Free Strand of the Greater Omentum in Surgical Practice and its Morphological Characteristics
Martynov Vladimir L, Kolchin Dmitry G, Vadim Alexandrovich K* and Vadim Aleksandrovich T
1Doctor of Medical Sciences, Associate Professor, National Research Nizhny Novgorod State University, N.I. Lobachevsky (UNN), Russia
2Department of Surgery; GBUZ GKB No. 12, Nizhny Novgorod, Russia
3Candidate of Medical Sciences, Deputy Chief Physician for Surgery, GBUZ GKB No. 12, Nizhny Novgorod, Russia
Received Date: 03/09/2020; Published Date: 19/11/2020
*Corresponding author:Martynov VL, GBUZ NO, City Clinical Hospital No-12, Sormovsky District of Nizhny Novgorod, Russia, 603033, Tel: 89049188600; E-mail: hirurgia12@mail.ru
Abstract
In his operating work, the surgeon often uses the patient's tissue to solve practical problems. For our work, the data of Liebermann-Meffert D. and White H. (1989) on the greater omentum are of interest [1]. Research shows that the "policeman of the abdominal cavity" - the great omentum in pathological conditions, acquires very special properties: plasticity; the ability to adhere to an injured and inflamed surface; the ability to hemostasis; the ability for ingrowth and revascularization; the ability to absorb liquids and microparticles from the abdominal cavity; the ability to phagocytosis and immunological response. Adhesions with the omentum are formed much faster than with other organs of the abdominal cavity. Even the freely transplanted omentum tissue without blood supply retains these properties. After 21 days, the omentum tissue is completely fused with the recipient [2].
Introduction
Experimental studies of ingrowth of the omentum graft and its vessels are very indicative. Sections of the omentum of different thickness and size were separated from its bulk and fixed without revascularization to various organs and tissues of the same or another animal: stomach, small and large intestine, liver, spleen, kidney, urinary bladder, lung, pleura, peritoneum, mesentery, aorta, inferior vena cava. Within a week, the graft is firmly attached to the tissues of the recipient organs, its separation is difficult, due to a decrease in the amount of fat, its thickness is reduced, necrobiotic processes, necrosis zones are reduced. After three weeks, the graft cannot be separated, when an attempt is made, bleeding occurs, the amount of fat decreases and is replaced by dense fibro- and angioplastic tissues so that its surface resembles the surface of the recipient tissue. After 12 weeks, it is difficult to distinguish the omentum tissue from the recipient tissue; the suture line serves as a reference point. The engraftment of free grafts did not depend on their size, but necrosis zones are more often formed in thick grafts. The graft remains viable when frozen for two weeks or even longer. Stages of omentum transplant engraftment: attachment - up to 4 hours, beginning of vascular ingrowth - 24 hours, tight fit - 48 hours, revascularization - 3 days, fat resorption - 3 weeks, fibrous degeneration - 24 weeks [1].
These studies allowed us to use a strand of the free area of the greater omentum in the small intestine in 107 patients. Here is an example of the clinical use and preservation of the viability of the free strand of the greater omentum.
Case Report
A 25 years old, was admitted to the GBUZ NO "GKB No. 12" in Nizhny Novgorod on 11.11.2013 with a diagnosis of "Closed abdominal trauma". After dynamic observation, an emergency laparotomy was performed, during which a rupture of the pancreatic head was detected. Outflow of bile, pancreatic juice was not detected. A tampon was brought to the site of damage to the gland through a separate incision in the right lumbar region. The drains were placed in the right lateral canal, in the omental bursa, in the small pelvis. On 20.11.2013, the intake of contents up to 3 liters with an admixture of bile was noted. On an urgent basis, relaparotomy was performed, during which two perforations were revealed on the posterior wall of the vertical part of the 12-PC, each with a diameter of up to 7 mm, from which, after the introduction of methylene blue, a blue discharge began to flow into the stomach. After excision of the edges of the perforations, the latter are sutured with interrupted single-row sutures. The seam line is reinforced with a large gland strand. A drainage-foam rubber system for active aspiration is connected to this zone through the opening of the right lumbar region (the place of the gauze pad). A loop of the jejunum was isolated 30 cm from the Treitz ligament, on which an areflux nutritional jejunostoma was formed with an interintestinal anastomosis according to Brown and a "plug" on the leading loop 1 cm below the anastomosis. The stoma was placed in the left mesogastric region. A feeding tube was inserted 25 cm behind the anastomosis line.
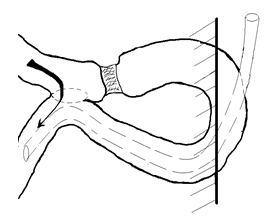
Figure 1: Scheme of the formation of a "plug" to create an areflux nutritional jejunostoma according to the developed method.
On January 20, 2014, the patient was admitted to the Nizhny Novgorod City Clinical Hospital No. 12 for the second stage of treatment - closing the nutritional jejunostomy. The skin around the stoma is intact. Performed fistuloenterography through a probe introduced into the leading section of the stoma to the "plug". The contrast does not pass through the "plug" zone, which confirms its areflux function.
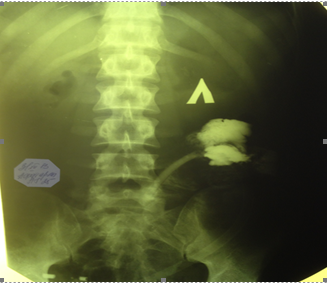
Figure 2: Fistuloenterography - the contrast does not pass through the "plug" formation zone.
01/23/2014 under general anesthesia in the left mesogastric region with two bordering incisions around the stoma, the latter was isolated from the tissues of the anterior abdominal wall. The segment of the intestine with the stoma is brought out to the anterior abdominal wall. The area of the free omentum with the ligature, which acts as a "plug", is viable, loosely welded to the jejunum. The interintestinal anastomosis is passable. Near the anastomosis, the sections of the intestine were stitched with the UO apparatus. The section of the intestine bearing the stoma was resected. The intestinal stumps were additionally sutured with two semi-lace sutures each. Layered suture of the wound of the anterior abdominal wall. Preparation: a section of the jejunum up to 10 cm long with a stoma and a free section of the greater omentum - “plugs”. The area of the free omentum with a ligature, which acts as a "plug", was loosely welded to the jejunum (Fig. 3). The mucous membrane of the jejunum of the "plug" formation zone is not visually changed (Fig. 4). The interintestinal anastomosis is passable.
Morphological examination of the "plug" zone at 3, 6, 9, 12 hours of the intestinal wall circumference showed only edema, moderate lymphohistiocytic infiltration, moderate circulatory disorders [3].
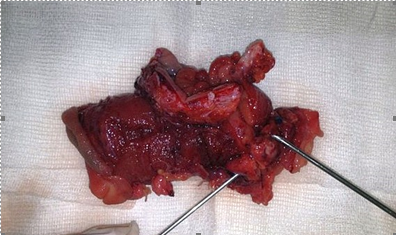
Figure 3: The macro specimen shows the design of the "plug" from a viable free section of the greater omentum.
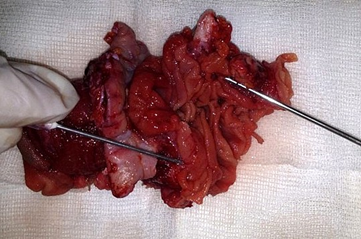
Figure 4: The mucous membrane of the jejunum of the "plug" formation zone is not visually changed.
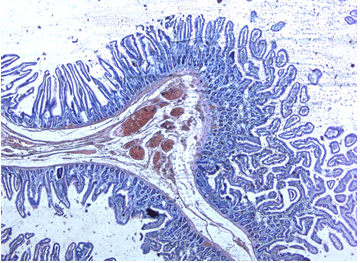
Figure 5: Fragment of the intestinal mucosa in the "plug" zone. In the submucosa - pronounced plethora of blood vessels, moderate round-cell infiltration. Hematoxylin-eosin staining. Uv. X 200.
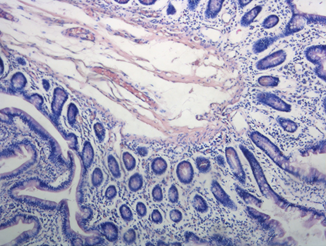
Figure 6: A fragment of the intestinal mucosa in the "plug" zone. Edema, moderate lymphohistiocytic infiltration, moderate circulatory disorders. Hematoxylin-eosin staining. Uv. X 400.
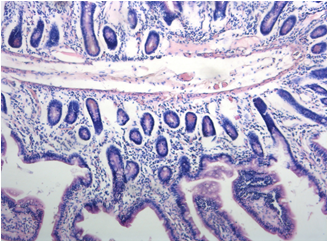
Figure 7: Fragment of the intestinal mucosa in the "plug" zone. Edema, moderate lymphohistiocytic infiltration, moderate circulatory disorders. Hematoxylin-eosin staining. Uv. X 400.
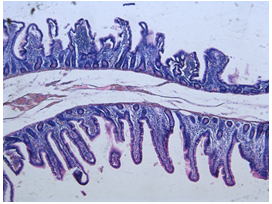
Figure 8: Fragment of the intestinal mucosa in the "plug" zone. Dystrophic changes in the mucous membrane, edema, moderate lymphohistiocytic infiltration, moderate circulatory disorders. Hematoxylin-eosin staining. Uv. X 400.
The wound healed by primary intention. In satisfactory condition 02/03/2013 was discharged for outpatient observation by a surgeon.
Conclusion
Thus, our observation confirms the possibility of using a strand of "free", devascularized omentum as a plastic material in small bowel surgery.
References:
- Liebermann-Meffert, D, White, H. Big gland, D. Liebermann-Meffert, H. White M . Medicine. 1989;336 p.
- Loewy R. Methode des greffes peritoneales / R Lo, S. S. Relationship between age and clinical characteristics of patients with gastric cancer / S. S. Lo, C. W. Wu, M. C. Hsieh. J. Gastroenterol Hepatol. 1996;11(6):511-514.
- Thompson, S. A. The use of free omental grafts in the thorax. An experimental study. Am. J. Surg. 1945;70:227-231.

