Mycobacterium Paraffinicum: A Rare Non-Tuberculous Mycobacterium Pulmonary Infection
Santiago HOC1*, Ramírez KM1, Ricardo F1, Colón M1, Caliz MJC2 and Rodríguez KCP1
1Department of Pulmonary and Critical Care Medicine, San Juan City Hospital, Puerto Rico
2Department of Pulmonary and Critical Care Medicine- Auxilio Mutuo Hospital, Puerto Rico
Received Date: 10/10/2020; Published Date: 07/11/2020
*Corresponding author: Hector O Collazo Santiago, Department of Pulmonary and Critical Care Medicine, San Juan City Hospital, PO Box 70344, San Juan, Puerto Rico. Tel: 787-607-4516; E-mail: omar_collazo@hotmail.com
Abstract
Introduction: Mycobacterium paraffinicum has been isolated from numerous soil samples from widely distributed oil fields. In 1971 M. paraffinicum was not considered a legitimate Mycobacterium species because of the phenotypic confusion with M. scrofulaceum. However, after an extensive molecular sequence analysis in 2010, it was finally reincorporated into the taxonomy.
Case presentation: An 85-years-old, former smoker man came to the emergency department complaining of worsening exertional dyspnea of several months of evolution. A chest CT scan revealed a large cavitary lesion associated with multiple smaller nodes with central cavitation throughout both lung fields. A flexible bronchoscopy was performed and the bronchoalveolar lavage culture was positive for M. paraffinicum.
Conclusion: To our knowledge there are only two published cases of pulmonary infection by this pathogen. To date there is no standard drug therapy regimen for M. paraffinicum infection. More research and development are needed in this field as to improve diagnostic and treatment for this rare disease.
Keywords: Mycobacterium paraffinicum; Taxonomy; Flexible bronchoscopy; Nontuberculous mycobacterium
Abbreviations: AFB: Acid Fast Bacilli; NTM: Nontuberculous Mycobacterium; RIPE: Rifampin Isoniazid Pyrazinamide Ethambutol; PPD: Purified Protein Derivative.
Introduction
Mycobacterium paraffinicum has been isolated from numerous soil samples from widely distributed oil fields [1]. Originally isolated in 1956 and described as a long, slender, strongly acid-fast rods showing Much's granules with Ziehl-Neelsen stain; which produced yellow, waxy, wrinkled colonies. In 1971 M. paraffinicum was not considered a legitimate Mycobacterium species because of the phenotypic confusion with M. scrofulaceum. However, in 1991 a review of rarely encountered mycobacterial diseases acknowledged that it had obviously different biochemical responses from M. scrofulaceum and after an extensive molecular sequence analysis in 2010, it was finally reincorporated into the taxonomy [1]. Investigation of antimicrobial susceptibility was done, and results showed that M. paraffinicum’ strains were susceptible in vitro to rifabutin, linezolid, clarithromycin, and amikacin [2].
Case Presentation
We present an 85-years-old, former smoker man with a past medical history of colon adenocarcinoma status post colostomy, hypertension, hypothyroidism, and glaucoma complaining of worsening exertional dyspnea of several months of evolution. He denied cough, unintentional weight loss, fever, chills, night sweats, hemoptysis recent travel, and exposure to tuberculosis, asbestos or silica. Physical examination was unremarkable. Initial chest CT scan revealed a large cavitary lesion of approximately 4.5x4.2 cm, in addition to multiple smaller nodes with central cavitation throughout both lung fields (Figure 1). PPD skin test was negative. PET-Scan showed increased FDG concentration with uneven distribution on the upper lobe posteromedial aspect of right lung with a maximum SUV of 12.3. A flexible bronchoscopy was performed and the bronchoalveolar lavage sample was positive for Acid Fast Bacilli smear (AFB), for which he was started on RIPE therapy. Unexpectedly, AFB culture revealed M. paraffinicum growth and thus, RIPE therapy was discontinued and intravenous imipenem, azithromycin and amikin were started. In view of adequate clinical response, he was discharged approximately one month later with azithromycin and ciprofloxacin. Subsequent chest CT scan was performed 3 months later in which marked improvement was noted compared with the previous images.
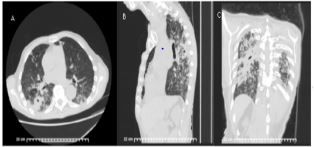
Figure 1: (A) CT thorax with (B) sagittal and (C) coronal views showing a large cavitary spiculated mass seen in the dependent portion of the superior aspect of the right lower lobe with surrounding sub-centimeter branching centrilobular nodules.
Discussion
M. Paraffinicum is a slow growing mycobacterium, and a rare cause of clinical Nontuberculous Mycobacterium infection (NTM). It was initially described in pseudo outbreak; however, it is capable of causing symptomatic lung disease [3]. To date, little is known about its pathogenic potential, drug susceptibility profile, and treatment outcome. To our knowledge there are only three published cases of pulmonary infection by this agent, all treated with similar antibiotic regimen with adequate clinical response [1,4,5]. More research and development are needed in this field as to improve diagnostic and treatment for this rare disease.
Conclusion
To date there is no standard drug therapy regimen for M. paraffinicum infection. More research and development are needed in this field to improve diagnostic and treatment for this rare disease.
Acknowledgement
We would like to thank all the other staff from Auxiluo Mutuo Hospital and San Juan City Hospital who have contributed to this case report.
References:
- Chan AW, Kabbani S, Staton G, Kraft CS. Mycobacterium paraffinicum causing symptomatic pulmonary infection. Journal of clinical microbiology. 2014;52:1281-1283.
- Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27:727-752.
- Wang SH, Pancholi P, Stevenson K, Yakrus MA, Butler WR. Pseudo-outbreak of "Mycobacterium paraffinicum" infection and/or colonization in a tertiary care medical center. Infection control and hospital epidemiology. 2009;30:848-853.
- Barretto AR, Monteiro J, Lopes ML, da Costa A. A case of pulmonary infection due to Mycobacterium paraffinicum from the Amazon Region. IDCases. 2017;10:1-3.
- Pei Sze, CT, Ruad P. A rare case of lymphadenitis and pulmonary disease caused by Mycobacterium paraffinicum. Respirology Case Reports. 2019;7:1-3.

