Masseter Muscle Resection for Facial Asymmetry Correction Due To Unilateral Masseteric Hypertrophy: A Rare Case Report
Pereira Rafael1, Rodrigues Vitor C2, Santana Anna Cecília S2, Marangon JR Helvécio1, Nery Dirceu TF3, Mascarenhas Gustavo M4
1Adjunct Professor, School of Dentistry, University Center of Patos de Minas (UNIPAM), Patos de Minas, Minas Gerais, Brazil
2DDS student, School of Dentistry, University Center of Patos de Minas (UNIPAM), Patos de Minas, Minas Gerais, Brazil
3Adjunct Professor, School of Dentistry, Catholic University of Brasilia, Brasilia, Distrito Federal, Brazil
4PhD Student, São Leopoldo Mandic, Campinas, São Paulo, Brazil.
Received Date: 27/10/2020; Published Date: 08/12/2020
*Corresponding author: Rafael Martins Afonso Pereira, School of Dentistry, University Center of Patos de Minas, Av. Marabá, 831 – Alto dos Caiçaras, Zip Code: 38703-236, Patos de Minas, MG, Brazil. Telephone and fax: +55 (34) 3826-2500, E-mail: rafaelmap@unipam.edu.br
Abstract
Unilateral masseteric hypertrophy is a rare and benign anomaly, usually asymptomatic, which follows a slow and progressive growth pattern and has variable causal factors. The treatment of masseteric hypertrophy can be surgical and non-surgical, however, there is no protocol in the literature that determines which is the most suitable. A 23-year-old female patient presented with aesthetic complaints and clinical data compatible with unilateral hypertrophy of the masseter muscle. After facial analysis associated with imaging examination, it was concluded that the patient needed a unilateral masseter muscle resection surgery to decrease the lateral volume on the left side of the face by approximately 12mm. Surgical treatment was proposed using the modified PARY technique. Surgical treatment proved to be efficient, achieving satisfactory and stable results after 4 years of the surgical procedure, reducing the patient's facial asymmetry, without the need of new interventions and with no sequela.
Keywords: Facial asymmetry; Masseter muscle hypertrophy; Surgical treatment
Introduction and Case Report
The masseter is considered a powerful masticatory muscle that has a quadrangular shape. It´s origin in the zygomatic arch and its insertions in the angle and branch of the mandible and, due to its location, plays a fundamental role in facial aesthetics [1,2]. Masseteric Hypertrophy or Masseter Muscle Hypertrophy are cases in which there is a volumetric increase of this muscle, on one or both sides of the face [3,4].
Unilateral hypertrophy of the masseter muscle, which causes facial asymmetry, is an unusual, benign and generally asymptomatic clinical condition that has variable causal factors, some of which are: temporomandibular disorders, malocclusions and parafunctional habits, such as tightening, bruxism and chronic gingival chewing [1-3,5]. In some cases, masseteric hypertrophy can develop into a symptomatic condition, in which patients report myofacial pain, especially in the regions of the masseter muscle, functional impairments, such as trismus, and aesthetic changes, when facial asymmetries or changes in the shape of the face are evident [3,6,7].
Although the diagnosis of this condition is clinical, through targeted interview and muscle palpation [1], complementary exams are necessary to rule out the possibility of diseases that affect the parotid-masseteric region [1,8]. Among these exams, we highlight the panoramic and frontal postero-anterior radiographs, morphometric analysis, electromyography, ultrasonography, computed tomography and magnetic resonance. The combination of these last two techniques is considered the gold standard [7].
The treatment of masseteric hypertrophy can be surgical and non-surgical (conservative), each presenting advantages and disadvantages. However, there is no consensus or protocol in the literature that determines which is the most appropriate [6].
The purpose of this work is to report a case of unilateral hypertrophy of the masseter muscle treated surgically and followed up prospectively for 4 years, associated with a literature review of this condition.
A 23-year-old female patient was referred for evaluation, complaining of facial asymmetry. Through facial analysis associated with the imaging examination, it was concluded that the patient needed to decrease the lateral volume on the left side of the face by approximately 12mm because she had a condition compatible with unilateral hypertrophy of the masseter muscle (Figures 1-3).
Surgical treatment with slight overcorrection was proposed, removing a large amount of the deep portion of the masseter muscle associated with bone regularization, by intraoral approach, using the modified PARY technique. First, an incision was made with a scalpel in the mucosa and submucosa, approximately 5mm lateral from the mucogingival union, extending from approximately 15mm above the mandibular occlusal plane to the mesial of the first molar. Then, superficial cutting dissection maneuvers were performed until the buccinator muscle was exposed. Periosteal incision was performed, exposing the anterior border of the mandibular branch but yet periosteal detachment was not performed. Dissection toke place, starting with Metzenbaum scissors and Molt detacher, deepening and showing the masseter muscle (Figure 4). When the fascia of the lateral surface of the masseter muscle became visible, retractors were removed and a index finger dissection was initiated, separating the masseteric fascia from the aponeurotic muscular system. After lateral dissection, the medial detachment of the periosteum was carefully performed, avoiding rupture or laceration of the periosteum. The masseter muscle was then fully exposed, both medially and laterally, giving a better perception of the transverse dimension of the muscle (Figure 5). Subsequently, an electrocautery incision was performed to remove a large medial portion of the masseter muscle, according to the case planning (Figure 6). Bauer's retractors were placed at the inferior border of the mandible and in the sigmoid notch, and a Merril-Lavassier retractor is placed at the posterior board of the mandible, retracting the superficial portion of the muscle laterally. The bone spur was removed, with maxicut and reciprocating bone burs for regularization. After this stage, an active drain was inserted through the intraoral approach, transfixed to the skin in the submandibular region and fixed with sutures (Figure 7). Compressive curative with micropore and bandages were kept in place for 24 hours in order to reduce dead space, hematoma development and postoperative infection The drain was maintained for 72 hours.
Currently, the patient has a stable postoperative follow-up of 4 years, with no opening limitation, no pain and aesthetic complaints, with bilateral symmetry returned and without recurrence (Figure 8).

Figure 1: Preoperative frontal view.
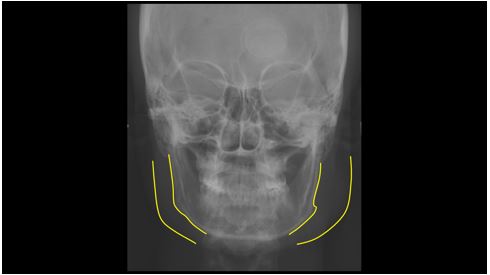
Figure 2: Frontal teleradiography with the delimitations of the masseter muscle.
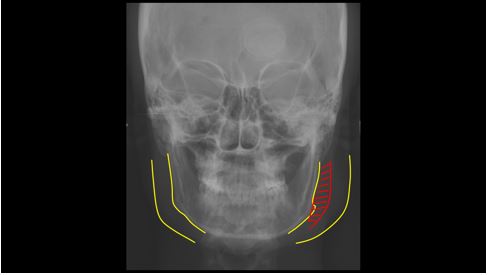
Figure 3: Frontal teleradiography with the limits of surgical correction.
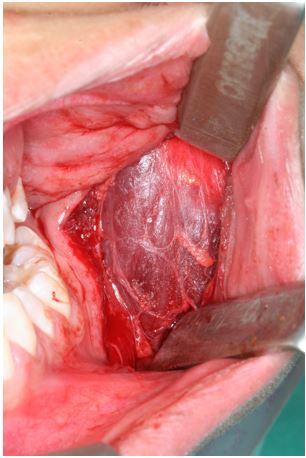
Figure 4: Exposed masseter muscle fascia.
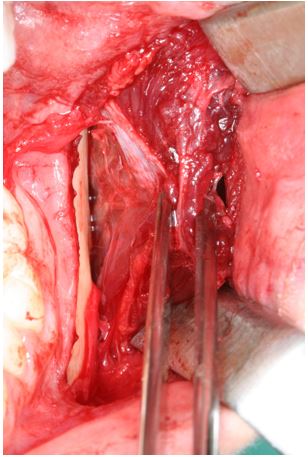
Figure 5: Total exposure of the masseter muscle.
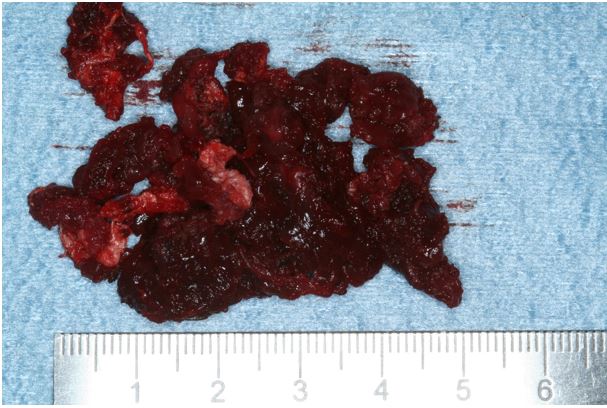
Figure 6: Deep portion removed from the masseter muscle.
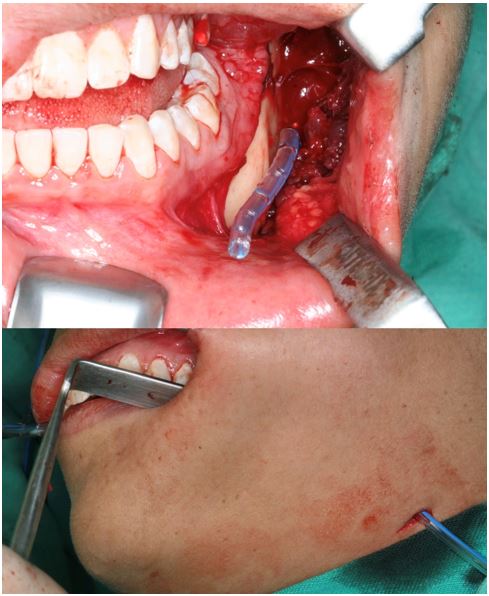
Figure 7: Insertion of the active drain.

Figure 8: Postoperative frontal view.
Discussion
Unilateral masseteric hypertrophy is a relatively rare anomaly, which follows a slow and progressive pattern of growth [2,9], affecting men and women in a 1:1 ratio, especially between the second and third decade of life [7,9,10].
This hypertrophy causes changes in the facial lines that can generate asymmetries or produce an appearance of a “square” face [2,8]. These characteristics are not well accepted aesthetically, since they cause discomfort and negative impacts for many patients [2,11]. In the present case, the patient's main complaint was aesthetics.
The diagnosis of this anomaly is made by associating the clinical examination with the results of imaging tests, especially computed tomography and magnetic resonance imaging [1]. In these exams, masseteric hypertrophy appears in a similar way, demonstrating muscle enlargement. In addition, in computed tomography, it is possible to observe, in a posteroanterior view, the presence of an abnormal lateral projection at the angle of the mandible, called bone spur [1,6]. In the present case, after the clinical examination, the strongest diagnostic hypothesis was masseteric hypertrophy. Thus, only frontal teleradiography was necessary to confirm the diagnosis, since it was possible to observe a large soft tissue asymmetry, as well as the presence of the bone spur. With the diagnosis already defined, it was not necessary to request other complementary exams, such as computed tomography and magnetic resonance imaging, considered today the gold standard of diagnosis, however, more expensive.
Masseter muscle hypertrophy has, as a differential diagnosis, diseases of the parotid glands, parotid inflammatory disease, unilateral compensatory hypertrophy, benign or malignant muscle tumors, vascular tumors, among others [1,10]. The diagnosis is more challenging when it comes to unilateral masseteric hypertrophy [10]. However, as much as in this case the hypertrophy was unilateral, there was no difficulty in closing the diagnosis, since all the characteristics, both clinical and radiographic, were compatible with masseteric hypertrophy.
There are several treatment options for the management of masseteric hypertrophy, which can be classified into surgical and non-surgical [2]. Non-surgical methods include prescription of anxiolytics, antidepressants and muscle relaxants, dental restorations and occlusal adjustments, radiofrequency and application of type A botulinum toxin. Surgical methods include mandibular angle removal, masseter neurectomy and intra reduction or extra-oral masseter muscle [7].
It is necessary to consider some factors to define the best treatment management for the patient, with the first analysis focusing on the severity of hypertrophy. Surgical intervention is capable of reducing two-thirds or more of the masseter muscle volume, while botulinum toxin, at its maximum dosage, can reduce only one-third of the muscle volume. Thus, in cases where masseteric hypertrophy is severe, the surgical option should be used [6].
Another criteria to be analyzed is related to the longevity and predictability of the treatment [6]. It is well known that the injection of botulinum toxin type A is a safe procedure that produces good results for the treatment of mesenteric hypertrophy [3,12,13], however it has many adverse effects such as edema, bruising, dizziness, headache, weakness in chewing, asymmetry, xerostomia, among others [3,4,14]. In addition to these factors, another limitation of the use of this technique is its temporary pharmacological effects, which require several reapplications due to an approximate duration of six months [2,3,15]. On the other hand, the surgical option is capable of providing a more predictable and definitive treatment [6], even with the possible complications, such as postoperative hemorrhage, edema, hematoma, facial asymmetry and damage to noble structures. Taking into account the severity of hypertrophy, predictability and, consequently, the effectiveness of the treatment, we opted for the surgical procedure using the modified PARY technique, already described.
The traditional treatment for hypertrophy of the masseter muscle involves its partial surgical resection, associated or not with mandibular angles, which can be performed intra or extra-oral [3]. In the past, the headgear technique was better accepted and indicated, since it offered a better visualization of the operative field. However, with the evolution of surgical materials, as well as the development of new techniques, the procedure through the intraoral route has become a good option [2]. In this case, we opted to perform partial resection of the masseter muscle by intraoral route, since we wanted to minimize the risks of facial nerve damage, as well as avoid noticeable scarring in the patient, whose main complaint was aesthetics.
In the present study, surgical treatment proved to be efficient, achieving satisfactory and stable results after 4 years of the surgical procedure, reducing the patient's facial asymmetry, without the need for new interventions and with no sequela and recurrence.
Description of Each Author's Contribution to the Manuscript
- Rafael Martins Afonso Pereira: involved in patient assistance, clinical documentation, performing the surgical procedure, literature review and drafting the manuscript;
- Vitor Carvalho Rodrigues: literature review and drafting the manuscript;
- Anna Cecília Silva Santana: literature review and drafting the manuscript;
- Helvécio Marangon Júnior: involved in literature review, diagnosis and drafting the manuscript;
- Dirceu Tavares Formiga Nery: involved in performing the surgical procedure;
- Gustavo Mota Mascarenhas: involved in patient assistance, performing the surgical procedure, literature review and drafting the manuscript.
Conflicts of Interest/Competing Interests
The authors have no conflicts of interest to declare.
Grant Information
The authors received no specific funding for this work.
References
-
- Kebede Biruktawit, Megersa Shimalis. Idiopathic masseter muscle hypertrophy. Ethiopian Journal of health sciences, 2011; 21(3).
- Singh Sourav, et al. Surgical management of masseteric hypertrophy and mandibular retrognathism. National journal of maxillofacial surgery, 2011; 2(1): p. 96.
- Graziano P, et al. Bilateral hypertrophy of masseteric and temporalis muscles, our fifteen patients and review of literature. Eur Rev Med Pharmacol Sci, 2016; 20(1): p. 7-11.
- Yeh Yu‐Ting, Peng Jui‐Hui, Peng Hsien‐Li Peter. Literature review of the adverse events associated with botulinum toxin injection for the masseter muscle hypertrophy. Journal of cosmetic dermatology, 2018; 17(5): p. 675-687.
- Prabhu Rohan, Mandel Louis. Simultaneous bilateral hypertrophies of the parotid gland and masseter muscle: Case Report. Journal of Oral and Maxillofacial Surgery, 2017; 75(1): p. 149-152.
- Pary Augusto, Pary Katyuscia. Masseteric hypertrophy: considerations regarding treatment planning decisions and introduction of a novel surgical technique. Journal of oral and maxillofacial surgery, 2011; 69(3): p. 944-949.
- Fedorowicz Zbys, Van Zuuren Esther J, Schoones Jan. Botulinum toxin for masseter hypertrophy. Cochrane Database of Systematic Reviews, 2013; n. 9.
- Guruprasad R, et al. Masseter and medial pterygoid muscle hypertrophy. Case Reports, 2011; 2011: p. bcr0720114557.
- Parente Eduardo Varela, et al. Surgical treatment of bilateral temporalis and masseteric hypertrophy: Report of a case. Open Journal of Stomatology, 2013; 3(1): p. 99.
- Sannomya Eduardo Kazuo, Gonçalves Marcelo, Cavalcanti Marcelo Paraíso. Masseter muscle hypertrophy: case report. Brazilian dental journal, 2006; 17(4): p. 347-350.
- Hirohi Toshitsugu, Yoshimura Kotaro. Lower face reduction with full-thickness marginal ostectomy of mandibular corpus-angle followed by corticectomy. Journal of plastic, reconstructive & aesthetic surgery, 2010; 63(8): p. 1251-1259.
- Choe Seong Wook, et al. Effects of botulinum toxin type a on contouring of the lower face. Dermatologic surgery, 2005; 31(5): p. 502-508.
- Bas Burcu, et al. Treatment of masseteric hypertrophy with botulinum toxin: a report of two cases. Oral Patol. Oral Y Cirugía Bucal, 2010; 15: p. e649-e652.
- KIM, Jae-Hong et al. Effects of two different units of botulinum toxin type a evaluated by computed tomography and electromyographic measurements of human masseter muscle. Plastic and reconstructive surgery, 2007; 119(2), p. 711-717.
- Ham Jong-Wook. Masseter muscle reduction procedure with radiofrequency coagulation. Journal of oral and maxillofacial surgery, 2009; 67(2), p. 457-463.

