Inverted, Ulcerated Meckel’s Diverticulum as a Cause of Occult GI Bleed
Hampton B Sasser*1, Andrew S Brock2
1Department of Medicine, Internal Medicine Resident, Medical University of South Carolina, USA
2Department of Medicine, Division of Gastroenterology and Hepatology, Medical University of South Carolina, USA
Received Date: 28/10/2020; Published Date: 10/12/2020
*Corresponding author:Hampton B Sasser, Department of Medicine, Internal Medicine Resident, Medical University of South Carolina, 96 Jonathan Lucas St., MSC 623, Suite 807E Clinical Science Bldg. Charleston, SC 29425, USA. E-mail: sasserh@musc.edu, Phone: 843-870-4588, Fax: 843-792-0448
Abstract
Meckel’s diverticulum is the most common congenital malformation of the GI tract, though is rarely encountered in adulthood. Symptomatic Meckel’s diverticula in adults most often manifest by bleeding. In this case, an elderly woman presented with symptomatic anemia which was ultimately due to occult GI bleed from an inverted, ulcerated Meckel’s diverticulum. Capsule endoscopy, computed tomography, and balloon-assisted enteroscopy all aided in the diagnosis. Surgical resection confirmed the diagnosis and also served as definitive treatment.
Keywords: Meckel’s diverticulum; Occult GI bleed; Anemia; Capsule endoscopy; Balloon-assisted enteroscopy; Single balloon enteroscopy
Introduction
Meckel’s diverticulum is the most common congenital malformation of the GI tract. The majority of Meckel’s diverticula go undetected and remain asymptomatic. [1,2] Symptomatic Meckel’s diverticula tend to present in childhood with symptoms of obstruction. In adults, bleeding is the most common cardinal symptom.
Case Report
A 65-year-old woman presented with weakness, fatigue, decreased appetite, and weight loss. She denied abdominal pain, melena, or hematochezia. She had been taking meloxicam daily for osteoarthritis. Review of systems was otherwise negative. Past medical history was notable for breast cancer that was treated with modified radical mastectomy 15 years prior. She was up to date on age-appropriate cancer screening and had undergone colonoscopy two years prior. Laboratory testing revealed a hemoglobin of 4 gm/dL so the patient was subsequently admitted to her local hospital for blood transfusion and further workup.
The patient had normal vital signs and an unremarkable physical exam, including abdominal exam. Due to concern for obscure GI bleed, the patient underwent colonoscopy and esophagogastroduodenoscopy which did not find a source of blood loss. CT abdomen and pelvis with IV contrast was normal as well. Capsule endoscopy was subsequently performed and revealed a large polypoid mass in the mid to distal ileum with scant blood nearby. CT enterography failed to demonstrate the intraluminal small bowel mass that was seen with capsule endoscopy and nuclear medicine Tc-99m pertechnetate scintigraphy (Meckel’s scan) did not suggest Meckel’s diverticulum.
She was referred to our facility for retrograde single balloon enteroscopy. This revealed a 5 cm ulcerated submucosal mass in the mid ileum, about 80 cm proximal to the ileocecal valve (Figure 1, 2). Biopsies were taken of the mass and pathology revealed benign reactive small bowel mucosa with edema and evidence of ulceration without evidence of dysplasia or malignancy; however, a submucosal mass lesion could not be excluded. Given the continued concern for malignancy, the patient was referred to colorectal surgery at our institution for resection of the suspect neoplasm. Staging scans including CT of the chest, abdomen, and pelvis were negative for metastases. However, CT of the abdomen and pelvis with IV contrast did reveal an intraluminal, blind-ending structure in the mid to distal ileum suggestive of an invaginated Meckel’s diverticulum (Figure 3). She underwent successful laparoscopic small bowel resection and anastomosis. Pathology of the resected tissue revealed benign small bowel mucosa with intraluminal small bowel, confirming the diagnosis of Meckel’s diverticulum.
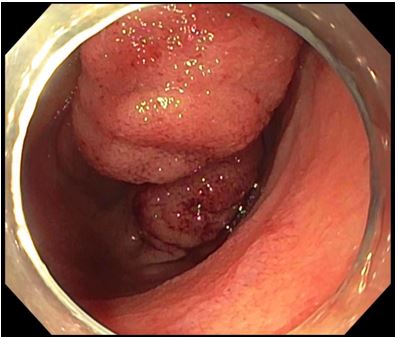
Figure 1: Retrograde single balloon enteroscopy view of inverted Meckel’s diverticulum in mid to distal ileum which appears as a submucosal mass.
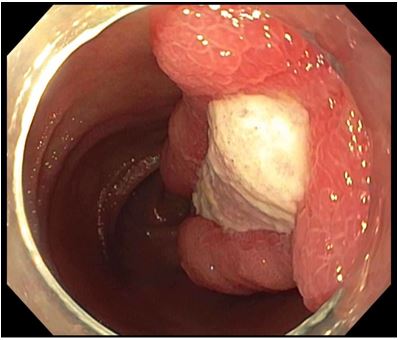
Figure 2: Retrograde single balloon enteroscopy view of ulcerated portion of the inverted Meckel’s diverticulum.

Figure 3: CT of the abdomen and pelvis with IV contrast which shows the intraluminal, blind-ending Meckel’s diverticulum in the mid to distal ileum.
Discussion
Meckel’s diverticulum results from incomplete obliteration of the vitelline duct in the developing fetus and is the most common congenital abnormality of the GI tract. The vast majority of Meckel’s diverticula remain asymptomatic and go undetected [1,2]. In a Mayo Clinic review of 1476 patients noted to have a Meckel’s diverticulum during surgery, only 16% of the Meckel’s diverticula were symptomatic. Symptomatic Meckel’s diverticula are typically discovered in childhood and have up to 3:1 male to female predominance [1,2]. In children, obstruction is the predominant presenting symptom; in adults, bleeding [2]. Bleeding from a Meckel’s diverticulum can occur with or without the presence of ectopic tissue, most commonly gastric.
Diagnosis of a symptomatic Meckel’s diverticulum can be quite difficult and requires a high level of suspicion, especially in an older adult. Capsule endoscopy can be a useful diagnostic tool in Meckel’s diverticulum [3,4]. In a case series, Krstic et al. described several features of Meckel’s diverticulum on capsule endoscopy: double lumen sign, diaphragm sign, and visible blood [3]. The positive predictive value for diagnosing Meckel’s diverticulum using capsule endoscopy in that series was 84.6% [3]. Our patient’s diverticulum lacked all of the aforementioned visual characteristics and instead appeared as an inverted, ulcerated polypoid lesion which has also been previously described [5].
When capsule endoscopy and other work-up is inconclusive, balloon-assisted enteroscopy can aid in the diagnosis due to its ability to reach deeper into the small bowel. For this purpose, balloon-assisted enteroscopy is most often performed in a retrograde fashion but depending on location of the Meckel’s can be successfully done anterograde as well. Other helpful diagnostic tests include computed tomography, small bowel series, and Tc-99m pertechnetate scintigraphy (Meckel’s scan). One caveat of the Meckel’s scan is that a negative result does not rule out a Meckel’s diverticulum. The Meckel’s scan detects ectopic gastric mucosa and, as previously alluded to, anywhere from 4.6% to 71% of symptomatic Meckel’s contain gastric tissue [1].
Surgical resection is indicated for all symptomatic Meckel’s diverticula. The most commonly employed surgical technique is segmental “T-shape” resection-anastomosis; wedge resection and tangential stapling are described as lesser-used options [6]. Resection can be performed laparoscopically, laparoscopy-assisted, or by open surgery. Surgical resection is generally well tolerated and has low rate of post-operative complications [1]. Alternatively, in at least two cases of inverted Meckel’s diverticula, endoscopic resection using double-balloon enteroscopy has been done with success [7,8]. More studies are needed to determine the safety and effectiveness of this technique.
Management of incidentally discovered, asymptomatic Meckel’s diverticula is an area of debate that is beyond the scope of this article. However, it is worth noting that the Mayo Clinic review described several patient and Meckel’s characteristics that were associated with symptomatic Meckel’s diverticula: patient age <50 years, male sex, diverticulum length >2 cm, and ectopic or abnormal features within a diverticulum [2]. Further studies are needed to determine optimal management of incidentally discovered, asymptomatic Meckel’s diverticula.
Conclusion
Patients presenting with occult or obscure GI bleeding, intestinal obstruction, or acute abdominal pain—the three most common presenting symptoms of Meckel’s diverticulum—in whom initial workup is inconclusive, it is important to keep Meckel’s diverticulum in the differential diagnosis. Correctly diagnosing Meckel’s diverticulum often requires a combination of imaging modalities, endoscopy, and even surgery. Further complicating matters, Meckel’s diverticula have the potential to invert and ulcerate, which endoscopically can be mistaken for submucosal tumor as evidenced in this case. Arriving at a correct diagnosis of symptomatic Meckel’s diverticulum is significant, as surgical resection is curative and generally well tolerated.
Authorship Criteria
Hampton Sasser performed literature review, analysis of the case, drafted the manuscript, revised the manuscript critically, and gave final approval of the version to be published.
Andrew Brock performed the balloon-assisted enteroscopy for this patient, contributed to concept and design of the case report, critically revised the report, and gave final approval of the version to be published. Andrew Brock will be designated as ‘guarantor’.
Conflicts of Interest
The authors do not have any conflicts of interest to disclose.
Grant Information
The authors received no specific funding for this work.
References
- Hansen CC, Soreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore) 2018; 97:e12154.
- Park JJ, Wolff BG, Tollefson MK, et al. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg 2005; 241: 529-533.
- Krstic SN, Martinov JB, Sokic-Milutinovic AD, et al. Capsule endoscopy is useful diagnostic tool for diagnosing Meckel's diverticulum. Eur J Gastroenterol Hepatol 2016; 28:702-707.
- Lin L, Liu K, Liu H, et al. Capsule endoscopy as a diagnostic test for Meckel's diverticulum. Scand J Gastroenterol 2019; 54:122-127.
- Fukushima M, Kawanami C, Inoue S, et al. A case series of Meckel's diverticulum: usefulness of double-balloon enteroscopy for diagnosis. BMC Gastroenterol 2014; 14:155.
- Lequet J, Menahem B, Alves A, et al. Meckel's diverticulum in the adult. J Visc Surg 2017; 154:253-259.
- Fukushima M, Suga Y, Kawanami C. Successful Endoscopic Resection of Inverted Meckel's Diverticulum by Double-Balloon Enteroscopy. Clinical Gastroenterology and Hepatology 2013; 11:e35.
- Konomatsu K, Kuwai T, Yamaguchi T, et al. Endoscopic full-thickness resection for inverted Meckel’s diverticulum using double-balloon enteroscopy. Endoscopy 2017; 49:E66-E67.

