Isolated Vestibulopathy: A Potentially Unrecognized Presentation of COVID-19
Cody J Falls, Yanchen Zhang, Michael D Puricelli,*
Division of Otolaryngology, University of Wisconsin-Madison School of Medicine and Public Health, USA.
Division of Otolaryngology, University of Wisconsin Hospitals and Clinics, USA.
Received Date: 01/02/2021; Published Date: 16/02/2021
*Corresponding author: Michael D Puricelli, University of Wisconsin-Madison School of Medicine and Public Health, Madison, University of Wisconsin Hospitals and Clinics, 600 Highland Avenue Room MC 7375; Madison, WI 53792-7375, USA. Phone: (608) 262-7181, Email: mpuricelli@wisc.edu
Abstract
COVID-19 infection presents differently in adults and children, with an increasingly understood range of symptoms. Neurotropic properties of COVID-19 have been shown to contribute to taste and smell disturbance as well as disequilibrium in adults. This is the first report, to our knowledge, of a pediatric COVID-19 patient with vertigo as the sole presenting symptom. Routine examination in these patients may include head impulse testing, assessment for nystagmus, test of skew and hearing assessment. A low threshold for COVID-19 testing in typical and atypical presentations should be entertained as well as adequate personal protective equipment for higher risk diagnostic maneuvers.
Keywords: Vestibular neuritis; COVID-19; SARS-CoV-2; Dizziness; Vertigo.
Introduction
Fever/chills, cough, shortness of breath/difficulty breathing, fatigue, muscle/body aches, headache, sore throat, nasal congestion, rhinorrhea, nausea/vomiting, diarrhea and loss of taste/smell are features of COVID-19 [1]. Pediatric patients generally show milder symptoms than adults, and typical symptoms include cough, sore throat, fever, and/or diarrhea [1,2]. Current best estimates show up to 40% of infectious individuals including both adults and children may be clinically asymptomatic, though it is known children are asymptomatic at higher rates [1,3]. Smell and taste dysfunction related to the neurotropic characteristics of COVID-19 received much attention as diagnostically significant presenting symptoms. Additionally, 18.4% of adult patients with COVID-19 indicate equilibrium symptoms [4]. In some adult cases, dizziness may be the sole presenting symptom [5]. The frequency of balance symptoms in COVID-19 infected pediatric patients is unknown; and to the authors’ knowledge, vertigo as the sole presenting symptom of a pediatric patient with COVID-19 has not yet been described in literature.
We report the first case of vertigo as the sole presenting symptom in a pediatric patient with COVID-19.
Case Report
A 15-year-old male with no pertinent past medical history presented to the emergency department with intractable dizziness, nausea, vomiting, and subjective right-sided hearing loss. Balance symptoms began the day of presentation, though some hearing difference was noted over the preceding weeks to months. While the patient had no other symptoms, a family member had been recently diagnosed with COVID-19. As a result of his COVID exposure, the patient was tested and found to be negative for COVID seven days prior to presentation. In the immediate period following his negative COVID test, he was found to have 1-2 days of clear rhinorrhea without fever or cough which spontaneously resolved several days prior to ED presentation.
On examination, horizontal nystagmus was present and hearing assessment by tuning fork was normal. Gait testing was not performed due to marked dizziness. Further neurological exam revealed no abnormalities.
Fast stroke MRI/MRA with and without contrast revealed no evidence of acute infarction, hemorrhage, or other abnormalities with patent major intracranial arteries and veins and no abnormal enhancement. Antiemetics and vestibular suppressants were administered and COVID-19 testing was ordered prior to admission. COVID-19 testing returned positive. The patient received supportive treatment and corticosteroids were administered. Vestibular suppressants were discontinued as soon as vertigo improved and physical therapy consultation was completed prior to discharge. Formal audiometry after discharge revealed normal hearing.
Discussion
Vestibular neuritis is an acute peripheral vestibulopathy typically presenting with hours to days of continuous vertigo. It frequently follows upper respiratory infection and is commonly attributed to neurotropic viral reactivation of latent HSV-1[6,7]. The superior division of the vestibular branch of the vestibulocochlear nerve is preferentially affected, causing dysfunction of the superior semicircular canal, lateral semicircular canal, and utricle, while sparing hearing [7]. Accordingly, patients present with hours to days of severe vertigo, nausea, vomiting, and gait instability with typical exam findings consisting of spontaneous horizontal/torsional nystagmus contralateral to the affected side, abnormal head thrust test for the involved semicircular canals, ipsilateral caloric paresis, unsteady gait with falls towards the affected side, and nystagmus suppressible with visual fixation[7]. Nystagmus intensity also typically increases with gaze in the direction of the fast phase (Alexander’s Law).
Symptoms can be debilitating and overlap with those of acute cerebrovascular accident of the cerebellum or brain stem[1,8]. The most widely accepted exam technique to differentiate central versus peripheral etiologies of vertigo is the HINTS plus protocol. The HINTS plus protocol involves 4 components: Head Impulse testing, Nystagmus, Test of Skew, plus hearing loss. A negative central finding in all four of the exam components (when performed by an expert) has a sensitivity for detecting central origins of abrupt-onset vertigo of 99.2% (Figure 1a-1c) [9]. In contrast, a positive central finding in any category other than hearing loss has a specificity of 96% for stroke [9]. This exam is very important clinically as it is more sensitive in detecting early (first 24-48 hours) posterior circulation strokes than the preferred imaging modality, MRI DWI [9].
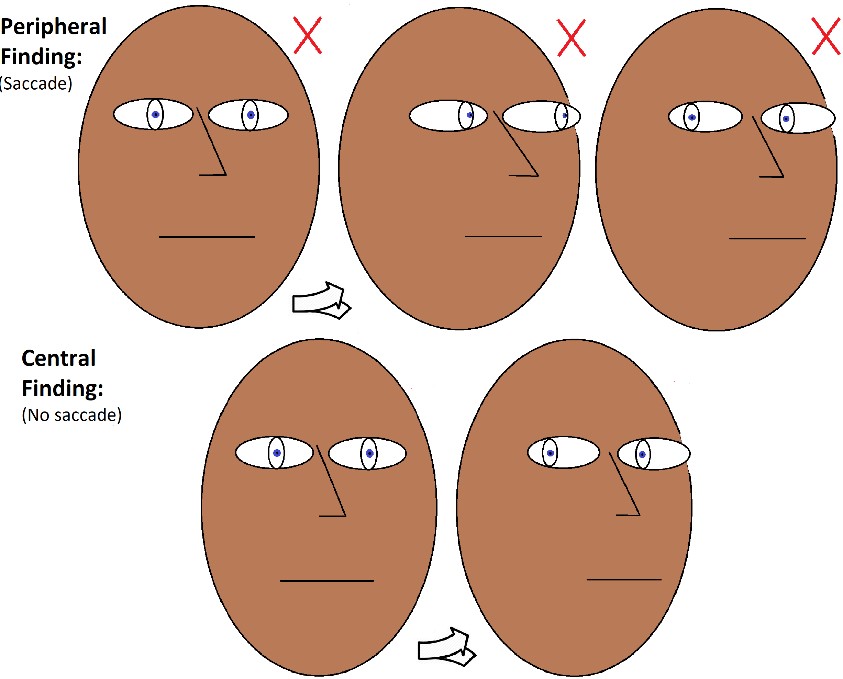
Figure 1: Head thrust exam. Central versus peripheral findings. HI of HINTS protocol
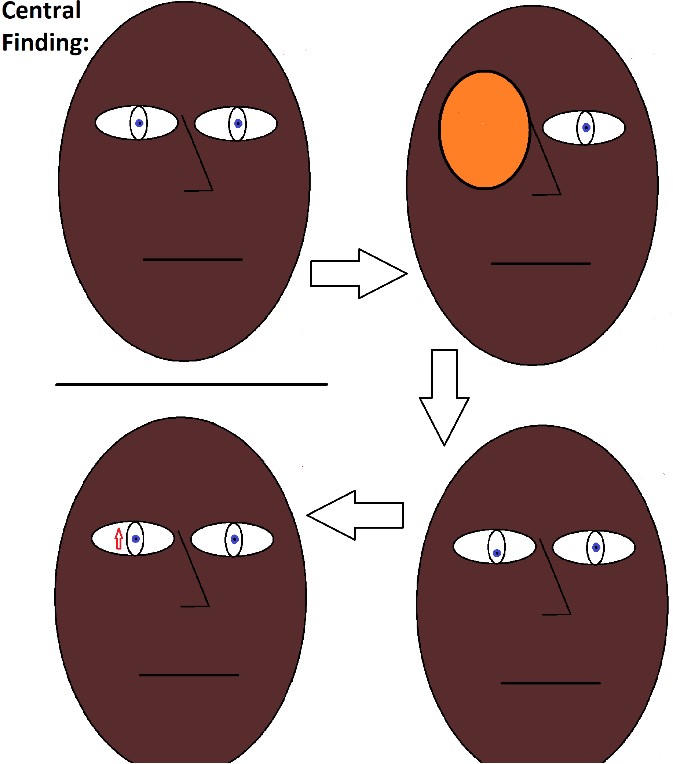
Figure 2: Deviation of skew with a positive central finding. TS of HINTS protocol.
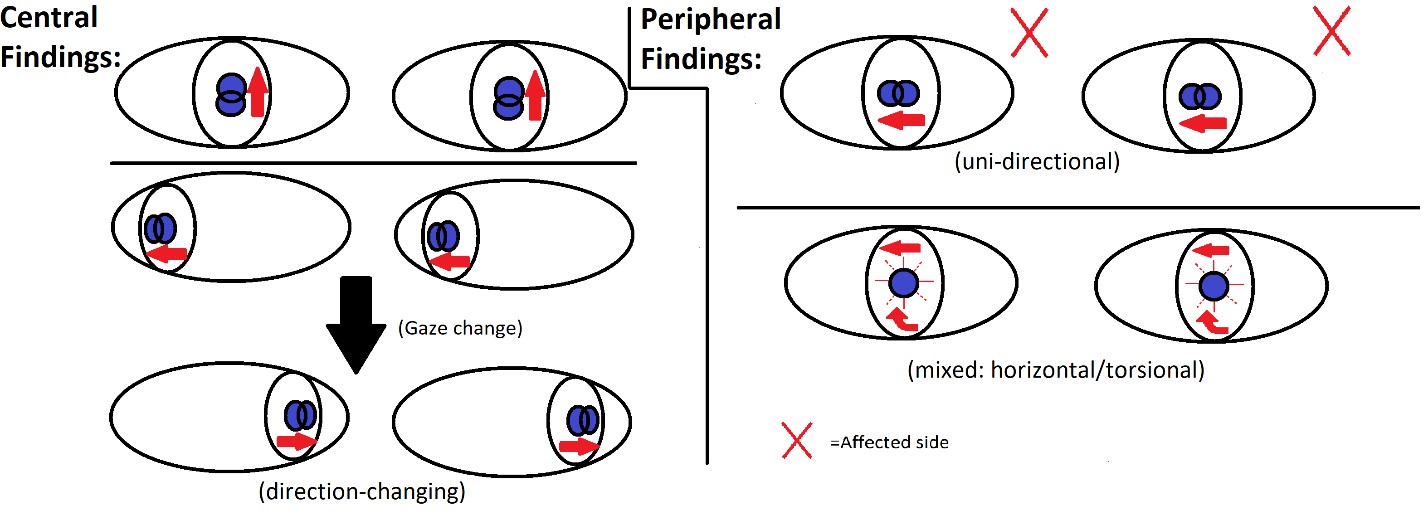
Figure 3: Central versus peripheral nystagmus findings. N of HINTS protocol.
Acute treatment for vestibular neuritis may include a short course of vestibular suppressing agents or antiemetics and vestibular rehabilitation as soon as able to be tolerated. Vestibular suppression should be limited to as short of a period as possible as there is evidence these agents can delay central compensation [10]. Glucocorticoid treatment is controversial as various studies have produced conflicting results, though most current research points towards foregoing the use of glucocorticoids unless clinical concern exists for sudden sensorineural hearing loss (labyrinthitis) as it provides no long term benefit over vestibular rehab therapy and comes with a host of possible side effects [11].
Performance of diagnostic tests may exacerbate dizziness symptoms and induce gag and vomiting. While COVID-19 is identified at the greatest concentration in respiratory secretions, it is also present in saliva, tears and cerumen. The presence of infectious virus in vomit is unknown; however, vomiting has previously been identified as a mechanism of transmission of SARS-CoV [12–14]. Further study of the frequency of COVID-19 attributable vestibular neuritis and infectious risk will guide appropriateness of COVID-19 testing and personal protective equipment use in these situations. Identification of less common presentations is important to making testing recommendations and mitigating viral spread.
Conclusion
This is the first case to the authors’ knowledge of vertigo as the sole presenting symptom of COVID-19 in a pediatric patient. Elucidation of all presenting signs and symptoms is important for diagnostic purposes and to ensure appropriate precautions when managing potentially infectious individuals. Additionally, given the potential role of asymptomatic/minimally symptomatic children in community spread of COVID-19, identification of atypical or minimally symptomatic presentations of COVID-19 may play a role in the early identification and containment of COVID-19 spread by the pediatric population [13]. Given these factors, a low threshold should be entertained for COVID-19 testing as well as use of personal protective equipment for these patients. Further study of vertiginous symptoms in pediatric COVID-19 patients is warranted.
Authorship Criteria
All authors contributed significantly to the primary draft, revision, as well as critical analysis.
Conflicts of interest
The authors have no relevant conflicts of interest to disclose.
Funding
No specific funding was obtained for this work.
Grant Information
The authors received no specific funding for this work.
References
- A Meta‐Analysis of 67 Studies with Presenting Symptoms and Laboratory Tests of COVID‐19 Patients - Mair - - The Laryngoscope - Wiley Online Library, (n.d.). https://onlinelibrary.wiley.com/doi/10.1002/lary.29207.
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 Among Children in China, Pediatrics. 145 (2020). https://doi.org/10.1542/peds.2020-0702.
- CDC, Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. (2020). https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html.
- Viola P, Ralli M, Pisani D, Malanga D, Sculco D, Messina L, et al. Tinnitus and equilibrium disorders in COVID-19 patients: preliminary results, Eur Arch Otorhinolaryngol. (2020). https://doi.org/10.1007/s00405-020-06440-7.
- Sia J. Dizziness can be an early sole clinical manifestation for COVID-19 infection: A case report, J Am Coll Emerg Physicians Open. (2020). https://doi.org/10.1002/emp2.12185.
- Suzuki S. [Detection of latent herpes simplex virus in human vestibular ganglia], Hokkaido Igaku Zasshi. 71 (1996) 561–571.
- Strupp M, Brandt T. Vestibular neuritis, Semin Neurol. 2009; 29: 509–519. https://doi.org/10.1055/s-0029-1241040.
- Zhou Z, Kang H, Li S, Zhao X. Understanding the neurotropic characteristics of SARS-CoV-2: from neurological manifestations of COVID-19 to potential neurotropic mechanisms, J Neurol. 2020; 267: 2179–2184. https://doi.org/10.1007/s00415-020-09929-7.
- Newman-Toker DE, Kerber KA, Hsieh YH, Pula JH, Omron R, Saber Tehrani AS, et al. HINTS outperform ABCD2 to screen for stroke in acute continuous vertigo and dizziness, Acad Emerg Med. 2013; 20: 986–996. https://doi.org/10.1111/acem.12223.
- Hain TC, Uddin M. Pharmacological treatment of vertigo, CNS Drugs. 2003; 17: 85–100. https://doi.org/10.2165/00023210-200317020-00002.
- Ismail EI, Morgan AE, Abdel Rahman AM. Corticosteroids versus vestibular rehabilitation in long-term outcomes in vestibular neuritis, Journal of Vestibular Research. 2018; 28: 417–424. https://doi.org/10.3233/VES-180645.
- Morawska L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air. 2006; 16: 335–347. https://doi.org/10.1111/j.1600-0668.2006.00432.x.
- Morawska L, Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality, Environ Int. 2020; 139: 105730. https://doi.org/10.1016/j.envint.2020.105730.
- Hanege FM, Kocoglu E, Kalcioglu MT, Celik S, Cag Y, Esen F, et al. SARS-CoV-2 Presence in the Saliva, Tears, and Cerumen of COVID-19 Patients, Laryngoscope. (2020). https://doi.org/10.1002/lary.29218.

