome Score (HOOS) values.
Keywords: Greater trochanter pain syndrome, calcific tendinosis, heterotopic ossification, hip
Introduction
Mechanical hip pain is difficult to diagnose due to its close proximity to the lumbar spine and pelvis. Lumbar spine pain prevalence is estimated to be 54-84% [1] in a lifetime. The diagnosis of somatic hip pain can be difficult as the lumbar spine can radiate pain and symptoms to the hip region. Konstantinou K et al [2]. found that those with low back pain were 2-42% more likely to report lower extremity radiant symptoms. Due to the potential for lumbar spine-based radiant pain into the lower extremity there might lie a bias towards prematurely diagnosing hip pain as a lumbar spine pathology [3]. Due to the difficulty in diagnosing hip pathology the lumbar spine and pelvis should be ruled out, along with any red flags [4] as potential pain generators prior to treatment. The purpose of this case report is to highlight (1) the clinical reasoning process and diagnosis of Greater Trochanteric Pain Syndrome (GTPS), specifically calcific tendinitis and (2) the positive effect of surgery and physical therapy on the patient’s function and pain.
Case Report
History
A 72-year-old female presented to physical therapy on numerous occasions over an 18-month period with a chief complaint of right lateral hip pain. The patient’s original mechanism of injury was repetitive swinging of a golf club and her initial pain was a dull ache and an occasional catching sensation at the hip’s dorsolateral greater trochanter. Her pain also included radiant tightness that extended to the distal lateral and dorsal thigh (Figure 1) with occasional extension of symptoms to the lateral foot [5]. After numerous secondary opinions (x4), one hip radiograph, three Magnetic Resonance Images (MRIs), one greater trochanteric bursal corticosteroid injection, three lumbar spine epidural steroid injections, and one gluteus medius/minimus tendon platelet-enriched plasma/stem cell injection [6] she was finally diagnosed post-surgically with calcific tendinitis of the gluteus medius/minimus tendon with the presence of a heterotopic ossification.
Examination
The patient had no previous medical history of right hip or lumbar spine pain. Her pain on the Numeric Pain Rating Scale (NPRS) at the time of the initial evaluation was 1/10 with 8/10 reported at its worst. The patient was taking prescription strength anti-inflammatories (Ibuprofen 800mg) as well as other existing prescriptions Synthroid, Lipitor, and Singulair. Lateral and dorsal hip structures visualization indicated gluteal atrophy. The patient demonstrated an antalgic compensatory Trendelenburg gait pattern and a positive single leg balance test that generated right hip pain in standing. Supine passive range of motion hip flexion, external rotation from 90° of hip flexion, and prone internal rotation from a 0° hip position were all painful with no deficits in motion. Resisted hip flexion, adduction from 90° of flexion, side lying abduction and prone internal rotation demonstrated normal strength grades with all causing lateral hip pain. Supine gluteus medius and maximus bursal testing through passive hip flexion, adduction and external/internal rotation generated lateral hip pain. Palpation of the gluteal tendon insertions (Figure 2) on the proximal dorso-lateral greater trochanter along with the ischial tuberosity were painful. The patient displayed numerous spinal and pelvic ring positive tests including a right lower extremity straight leg raise test [7] with symptom changes experienced with cervical flexion and ankle plantar flexion actions, sacroiliac dorsolateral and ventromedial tests, and a supine thigh thrust test. In prone on elbows position the L5 spinous process was more pronounced when compared to a prone position indicating a potential L5 retrolisthesis and lastly, the patient demonstrated right lower extremity altered dermatomal sensation in the S1 nerve distribution.
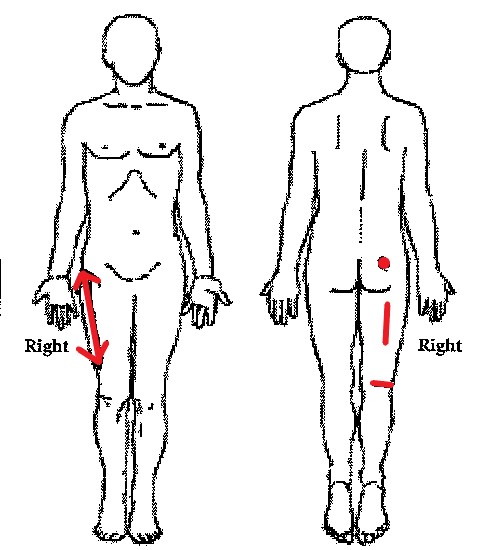
FIGURE 1: Patient’s original hip pain location - August 2018
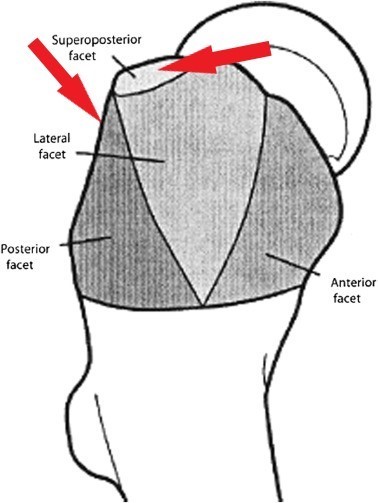
FIGURE 2: Patient’s painful palpation location
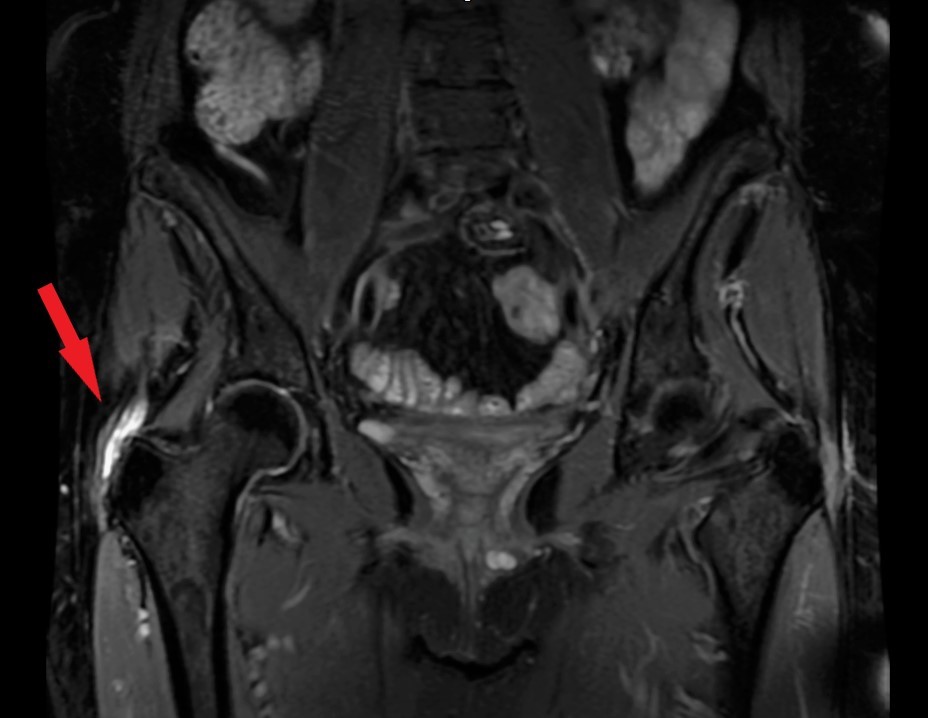
FIGURE 3A: Frontal-Plane Magnetic Resonance Image of Hip Gluteal Tendon Tears and Possible Heterotopic Ossification
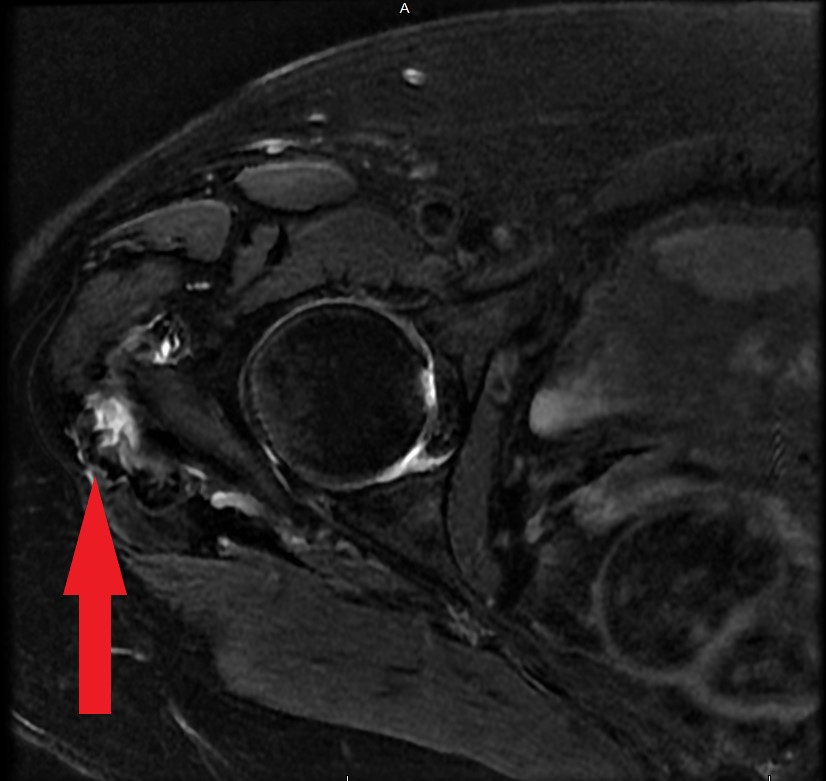
FIGURE 3B: Transverse-Plane Magnetic Resonance Image of Hip Gluteal Tendon Tears and Possible Heterotopic Ossification
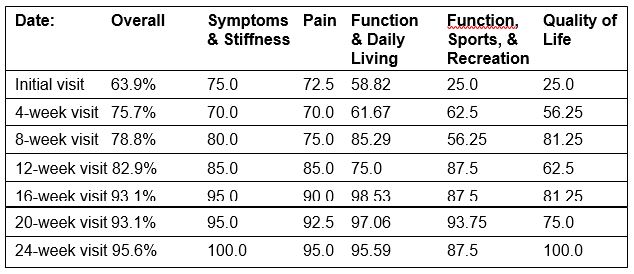
TABLE 1. Patient’s Hip Disability and Osteoarthritis Outcome Scores (HOOS)
Clinical Impression
Following a thorough physical therapy lumbar spine and hip examination it was determined that the patient’s pain originated at the hip (gluteus medius muscle, gluteal bursae) with a diagnosis of GTPS. Once hip images were obtained and viewed (Figures 3A & B) GTPS was confirmed. The diagnosis of GTPS was further corroborated by the surgical procedure 18-months later that found gluteus medius/minimus calcific tendinitis and the presence of a heterotopic ossification. The radiant symptoms into the lower extremity were initially deemed the result of lumbar spine radiculopathy from central and/or foraminal canal diameter changes due to degenerative disc disease and a L5 retrolisthesis, which was verified by the lumbar spine MRI. Differential diagnosis of sciatic nerve irritation was possible sensitization resulting from the concurrent GTPS.
Treatment/Intervention
Treatment originally addressed the potential contribution of the lumbar spine and sciatic nerve irritation through lumbar spine soft tissue mobilization, intervertebral foraminal space opening techniques (3-D lumbar spine axial separation), and neural flossing techniques for nerve mobility and swelling reduction [8]. Initially, until surgical correction, the local hip pain was treated with the application of transverse friction [9] to the insertion of the gluteus medius and minimus tendons at the greater trochanter with initial positive benefits that unfortunately plateaued over time. To address core muscle weakness neuromotor exercises were prescribed [10]. To address hip neuromotor control and strength deficits select hip muscle activation and strengthening exercises [11] were performed and progressed per Haff and Triplett [12]. The outcomes of these interventions did not result in sustained pain and function improvements therefore a surgical procedure was performed.
Post-surgical wound and scar deficits were regularly treated through soft tissue techniques until absence of sensitivity to touch. Hip motion deficits (flexion, abduction, internal/external rotation) were addressed through physical therapy manual therapy techniques until normalizations were achieved. The patient again started core [10] and hip [11] neuromotor exercises, which were progressed slowly until strength, gait, and function were normalized. The patient’s home exercise program reinforced the exercises described by Distefano et al [11]. with instructions to perform at least three times per week.
Outcome & Follow-Up
The patient’s surgical procedure resulted in immediate post-surgical improvement in pain per the NPRS and ability per the Hip Disability and Osteoarthritis Outcome Score [13] when comparing pre- and post-surgical values. Over the course of 23 physical therapy sessions the patient’s NRPS improved to 0/10 at best and 1/10 at its worst and an overall HOOS score of 93.1% (TABLE 1). At 6 and 12-week follow-up the NPRS and HOOS improvements were sustained.
Discussion
Diagnosing and then managing GTPS is multifactorial and can take more than three years to achieve [14]. Gluteus Medius calcific tendinitis is uncommon with reported values lower than the more common shoulder variation [15]. Typically, calcific tendinitis is self-limiting and can be treated with rest, nonsteroidal anti-inflammatory drugs, and physiotherapy however it can progress and become chronic. This case highlights the difficulty in diagnosing hip pain as there was concern originally that the spine was the cause for the patient’s hip pain. Practitioners should be prepared to rule out spinal nociceptive pain, somatic referred pain, radicular pain, and radiculopathy if they want to effectively treat the hip. In this case, lumbar MRI indicated degenerative disc disease and a L5 retrolisthesis while the patient clinical presentation was consistent with pain of spinal origin (below the knee radiant pain, S1 dermatomal numbness, S1 myotomal weakness, positive neurodynamic testing). Spine pain assumptions were then questioned since repeated lumbar spine epidural steroid injections did not affect the symptoms. The lateral hip and radiant thigh pain that remained were reproduced by the physical therapy hip examination and revealed numerous signs and symptoms concurrent with GTPS [5]. The lateral hip and radiant thigh pain is best described as being the result of somatic nociceptive radiant pain patterns into pathways mimicking spinal nerve roots [6] much like sciatic nerve sensitization seen with hamstring syndrome. The work by Eliav et al [16]. Further expands on the potential for neural sensitization as they were able to induce, with no apparent axonal loss, pain-related behaviors, hyperalgesia, and allodynia with sensory testing in a rat’s saphenous nerve distribution through the induction of an inflammatory process at the peripheral nerve.
In this case GTPS treatment, including physical therapy and injectional therapy included corticosteroid, tendon platelet-enriched plasma and stem cell injections [17] plateaued and required a surgical procedure to treat what was thought to be a MRI verified gluteus medius/minimus tear only to find out the MRI images were mistaken and there was actually intra-operatively verified calcific tendinitis and a heterotopic ossification. Westacott et al [18]. attest to MRI’s potential false-positives for gluteal tendon tears due to its 33-100% sensitivity, 92-100% specificity, while Almedghio and Garneti [19] found that calcific tendinitis can mimic infection or muscle tearing on MRI because of extensive bursal fluid, soft tissue, and muscle edema.
Conclusion
This patient’s 22-month experience with gluteus medius/minimus calcific tendinitis and heterotopic ossification highlights the difficulty both physicians and physical therapists have in diagnosing and treating GTPS. A detailed history and examination, the prescription of appropriate imaging studies, understanding potential imaging false positives, and the continued advocacy on behalf of the patient resulted in a surgical procedure that, when combined with skilled physical therapy, allowed for immediate and long-term sustained improvements.
References
- Samolsky Dekel BG, Sorella MC, Vasarri, A, Melotti RM. Reliability of the buttock applied strain test to diagnose radicular pain in patients with low back pain. Pain Pract. 2020. doi: 10.1111/papr.12890.
- Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine. 2008; 33: 2464-2472. doi: 10.1097/BRS.0b013e318183a4a2.
- Sembrano JN, Polly DW. How often is low back pain not coming from the back? Spine (Phila Pa 1976). 2009; 1: 34(1): E27-32. doi:10.1097/BRS.0b013e31818b8882.
- Verhagen AP, Popal N, Maher C, Koes BW. Red flags presented in current low back pain guidelines: a review. Eur Spine J. 2016; 25(9): 2788-2802. doi: 10.1007/s00586-016-4684-0. Epub 2016 Jul 4.
- Grimaldi A, Mellor R, Nicolson P, Hodges P, Bennell K, Vicenzino B. Utility of clinical tests to diagnose mri-confirmed gluteal tendinopathy in patients presenting with lateral hip pain. Br J Sports Med. 2017; 51(6): 519-524. doi: 10.1136/bjsports-2016-096175. Epub 2016 Sep 15.
- Torres A, Fernandez-Fairen M, Sueiro-Fernandez J. Greater trochanteric pain syndrome and gluteus medius and minimus tendinosis: nonsurgical treatment. Pain Manag. 2018; 8(1): 45-55. doi: 10.2217/pmt-2017-0033. Epub 2017 Nov 28.
- Majlesi J, Togay H, Unalan H, Toprak S. The sensitivity and specificity of the slump and the straight leg raising tests in patients with lumbar disc herniation. J Clin Rheumatol. 2008; 14(2): 87-91. doi: 10.1097/RHU.0b013e31816b2f99.
- Efstathiou MA, Stefanakis M, Savva C, Giakas G. Effectiveness of neural mobilization in patients with spinal radiculopathy: a critical review. J Bodyw Mov Ther. 2015; 19(2): 205-212. doi: 10.1016/j.jbmt.2014.08.006. Epub 2014 Aug 17.
- Brosseau L, Casimiro L, Milne S, Robinson V, Shea B, Tugwell P, Wells G. Deep transverse friction massage for treating tendinitis. Cochrane Database Syst Rev. 2002; (1): CD003528.
- Kavcic N, Genier S, McGill SM. Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises. Spine. 2004; 29: 2319-2329.
- Distefano LJ, Blackburn TJ, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009; 39(7): 532-540. doi: 10.2519/jospt.2009.2796.
- Haff GG, Triplett NT. Essentials of Strength Training, 4th ed. Champaign, IL: Human Kinetics, Inc; 2015.
- Nilsdotter A, Bremander A. Measures of hip function and symptoms: harris hip score (hhs), hip disability and osteoarthritis outcome score (hoos), oxford Hip score (ohs), lequesne index of severity for osteoarthritis of the hip (lisoh), and american academy of orthopedic surgeons (aaos) hip and knee questionnaire. Arthritis Care Res. 2011; 63 Suppl 11: S200-207. doi: 10.1002/acr.20549.
- Domb BG, Botser I, Giordano BD. Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med. 2013; 41: 988–997.
- Siegal DS, Wu JS, Newman JS et al. Calcific Tendinitis: A Pictorial Review. Can Assoc Radiol J. 2009 Dec;60(5):263-272. DOI: 10.1016/j.carj.2009.06.008
- Eliav E, Herzberg U, Ruda MA, Bennett GJ. Neuropathic pain from an experimental neuritis of the rat sciatic nerve. Pain. 1999; 83: 169-182.
- Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2013; 12: CD010071. doi: 10.1002/14651858.CD010071.pub2.
- Westacott DJ,. Th Minns JI, Foguet P. The diagnostic accuracy of magnetic resonance imaging and ultrasonography in gluteal tendon tears--a systematic review. Hip Int. 2011; 21(6): 637-645. doi: 10.5301/HIP.2011.8759.
- Almedghio S, Garneti N: The acute and chronic presentation of gluteus medius calcific tendinitis- a case report of two. J Orthop Case Rep. 2014; 4: 48–50.

