Eosinophilic Cholecystitis, A Rare Case Report With a Review of the Literature
Nasim M and Mohammadzadeh S*
Department of Pathology, Shiraz University of Medical Sciences, Iran
Received Date: 10/09/2020; Published Date: 20/11/2020
*Corresponding author:
Sahand Mohammadzadeh, Department of Pathology, Shiraz University of Medical Sciences, Iran Fax: 071323017; Tel: 09173078147; E-mail: mohammads@sums.ac.ir; Orcid:0000-0001-6974-1323
Abstract
The clinical presentation of eosinophilic cholecystitis (EC) is the same as typical cholecystitis. The right upper quadrant (RUQ) tenderness and Murphy’s sign are common symptoms. In literature, some cases reported that have been associated with the hyper-eosinophilic syndrome(HES), infections, drugs, and parasitosis, but the etiology is often unknown. We report a 32-year-old woman presented with two days of RUQ pain with radiation to the right shoulder. A clinical picture of severe acute cholecystitis was recorded. The patient underwent open cholecystectomy. Microscopically, an edematous wall with occasional acute and chronic inflammatory cells and predominantly eosinophils were observed. Because the signs of EC are the same as typical cholecystitis, it should not be considered a separate entity. The importance of the diagnosis of EC is that it can be associated with other diseases that should be considered when it is diagnosed.
Keywords: Eosinophilic Cholecystitis; Gallbladder Disease; Cholecystectomy
Introduction
The clinical symptoms of Eosinophilic cholecystitis (EC) are the same as typical cholecystitis. It presents with right upper quadrant (RUQ) tenderness. Some cases have been associated with the hyper-eosinophilic syndrome(HES), parasitosis, infections, drugs, but in most cases, the etiology is not well known [1-3]. It represents 0.25 up to 6.4% of all cholecystitis [4].
EC is clinically indistinguishable from other causes of cholecystitis. However, peripheral eosinophilia is sometimes seen, as in parasitic disease and HES [3]. In the microscopic examination, massive transmural infiltration of eosinophils that make up 90% or more of the inflammatory infiltration is the main histologic characteristic [5]. Usually, EC is acalculous, but calculi are found in 30% of cases [6]. When its involvement is limited to the gall bladder, the best treatment is cholecystectomy, and the prognosis is usually good [7]. We report a case of EC in a woman who presented with RUQ tenderness.
Case Presentation
A 32-year-old woman presented with RUQ pain with radiation to the right shoulder since two days before admission. Then presented with nausea and temperature of 37 °C for the past two days. The patient had no past personal or family history. Her investigations indicated hemoglobin 12.1 g/dl, total leukocyte count 8.4×103/ mm3, neutrophils 55%, lymphocyte 35%, eosinophils 7%, monocytes 2%, band 1% and platelets 313×103/ul/mm3. Ultrasound showed a semi distended gall bladder with no stone. A clinical picture of severe acute cholecystitis was recorded. The patient underwent open cholecystectomy. On gross examination, the gall bladder was 80mm in length, with a 30mm average diameter. The average wall, the thickness was 3mm, with a rubbery grayish-green cut section (Figure 1). Microscopically, an edematous wall with occasional acute and chronic inflammatory cells were seen with predominantly eosinophils that make up 90% or more of the inflammatory infiltration (Figure 2). A diagnosis of acute EC was reported. Drug history and past medical history of patients were negative. Cholecystectomy led to full recovery, and the patient was discharged without any complications. Due to peripheral eosinophilia, we recommended evaluating the patient for the hyper-eosinophilic syndrome, eosinophilic gastroenteritis, and parasitosis.
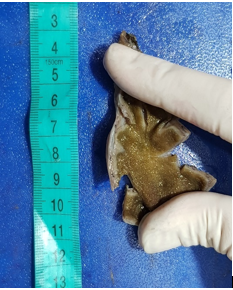
Figure 1: Gross picture photo showingrubbery grayish-green wall withirregular mucosalsurface.
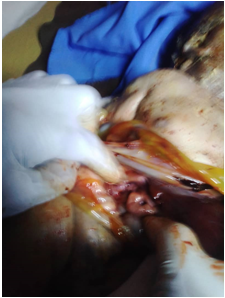
Figure 2:Inflammatory transmuralinfiltrate, predominantly eosinophilic, in the gallbladder wall. (H&E stain). 2A: 200x magnification; 2B: 400x magnification
Discussion
In most cases of acute cholecystitis, gallstone impaction starts the inflammatory process. The bile accumulates in the gall bladder and causes chemical irritation, and may facilitate bacterial invasion [7,11].
Few case reports and case series are available in the literature about EC. The prevalence of EC ranges from 0.25 to 6.4%, as reported in multiple studies [1,3,4]. Although few case reports are describing EC, the etiopathogenesis is still not well known [5]. In a series by Fox et al. (12,13), 625 gallbladders were evaluated, in which 16 of them exhibited eosinophilic infiltration. In the series published by Dabbs et al. [5], 217 gallbladders were assessed over two years, and in 14 (6.5%) of the EC were observed. A study reported by Muhlberger et al. [14] 55 of 660 resected gallbladders (8.3%) had ≥25% eosinophilic infiltration.
A search in the literature revealed 27 individuals with acute cholecystitis accounts of EC since 1949. The majority of them have associated with HES and eosinophilic cholangiopathy, parasitic infestation, or acalculous cholecystitis [3,4,8,10,11]. When peripheral eosinophilia is observed, the diagnosis of HES should be considered [2].
Acalculous cholecystitis is another cause of eosinophilic cholecystitis, with the invasion of the mucosal surface by eosinophils [15]. Causes of acute acalculous cholecystitis are different, including critical illness, major burns, herbal medicine [16,17]. Patients with acalculous cholecystitis are three to four times more likely to have EC than patients with gall stone.
If no etiology was found, the case is considered one of idiopathic EC. Idiopathic cholecystitis is crucial because laboratory tests can not diagnose it. By considering peripheral eosinophilia, one must think of the number of etiologies that may cause such disease.
Abdominal Ultrasound results may be unremarkable or show signs suggestive of typical cholecystitis such as gallbladder distension, wall thickening, or sonographic Murphy sign [10].
In our patient peripheral eosinophilia, about 7% was noted during the hospital course. The etiology for eosinophilia was unknown. Cholecystectomy led to full recovery, and the patient was discharged without any complications. Due to peripheral eosinophilia, we recommended evaluating the patient for the hyper-eosinophilic syndrome, eosinophilic gastroenteritis, and parasitosis.
Because EC can happen may occur in many conditions, and it can be associated with other diseases; therefore, when it is diagnosed, possible associated etiologies should be investigated. Pathologists should carefully differentiate EC from other causes of cholecystitis, which may have a worse prognosis than the cholecystitis itself [18-21].
EC prognosis is good [22]. When the disease is limited to the gall bladder, the treatment of choice is cholecystectomy, preferably performed laparoscopically [23,24].
Conflict of Interests
Fryns syndrome is a rare autosomal recessive disorder with a high rate of stillbirth and early neonatal mortality. Diagnosis of FS can be made prenatally through maternal ultrasound scan.Rare associations such as omphalocele and undescended testes can be found in FS.
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
The research has been carried out by the World Medical Association Declaration of Helsinki.The study approved by the EthicsCommittee of Shiraz University of medical science.
Funding/Support: Personal support of authors. No institutional funding.
Patient Consent
Informed consent was obtained from the patient.
Data Availability
The data used to support the findings of this study are included in the article. Previously reported data were used to support this study and are available at DOI: 10.1016/j.cireng.2013.10.040and DOI: 10.4103/AZMJ.AZMJ_82_19.
References:
- Albot G, Poilleux, Olivier C, Libaude H, Cascarigny P. Les cholecystites a eosinophils. Presse Med 1949;39: 558-559,
- Felman RH, Sutherland DB, Conklin JL, Mitros FA. Eosinophilic cholecystitis, appendiceal inflammation,pericarditis, and cephalosporin-associated eosinophilia. Digest Dis Sci 1994;39:418-422.
- Tenner S, Roston A, Lichtenstein D, Brooks D, Herlihy E, Carr-Locke D. Eosinophilic cholangiopathy. GastrointestEndosc1997;45:307-309.
- Al-Abdulla NA, Schulick RD, Regan F. Hypereosinophilic sclerosing cholangitis: findings using half- Fourier magnetic resonance imaging. Hepatogastroenterology2000;47:359-361.
- Hepburn A, Coady A, Livingstone J, Pandit N. Eosinophilic cholecystitis as a possible late manifestation of the eosinophilia-myalgia syndrome. Clinical Rheumatology 2000;19:470-472.
- Tajima K, Katagiri T. Deposits of eosinophil granule proteins in eosinophilic cholecystitis and eosinophilic colitis associated with hypereosinophilic syndrome. Digest Dis Sci 1996;41:282-288.
- Butler TW, Feintuch TA, Caine WP. Eosinophilic cholangitis, lymphadenopathy, and peripheral eosinophilia: a case report. Am J Gastroenterol 1985;80:572- 574.
- Fox H, Mainwaring AR. Eosinophilic infiltration of the gallbladder. Gastroenterology 1972;63:1049-1052.
- Kim YH. Eosinophilic cholecystitis in association with Clonorchis sinensis infestation in the common bile duct. Clin Radiol1999;54:552-554.
- Russel COH, Dowling JP, Marshall RD. Acute eosinophilic cholecystitis in association with hepatic echinococcosis. Gastroenterology 1979;77:758-760.
- Dabbs DJ. Eosinophilic and lymphoeosinophilic cholecystitis. Am J SurgPathol1993;17:497-501.
- Rosengart TK, Rotterdam H, Ranson JHC. Eosinophilic cholangitis: a self-limited cause of extrahepatic biliary obstruction. Am J Gastroenterol 1990;85:582-585.
- Adusumilli PS, Lee B, Parekh K, Farrelly P. Acalculous eosinophilic cholecystitis from herbal medicine: a review of adverse effects of herbal medicine in surgical patients. Surgery 2002;131:352-356.
- Muhlberger VF. ZurMorphologie der eosinophilen cholecystitis und die frageihrerallergischengenese. Int Arch Allergy 1954;5:434-448.
- Hellstrom HR. Eosinophilic and lymphoeosinophilic cholecystitis. Am J SurgPathol 1994:18:215.
- Kerstein MD, Sheahan DG, Gudjonsson LJ. Eosinophilic cholecystitis. Am J Gastroenterol 1976; 66:349-352.
- Leegaard M. Eosinophilic cholecystitis. Acta ChirScand1980;146:295-296.
- Steffen RM, Wyllie R, Petras RE, Caulfield ME, Michener WM, Firor HV, Norris DG. The spectrum of eosinophilic gastroenteritis: report of six pediatric cases and review of the literature. Clin Pediat1991;30:404- 411.
- Rodriguez HE, Djoham RS, Cahill WJ, Connolly MM, Podbielski FJ. Laparoendoscopic diagnosis of eosinophilic enteritis. JSLS 1998;2:181-184.
- Stringel G, Mercer S, Sharpe D, Shipman R, Jimenenez C. Eosinophilic gastroenteritis. Canad J Surg 1984;27: 182-183.
- Parry SW, Pelias ME, Browder W. Acalculous hypersensitivity cholecystitis: hypothesis of a new clinicopathologic entity. Surgery 1988;911-916.
- Shakov R, Simoni G, Villacin A, Baddoura W. Eosinophilic cholecystitis, with a review of the literature. Ann Clin Lab Sc 2007;37:182-5.
- Punia RP, Arya S, Jain P, Bal A, Mohan H. Eosinophilic and lymphoeosinophilic cholecystitis. Indian J Gastroenterol 2003;22:153-4.
- Patel NB, Oto A, Thomas S. Multidetector CT of emergent biliary pathologic conditions. Radiographics2013;33:1867-88.

