A Modified Supine Positioning Setup for Diabetic Foot Reconstruction with Peroneal Artery Perforator Based Propeller Flap: Technique Tips and Tricks
Xiangxia L*
Division of Plastic Surgery, First Affiliated Hospital, Sun Yat-sen University, China
Received Date: 19/08/2020; Published Date: 19/11/2020
*Corresponding author:Xiangxia Liu, Division of Plastic Surgery, First Affiliated Hospital, Sun Yat-sen University, 58# Zhongshan Road II Guangzhou, 510080, China. E-mail: liuxsha@mail.sysu.edu.cn
Abstract
Most posterior hind-foot and ankle surgery is traditionally setup in a prone position for better access during the surgery. When using the peroneal artery perforator based propeller flap to reconstruct the complex wound of a diabetic foot, the best approach to dissect the perforator vessels is from anterior aspect when the patient lays on supine with leg rotated internally, obviously this position put a lot of stress on the surgeons to get the access of the heel, vice versa. Furthermore, in some cases the co-morbidity of the patient may limit the patient from lying on prone for a long hour surgery under general anesthesia for safety reasons. In this article we present a 54 years old male complex wound case of diabetic foot with skin necrosis in heel and medial ankle area (Figure 1), which was reconstructed with peroneal artery perforator based propeller flap. The purpose of this paper is to describe in detail of an innovative and modified supine positioning during the surgery, which facilitated both the harvest of flap and reconstruction of the heel and ankle procedure.
Keywords: Surgical Positioning; Diabetic Foot; Propeller Flap; Reconstruction; Level of Evidence: Level V; Expert Opinion.
Figure 1: A 54 years old male with diabetic foot on the left side.

Figure 1a: Initial presentation.

Figure 1b: Medial aspect of the defect after debridement, showing posterior tibial tendon exposure.

Figure 1c: Posterior aspect of the defect after debridement, showing Achilles tendon and bone exposure.
Techniques
The patient is placed in traditional supine position and bilateral upper extremities are tugged on the sides of the body with intravenous access on the right hand contralateral to the left foot to be operated on. All the potential pressure points are protected. The whole left lower extremity is prepped and draped. A sterile pneumatic thigh tourniquet is applied. A self-invented C shaped abdominal retractor (Figure 2), which is widely used in abdominal surgery, is applied with the curve pointing caudally (Figure 3a). The left lower extremity can be placed on the surgical table while the surgeons are dissecting the perforator vessels or placed on the bar of C shaped abdominal retractor with appropriate padding while the surgeons need to access the heel and posterior aspect of the lower leg to harvest and inset the flap (Figure 3b and c). After the flap is harvest, the tourniquet is released and the split-thickness skin graft is harvested from the upper thigh by Zimmer® dermatome. With the support of retractor, surgeons are able to change the lower leg position easily and maintain the position to get access of the heel and posterior aspect of lower leg. The defects are successfully covered by the propeller flap based on a single perforator of peroneal vessels (Figure 4).
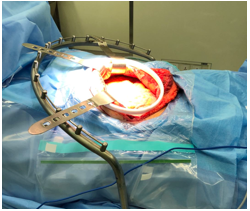
Figure 2: The setup of C shape retractor during the abdominal surgery on lateral view.
Figure 3: The setup of C shape retractor during the heel reconstruction surgery.

Figure 3a: Initial setup of C shape retractor with lower extremity on the table.


Figure 3b and 3c: The lateral and bottom view when the lower extremity is placed on the C bar with cushion underneath.
Discussion
It is estimated that 12 percent of diabetic patients could develop foot ulceration during their lifetime.5For complex wounds with bone and/or tendon exposure in patients with multiple co-morbidities, the selection of reconstructive options was limited. More and more studies supported the peroneal/posterior tibial/anterior tibial artery perforator based flaps as a powerful tool in diabetic patients with compromised lower leg circulation.3,4Appropriate surgical position is crucial for both the safety of the patients and the efficiency of the procedure.1,2,8,9,11The best position for posterior hind-foot and ankle procedure is prone.12While in diabetic foot reconstruction, there are a significantly large percentage of patient having multiple co-morbidity diseases, by putting them on prone position for a long hour’s surgery may jeopardize the patients’ safety.6The anterior approach is a safe and fast track to dissect the peroneal artery perforator vessels, which means the patient would lay on supine position with lower leg internally rotated. Unfortunately, a traditional supine position is a nightmare for the posterior hind-foot and ankle procedures because surgeons may only have limited access to the surgical field, oftentimes the lower extremity must be raised and held consistently by an assistant. In some scenario this position dilemma may be solved by lateral decubitus position, but it is inapplicable in our patient because he had a wound on the medial malleolus area needs to be covered at the same time. Lower leg Mayo stand pad may help the surgeons to access the heel and ankle, and keep the anterior approach for the perforator vessels dissection, while there is no access for flap harvest and skin grafting.7,10 Our circulation nurses come up with an innovative idea of using the abdominal retractor to support the lower leg while keeping the supine position (Figure 3).

Figure 4: The postoperative picture of medial aspect and posterior aspect of the foot.
This abdominal retractor was invented by Dr. Liang Lijian from the Division of Hepatic Surgery in our hospital and widely applied in abdominal surgery (Figure 2). With the support by the retractor’s C shape bar, we are able to access both anterior and posterior of the lower leg. Also it is convenient to switch the position during the surgery and there is minimal impact on the skin harvesting procedure on the thigh. This position could be one of the best solutions for our patient who could not tolerate general anesthesia and prone position. Furthermore we are thinking of making a customized supportive device to accomplish the idea and provide more convenient surgical position for this type of procedure. With the possible help for the device, surgeons will be able to place the patient in supine position and perform the posterior hind-foot and ankle procedure without any struggle.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest in respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References:
- Agostini J, Goasguen N, Mosnier H. Patient positioning in laparoscopic surgery: tricks and tips. J Visc Surg. 2010;147(4):e227-232.
- Boszczyk A, Kordasiewicz B, Kicinski M, Fudalej M, Rammelt S. Operative Setup to Improve Sagittal Syndesmotic Reduction: Technical Tip. J Orthop Trauma. 2019;33(1):e27-e30.
- Demiri E, Tsimponis A, Pavlidis L, Spyropoulou GA, Foroglou P, Dionyssiou D. Reverse neurocutaneous vs propeller perforator flaps in diabetic foot reconstruction. Injury. 2020.
- Dhua S, Manashree S, Tilak BG. The Clinical Outcome of Perforator Based Sural Artery and Propeller Flaps in Reconstruction of Soft Tissue of Extremities. World J Plast Surg. 2019;8(1):3-11.
- Ducic I, Attinger CE. Foot and ankle reconstruction: pedicled muscle flaps versus free flaps and the role of diabetes. Plast Reconstr Surg. 2011;128(1):173-180.
- Gougoulias N, Dawe EJ, Sakellariou A. The recovery position for posterior surgery of the ankle and hindfoot. Bone Joint J. 2013;95-B(10):1317-1319.
- Hampton CB, Shawen SB, Keeling JJ. Positioning technique for combined anterior, lateral, and posterior ankle and hindfoot procedures: technique tip. Foot Ankle Int. 2010;31(4):348-350.
- Harada Y, Tanaka JI, Umemoto T, et al. Toward standardized patient positioning to avoid peripheral nerve injury during laparoscopic colorectal surgery: Application of a protocol and study of the resulting relationship between total rotation time and contact pressure at the shoulder. Asian J Endosc Surg. 2019;12(3):269-274.
- Liu X, Wang X, Meng X, Wang H, An Z. Effects of patient position on lower extremity venous pressure during different types of hysterectomy. J Obstet Gynaecol Res. 2015;41(1):114-119.
- Soden PA, Zettervall SL, Ultee KH, et al. Dual antiplatelet therapy is associated with prolonged survival after lower extremity revascularization. J Vasc Surg. 2016;64(6):1633-1644e1631.
- Sukhu T, Krupski TL. Patient positioning and prevention of injuries in patients undergoing laparoscopic and robot-assisted urologic procedures. Curr Urol Rep. 2014;15(4):398.
- Williams JM, Bebbington A. The modified recovery position for posterior leg surgery. Ann R Coll Surg Engl. 2011;93(7):556.

