Migration of Rod into the Posterior Cranial Fossa, After C1-C2 Laminar Hooks Fusion: Case Report and Literature Review
Marouane Hammoud*, Rafik Al Hallak
Department of Neurosurgery, Hassan II University Hospital of Fez, Morocco
Departement of neurosurgery, Jean Bernard Hospital, Valenciennes, France
Received Date: 04/02/2021; Published Date: 17/02/2021
*Corresponding author: Medicine doctor, Department of Neurosurgery, Hassan II University Hospital of Fez, University Sidi Mohammed Ben Abdellah, Fez, Morocco. Email: marouane.hammoud@gmail.com.
Abstract
Background: Posterior atlantoaxial fusion is a common surgical technique for the treatment of upper cervical spine disability. Although, Contemporary laminar hook–rod systems offer reliable rigid immobilisation of adjacent vertebrae in the upper cervical spine. However, it carries the risks of fracture or migration, with associated potential life-threatening complications.
Case presentation: Herein, we report a case of 56 YO women who underwent posterior cervical C1-C2 fusion using contemporary laminar-hooks for odontoid type II fracture. 6 weeks after surgery, a routine CT scan control, showed migration of the rod in the posterior fossa and perforation of the skull with a head pin placement, though the patient was asymptomatic. We decided to remove all the instruments, after surgery, the patient was doing well, CT scan control showed evidence fusion of the fracture, we concluded that the missing rod was not well locked and had perforated the occipital bone.
Keywords: Posterior atlantoaxial fusion; Cervical spine; Complication; Rod migration.
Introduction
Posterior Atlantoaxial Fusion (PAAF) is used for the treatment of atlonto axial instability including trauma like odontoid fracture, congenital malformation like os odontoideum, rheumatoid arthritis, tumor, and infection [1].
Over the past decade, several techniques of PAAF have been described with improved safety profile, higher fusion rates, and superior clinical outcome [2].
However, there are various complications associated with PAAF that can negatively impact patient outcome [3].
In this paper, we describe an uncommon complication of rod migration into the posterior cranial fossa after PAAF using C1-C2 laminar hooks fusion.
Case Presentation
A 56 YO women with no medical history, presented cervical spine injury with no neurological impairment resulting from a traffic accident, Cervical CT Scan showed an anderson-D’alonzo Type II forward sloping odontoid fracture with anterior displacement and intact posterior C1 arch (Figure 1).
1 day after the injury, she underwent a C1-C2 posterior fusion using C1-C2 laminar hooks connected with two rods (Figure 2), followed by immobilization with a cervical collar for 6weeks. The postoperative course was uneventful.
6 weeks later, at the follow up visit, checked CT scan revelled consolidation of the fracture and migration of the right rod into the posterior cranial fossa (Figure 3). Luckily the patient had no neurological symptoms,
The patient had undergone the revision operation the day after; we decided to remove all the instruments because cervical CT Scan showed evidence of fusion across the odontoid fracture. The migrated rod was removed carefully.
Post- operative neck immobilization was emphasized to patient once more, and closed follow-up was planned.

Figure1: Sagittal CT Scan showing Type II odontoid fracture.
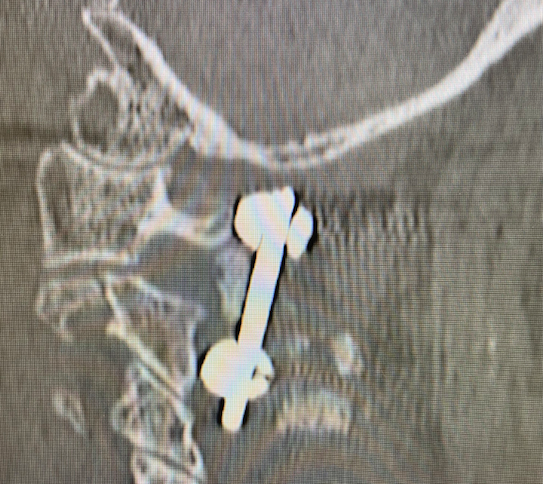
Figure 2: Sagittal CT Scan following initial fusion.

Figure 3: CT Scan reconstruction showing rod migration into the posterior fossa.
DISCUSSION
Odontoid fractures account for 9% to 15% of adult cervical spine fractures with the majority being type II fractures according to the Anderson and D’Alonzo classification [4].
In the elderly population, these fractures are the most common upper cervical spine fracture and, in the population, older than 80 years, the most common spine fracture of all.
These injuries usually result from hyperflexion or hyperextension of the cervical spine during low-energy impacts in the elderly or high-energy impacts in the young and middle aged. Neurologic injury associated with these fractures is rare [5-7].
The management of odontoid fractures is challenging, particular in the elderly. The objective is a rapid restoration of autonomy while limiting morbidity and mortality due to prolonged immobilisation [8].
Multiple factors determine the management of odontoid fracture, including fracture type, presence of associated fracture of the posterior elements, patient age and comorbidities. Generally, type I and type III injuries require non-operative treatment [9]. Type II often require surgical treatment, however there is no clearly consensus concerning the technique to use [10].
To overcome this pitfall, Roy-Camille proposed a classification based on the evaluation of the risk of displacement [11]: Type II with backward sloping or horizontal fractures can be managed by anterior screw fixation of the odontoid. The association with forward sloping fracture is an indication for posterior fusion [12].
Several techniques can be used for cervical posterior fusion, in the last decade, techniques based on instrumentation of lateral masses of C1/pedicles of C2 (Harms or Goel technique), and C1/C2 joints (Magerl’s technique) became popular [13,14], However they are technically more demanding and have the added risk of serious complications; Vertebral artery injury is the most common complication [15].
In contrast to Harms and Magerl’s techniques, posterior fixation with modern laminar claw hook–rod instrumentation is a safe and effective technique with comparable results in terms of fusion and neurological improvement. Also, it is technically less demanding with a lower morbidity [16], but it requires intact posterior elements.
Regardless of specific methods and instruments, a variety of complications have been reported following posterior spine fusion. In a reports published by Lall et al. [17], the most commonly encountered perioperative complications were related to instrumentation failure after non-union. Other commonly encountered complications included injury to the vertebral artery, dural tears, and wound infection. But, the screw fracture after trans-pedicle screws and screw-rod constructs is very rare with no relevant article in the literature review [18].
A quite rare complication of rod migration into the posterior cranial fossa as shown in the present case, was reported by Chun et al. [19]. A similar case was also reported by Plant et Ruff [20]. The authors of both cases have no culprit that the migration of the rod was attributed to any operative technical errors.
In the current case, we conclude that the rod was not well locked, then eroded the occipital bone, and finally migrated into the posterior fossa.
Conclusion
Spine surgeons should be thoroughly informed that failure of assembled instrumentation failure can occur without obvious causes, thus long-term follow-up should be performed in order to identify any early migration.
References
- Jacobson ME, Khan SN, An HS. C1-C2 Posterior Fixation: Indications, Technique, and Results. Orthop Clin North Am. janv 2012.
- Chen Q, Brahimaj BC, Khanna R, Kerolus MG, Tan LA, David BT, et al. Posterior atlantoaxial fusion: a comprehensive review of surgical techniques and relevant vascular anomalies. J Spine Surg. Mars 2020.
- Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA. Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg. mars 2020.
- Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Jt Surg Am Vol. déc 1974; 56(8):1663‑1674.
- Maak TG, Grauer JN. The contemporary treatment of odontoid injuries. Spine. 15 mai 2006; 31(11 Suppl): S53-60; discussion S61.
- Gonschorek O, Vordemvenne T, Blattert T, Katscher S, Schnake KJ. Treatment of Odontoid Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob Spine J. sept 2018.
- Faure A, Graillon T, Pesenti S, Tropiano P, Blondel B, Fuentes S. Trends in the surgical management of odontoid fractures in patients above 75 years of age: Retrospective study of 70 cases. Orthop Traumatol Surg Res. 2017.
- Geriatric spine fractures: an emerging healthcare crisis. - Abstract - Europe PMC.
- Ochoa G. Surgical management of odontoid fractures. Injury. 2005; 36 Suppl 2: B54-64.
- Ben Aïcha K, Laporte C, Akrout W, Atallah A, Kassab G, Jégou D. Surgical management of a combined fracture of the odontoid process with an atlas posterior arch disruption: A review of four cases. EM-Consulte.
- Roy-Camille R, Saillant G, Judet T, De Botton G, Michel G. Facteurs de gravité des fractures de l’odontoïde. Rev Chir Orthop. 1980; 66: 183-186.
- Hadley MN, Walters BC, Grabb PA, Oyesiku NM, Przybylski GJ, Resnick DK, et al. Management of combination fractures of the atlas and axis in adults. Neurosurgery. mars 2002; 50(3 Suppl): S140-147.
- Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994.
- Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001; 26(22): 2467‑2471.
- Gluf WM, Schmidt MH, Apfelbaum RI. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 191 adult patients in: Journal of Neurosurgery: Spine 2005; 2(2).
- Litrico S, Pennes F, Charbek S, Paquis P. Interest of laminar hooks in fixation of craniocervical junction. In Joint Annual Meeting EANS-SFNC EANS Annual Meeting (Formerly Winter Meeting) and the Annual Meeting of the SFNC; 2009.
- Lall R, Patel NJ, Resnick DK. A review of complications associated with craniocervical fusion surgery. Neurosurgery. 2010; 67(5): 1396‑1402; discussion 1402-1403.
- Oh CH, Ji GY, Seo HS, Yoon SH, Hyun D, Park H-C. Repeated Complication Following Atlantoaxial Fusion: A Case Report. Korean J Spine. 2014.
- Chun H-J, Bak KH, Kang TH, Yi H-J. Rod Migration into the Posterior Fossa after Harms Operation: Case Report and Review of Literatures. J Korean Neurosurg Soc. 2010.
- Plant JGA, Ruff SJ. Migration of rod through skull, into brain following C1-C2 instrumental fusion for os odontoideum: a case report. Spine. 2010; 35(3): E90-92.

