Non-Operatively Managed Primary Small Bowel Volvulus: A Case Report
Ewnte B*
Department of General Surgeon, Debre Tabor University, Ethiopia
Received Date: 09/09/2020; Published Date: 10/11/2020
*Corresponding author: Biniam Ewnte, Department of General Surgeon, Debre Tabor University, Debre Tabor, Ethiopia. E-mail: newbeneh@yahoo.com
Abstract
Background: Primary small intestinal volvulus is one of the common causes of intestinal obstruction in various localities of the developing world. Although operative intervention has been the usual mode of treatment; this case report depicts meticulous follow-up & care, there is a possibility for relief of obstruction with non-operative management.
Case presentation: this is a case report of a 20-year-old male patient presented with crampy abdominal pain and frequent bilious vomiting. Plain abdominal film showed multiple distended small bowel loops with air fluid level, consistent with small bowel obstruction. Ruling out other etiologies primary small bowel volvulus was entertained and naso-gastric tube inserted, patient catheterized and kept nil per oral. After 48 hours of admission all symptoms resolved the patient resumed feeding and was discharged home.
Conclusions: The reported case shows evidence in which the patient’s primary small bowel volvulus was relieved non-operatively with insertion of naso gastric tube keeping nil per oral.
Key words: Small bowel volvulus; Primary volvulus; Non-operative management
Abbreviations: BPM: Beats Per Minute; WBC: White Blood Cells; RBC: Red Blood Cells; HGB: Hemoglobin; HCT: Hematocrit; MCV: Mean Corpuscular Volume; BUN: Blood Urea Nitrogen; ALT: Alanine Aminotransferase; AST: Aspartate Aminotransferase; ALP: Alkaline Phosphatase
Introduction
Small bowel volvulus is a condition in which there is a torsion of all or a segment of the small bowel and its mesentery: this can lead to bowel obstruction, ischemia, infarction, or perforation. The typical patient with the primary volvulus of the small intestine was found to be a young adult, male, muscular, farmer, from a rural area whose diet was bulky and mainly made of cereals [1,2].
Case Presentation
A 20-year-old male patient presented to Nefas Mewcha primary hospital Emergency department in January 2020 with the main complaint of crampy abdominal pain and distention of 14 hours duration. Associated with this, he also had nausea and frequent bilious vomiting eight times. He had passed feces 24 hours ago. He had no fever, cough, chest pain or night sweating. He had no history of similar illness before, no history of previous abdominal surgery.
He is not married and claims to be not sexually active. Lives with his parents and has three sisters and two brothers. He makes a living as a farmer. There are no medical illnesses that run in the family. There was no history of tobacco smoking or substance abuse. He consumes a local alcohol made of sorghum occasionally.
At presentation, his blood pressure was 105/60 mm Hg, pulse rate was 68 Beats Per Minute (BPM), respiratory rate was 18 per minute and temperature was 36.2 oC axillary. Physical examination of the patient at presentation, the patient was acutely sick looking in pain; not in cardio respiratory distress. He had a dry tongue and buccal mucosa. No palpable lymph adenopathy in all accessible areas. Chest was clear and resonant. S1 and S2 cardiac sounds were well heard and there were no added cardiac sounds. Abdomen was slightly distended, moves with respiration, flanks were full, there were no scars, no distended veins and hernia sites were free. Palpation revealed a tense abdomen with no area of tenderness, no shifting dullness, hyperactive tympanic percussion note, bowel sounds were 35 per minute. There is scanty stool on the examining finger, with no blood on it from digital rectal examination, no palpable mass was detected. The patient was conscious and neurological examination was intact.
A complete blood count of our patient showed: White Blood Cells (WBC) 12500 mcL, Red Blood Cells (RBC) 4.6 mcL, Hemoglobin (HGB) 16 gm/dL, Hematocrit (HCT) 48%, Mean Corpuscular Volume (MCV) 89.1fL, platelets 470×103, creatinine 0.6, Blood Urea Nitrogen (BUN) 30, Alanine Aminotransferase (ALT) 28, Aspartate Aminotransferase (AST) 24, Alkaline Phosphatase (ALP) 48, albumin 4.3, total bilirubin 1.1 and direct bilirubin 0.4.
Plain abdominal X-Ray showed centrally distributed, distended small bowel loops and rectal gas shadow (Figure 1). CT scan is not available at this setup so it was not possible to do one.
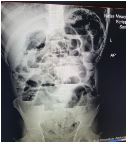
Figure1: Plain Abdominal X-Ray showing distended small bowel loops with multiple Air Fluid levels.
Management and Outcomes
The diagnosis of acute abdomen secondary to small bowel obstruction secondary to primary small bowel volvulus plus stage I shock was entertained, Double intravenous line was inserted and Trans-urethral catheter inserted, Naso-gastric tube was inserted. Three Liters of normal saline was given over a course of 2 hours, at emergency department. The patient was admitted to the ward and was advised on the possible options of management, consented on conservative management, associated risks and the possibility of surgical intervention at any time in the course of the management. The patient was kept Nil per oral, put on maintenance fluid and replacement of ongoing losses. Nasogastric tubes produced 600 ml of bilious content during the first 6 hours; which was replaced with an equal amount of ringer lactate. The abdominal cramp subsided after 4 hours of inpatient admission. After 12 hours of admission, the Blood pressure was 100/70 mmHg, pulse rate 68 per minute and the abdominal distension decreased significantly and the bowel sounds were 26 per minute, there was no area of tenderness and the patient passed flatus.
Following 24 hours of admission, the patient passed feces and vital signs were within normal range. Naso-gastric was removed and the patient was initiated with sips. The patient tolerated sips very well and was observed for 24 more hours and discharged on the next day. He was appointed to the surgical referral clinic after a week.
In subsequent weeks, the patient was seen at a referral clinic; he had no change in bowel habit or any other complaint. His vital signs were stable and physical examination was detected with no abnormality. He has been followed every month for 3 consecutive months and has reported no recurrence of symptoms.
Discussion
Volvulus is the Latin word for rolled up or twisted and is derived from the verb ‘volvere’, meaning to roll or turnabout. By definition, volvulus is an abnormal twisting of the intestine, which can impair the blood flow to the intestine. Volvulus can lead to gangrene and death of that segment of the gastrointestinal tract, intestinal obstruction, perforation of the intestine and peritonitis [3]. Small intestinal volvulus in adults can be classified as primary or secondary. In the former there is no obvious anatomical cause involving the mesentery or the small bowel, whereas in the latter there is an abnormal fixation due to adhesions or bands leading to the twisting of the mesentery. The primary type is often seen in Africa and Asia [4]. It is a significant cause of primary bowel obstruction in sub-Saharan Africa [5]. It is the leading cause of small bowel obstruction in Ethiopia [6].It is a rare entity in Western adults [7].
Clinical signs & symptoms were unspecific & resembled intestinal obstruction [8]. The most frequent symptom was observed to be sudden abdominal pain [9]. Vomiting was also observed in most of the patients while abdominal distention and constipation were reported less frequently [10]. Clinical examination reveals abdominal distension and/or diffuse tenderness with or without signs of peritonitis [8]. Small bowel volvulus is a rare but life-threatening surgical emergency. Owing to its rarity, it is seldom entertained as a differential for small bowel obstruction [11].
One of the challenges in managing primary small bowel volvulus operatively has been the risk of subsequent adhesion obstructions. The risk of occurrence of adhesion obstructions among patients that underwent laparotomy in general was reported to be 4.6% [12]. This gives rise to the endless circle of obstruction and subsequent operation, which further increase the risk more.
This case report presents a case of primary small bowel volvulus causing small bowel obstruction; which was managed non-operatively. Treatment of primary volvulus has mostly been via surgical intervention. This report depicts with close follow-up and Naso-gastric tube decompression, primary small bowel volvulus can also be treated without surgical intervention.
In the course of managing patients with primary small bowel volvulus, spontaneous resolutions has been observed [3]. This is because of natural de-rotation of the volvulus segment and relief of the obstruction. The case reported presented with symptoms and signs of small bowel obstruction. The patient has frequent vomiting with severe abdominal cramp associated with mild abdominal distension. The vital signs were within normal range supporting the diagnosis of non-ischemic obstruction. Abdominal x-ray showed multiple air fluid levels, which confirmed the diagnosis of small bowel obstruction. Ruling out other causes and considering the epidemiological prevalence, primary small bowel volvulus was entertained as a cause of obstruction.
As per the request of the patient to be followed conservatively, the patient was managed non-operatively with insertion of naso gastric tube and keeping nil per oral. The patient responded well for the management and were discharged subsequently. Showed no recurrence during the follow-up period.
Conclusion
Primary Small bowel volvulus is a rare cause of small bowel obstruction. The reported case shows evidence in which the patient’s primary small bowel volvulus was relieved non-operatively with insertion of naso gastric tube keeping nil per oral.
References:
- Ghebrat K. Trend of small intestinal volvulus in north western Ethiopia. East African medical journal. 1998;75:549-552.
- Ayalew T. Small intestinal volvulus in adults of Gonder region, northwestern Ethiopia. Ethiopian Medical Journal. 1992;30:111-117.
- Bhullar JS, Papapetrou P, Subhas G, Gupta N, Seman S and Mittal VK. Spontaneous resolution of primary small bowel volvulus with oral contrast. Journal of Current Surgery. 2012;2:110-112.
- Iwuagwu O and Deans GT. Small bowel volvulus: a review. Journal of the Royal College of Surgeons of Edinburgh. 1999;44:150-155.
- Purcell LN, Reiss R, Mabedi C, Gallaher J, Maine R and Charles A. Characteristics of intestinal volvulus and risk of mortality in Malawi. World journal of surgery. 2020;4:2087-2090.
- Demissie M. Small intestinal volvulus in Southern Ethiopia. East African medical journal. 2001;78:208-211.
- Coe TM, Chang DC and Sicklick JK. Small bowel volvulus in the adult populace of the United States: results from a population-based study. The American Journal of Surgery. 2015;210:201-210.
- Li X, Zhang J, Li B, Yi D, Zhang C and Sun N, et al. Diagnosis, treatment and prognosis of small bowel volvulus in adults: a monocentric summary of a rare small intestinal obstruction. PloS one. 2017;12:e0175866.
- Ruiz-Tovar J, Morales V, Sanjuanbenito A, Lobo E and Martinez-Molina E. Volvulus of the small bowel in adults. The American surgeon. 2009;75:1179-1182.
- Ng YYR, Ngu JCY and Wong ASY. Small bowel obstruction in the virgin abdomen: time to challenge surgical dogma with evidence. ANZ journal of surgery. 2018;88:91-94.
- Islam S, Hosein D, Dan D and Naraynsingh V. Volvulus of ileum: a rare cause of small bowel obstruction. Case Reports. 2016;2016:bcr2016216159.
- Barmparas G, Branco BC, Schnüriger B, Lam L, Inaba K and Demetriades D. The incidence and risk factors of post-laparotomy adhesive small bowel obstruction. Journal of Gastrointestinal Surgery. 2010;14:1619-1628.

