Rosai Dorfman Disease: Bull Neck Versusmoon Facies: A balancing Act? A Diagnostic and Therapeutic Dilemma
Kaushal D*, Verma AK, Sharma V, Elhence P and Kumar P
1Associate Professor, Department of Otorhinolaryngology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
2Senior Resident, Department of Otorhinolaryngology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
3Professor, Department of Pathology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
4Department of Paediatrics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
Received Date: 18/10/2020; Published Date: 18/11/2020
*Corresponding author:Darwin Kaushal, Associate Professor, Department of Otorhinolaryngology, All India Institute of Medical Sciences, Jodhpur 342005, Rajasthan (India). Tel: +91-8003647999; Email:drdarwin.aiims@gmail.com
Abstract
Rosai Dorfman Disease is a rare non-neoplastic disorder of unknown etiology presenting with painless massive cervical lymphadenopathy and/or extranodal involvement with a benign course. The challenge lies in diagnosis and deciding the best course of treatment as standard treatment guidelines are currently lacking.Oral steroid therapy, chemotherapy and radiotherapy have been advocated as therapeutic options with limited supporting evidence, each with their potential adverse effects. We present the case of a young male child with bilateral massive cervical lymphadenopathy who we diagnosed as RDD and treated with oral steroids. The challengein our case wasreaching a diagnosis and adjusting the dosage and duration of oral steroid therapyas evidence for appropriate titration of therapy is still lacking. He suffered from adverse effects of prolonged steroid therapy, requiring repeated change in course of management. Currently, he is on close follow-up with reversal of side effects and complete resolution of symptoms.
Keywords: Rosai Dorfman Disease; Massive Cervical Lymphadenopathy; Bull Neck, Moon Facies; Sinus Histiocytosis
Introduction
Sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease (RDD) was described first by Rosai and Dorfman in 1969. It is a rare and non-neoplastic histiocytic proliferative disorder ofunknown etiology, with a childhood predilection [1]. Although it resembles malignant disorders in appearance,its clinical course is predominantly benign albeit unpredictable.1Bilateral painless cervical lymphadenopathyis the most common presentation though extra-nodalmanifestations are also reported. The diagnosis is difficult due to nonspecific pathological findings and requires a high index of suspicion. A variable response to steroids and chemotherapeutic drugs has been described in literature however clear guidelines for optimum treatment are lacking [2,3]. We present a case report of a two years old child diagnosed with RDD, treated with long term oral steroid therapy. Dose adjustment posed a unique challenge as the child developed significant side effects of treatment. However, with prolonged and controlled oral steroid therapy, we could achieve complete resolution of symptoms and regression of side effects.
Case Report
A two yearsold boy was brought to our outpatient services (Otorhinolaryngology department) with the complaint of multiple bilateral neck swellings for last 6 months which were painlessand progressively increasing in size. There was no history of weight loss, fever and difficulty in swallowing or breathing or nasal complaints. On examination, there were multiple, mobile,discrete, non-tender bilateral lymph nodes at level II, III, IV and V, the largest measuring 4x3 cm.

Figure 1: Clinical image of the child showing cervical lymphadenopathy.
Investigations showed raised leucocyte counts(37310/cu. mm), erythrocyte sedimentation rate (70 mm in the first hour) and CRP (95.4 IU/ml).An ultrasonographic evaluation of neck showed multiple enlarged hypo to anechoic lesions on both sides of the neck, suggestive of cervicallymph nodes. Ultrasound abdomen did not show any mesenteric lymphadenopathy.FNAC (Fine Needle Aspiration Cytology) from lymph nodesshowed a polymorphous population of small and large lymphocytes with few uninucleate and binucleate histiocytes exhibiting emperipolesis. The presence of reactive lymphoid hyperplasia with histiocytosis and focal emperipolesis was suggestive of a diagnosis of RDD (Figure 2a).He was also subjected to excisional biopsy from the lymph node elsewhere for which we did a slide review. Immunohistochemistry showed strong positivityfor S100 protein (Figure 2b) and negativity for CD1a (Figure 2c).
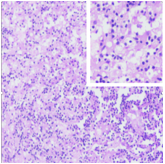
Figure 2a: H&E staining showing mature lymphoid tissue within large histiocytes (emperipolesis).
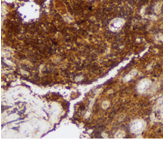
Figure 2b: Histopathological image showing strongly positive S 100 stain on Immunohistochemistry.
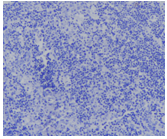
Figure 2c: Histopathological image showing CD1a negative staining on Immunohistochemistry.
ZiehlNeelsen (ZN) staining revealed noacid-fast bacilli. Thus, the diagnosis of Rosai-Dorfman Disease was established. The child was started on oral steroids(Tablet Prednisolone 0.5mg/kg) in consultation with pediatrician for six weeks with good clinical response. The dose was then tapered (Tab Prednisolone 0.25 mg/kg) over another 6 weeks and treatment was stopped. After a month, the child again developed bilateral cervical lymphadenopathy.He was started on low dose oral steroid (Tab Prednisolone 0.25 mg/kg/day) therapy for 3 months which was tapered slowly over the next 3 months. With continuous steroid therapy, the child developed moon facies (Figure 3a).
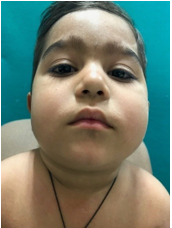
Figure 3a: Clinical image of the child showing development of Moon facies due to prolonged steroid therapy.
After 6 months, treatment was stopped and he was kept on close follow up.At the end of one steroid free year, the child remains asymptomatic with complete resolution of side effects (Figure 3b).
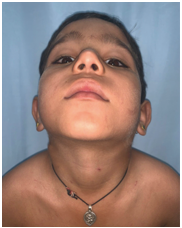
Figure 3b: Clinical image showing complete resolution of symptoms as well as side effects.
Discussion
The most common presentation of Rosai Dorfman Disease is painless massive cervical lymphadenopathy (bull neck) [1]. It may involve extranodal organs such as the central nervous system [4],orbit [5], skin [6] and may mimic malignancy which further complicates the diagnosis and management. It may also be associated with intermittent fever, malaise andweight loss. It shows childhood predilection but can present at any age [3]. Diagnosis is confirmed only with histopathological examination and immunohistochemistry, characterized by the abundance of large foamy histiocytes with emperipolesis along with plasma cells [7]. The clinical course is unpredictable and diverse, usually benign and resolves spontaneouslybut can be very aggressive in nature and can even lead to death [8]. Reasons for the aggressiveness or spontaneous remission are unknown.In this young child, there was no spontaneous remission of cervical lymphadenopathy. After histopathological confirmation, oral steroids were started and there was a dramatic disappearance of lymphadenopathy. However, as the steroids were tapered and stopped, the symptoms again flared up, necessitating the continuation of treatment. Various treatment modalities, for example, chemotherapy (Vinca alkaloid, an alkylating agent and corticosteroid) and radiotherapy have been tried with variable success rates [2]. Nevertheless, literature is inadequate to support the use of either. This observation prompted us to continue the steroids after dose titration to the lowest dose possible. After a year of stopping steroid therapy, the child remains asymptomatic and free of side effects.
Conclusion
The diagnosis of RDD is challenging due to its varied clinical course, as well as nonspecific histopathological appearance andrequires good coordination between the clinician and pathologist. However, trickier than the diagnosis is the treatment owing to lack of sufficient evidence to support the various existing therapeutic modalities.Steroids can be considered as an effective and safe treatment option with fewer side effects under controlled dosage and proper follow up.
Authorship Criteria
Darwin Kaushal: Concept and design of study, Final approval, 'guarantor'
Aman Kumar Verma: Drafting the article
Vidhu Sharma: Drafting the article& Critical Revision
Poonam Elhence: Drafting the article or revising it critically
Prawin Kumar: Drafting the article or revising it critically
Conflict of Interest
None
Grant Information
The author(s) received no specific funding for this work.
Acknowledgements
Informed written consent was taken from the guardian of the patient for clinical photograph.
References:
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: A pseudolymphomatous benign disorder.Analysis of 34 cases. Cancer. 1972;30(5):1174-88.
- Maia RC, de Meis E, Romano S, Dobbin JA, Klumb CE. Rosai-Dorfman disease: a report of eight cases in a tertiary care center and a review of the literature. Braz J Med Biol Res. 2015;48(1):06-12.
- Newman B, Hu W, Nigro K, Gilliam AC. Aggressive histiocytic disorders that can involve the skin. J Am Acad Dermatol. 2007;56(2):302-16.
- Andriko JA, Morrison A, Colegial CH, Davis BJ, Jones RV. Rosai-Dorfman Disease isolated to the Central Nervous System: A Report of 11 Cases. Mod Pathol. 2001;14(3):172-8.
- Petrushkin H, Salisbury J, O’Sullivan E. Intralesional steroid for orbital manifestations of Rosai-Dorfman disease. Clin Exp Ophthalmol. 2015;43(5):483-5.
- Kutlubay Z, Bairamov O, Sevim A, Demirkesen C, Mat MC. Rosai–Dorfman Disease: A Case Report with nodal and cutaneous involvement and review of the literature. Am J Dermatopathol. 2014;36(4):353-7.
- Averitt AW, Heym K, Akers L, Castro-Silva F, Ray A. Sinus Histiocytosis With Massive Lymphadenopathy (Rosai Dorfman Disease): Diagnostic and Treatment Modalities for this Rare Entity Revisited. J Pediatr Hematol Oncol. 2018;40(4):e198-202.
- Foucar E, Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: Current status and future directions. Arch Dermatol. 1988;124:1211-1214.

