A Case Report of Neonatal Intussusception
Khairunnisa CG¹, Ridzuan AS¹
¹Paediatric Surgery Unit, Department of General Surgery, Hospital UniversitiSains Malaysia
Received Date: 17/08/2020; Published Date: 23/09/2020
*Corresponding author: Khairunnisa CG, Paediatric Surgery Unit, Department of General Surgery, Hospital UniversitiSains Malaysia. E-mail: khairunnisacg@gmail.com
Abstract
Neonatal intussusception is deemed rare, accounting <1% of all childhood intussusception. The cardinal signs difficult to elicit due to extreme age of presentation. However, the diagnosis should always be in mind when dealing with unwell neonates.
Case Report
Baby of NA, A baby boy who was born term at 39 weeks via spontaneous vaginal delivery with a birth weight of 3kg. The baby passed out meconium right after birth. The initial meconium was yellowish in colour. However, on day 2 of life, the baby passed out meconium mixed with fresh blood for two episodes (Figure 1).

Figure 1: Showed meconium mixed with blood.
Otherwise, there was no abdominal distension or anal excoriation. There was no history of intolerant feeding or vomiting. The baby was given IM Vitamin K injection at birth. There was no family history of blood dyscrasias.
On examination, child was active on handling, CRT less than 2 seconds, jaundice up till chest region on single phototherapy. Blood pressure of 79/47mmHg, heart rate of 130bpm, oxygen saturation of 98% under room air. Lungs were clear, abdomen soft, not distended, no mass palpable, bowel sound was present and active.
In view of hemorrhagic disease of newborn, blood parameters were taken and no abnormality noted. Plain abdominal radiograph (AXR) showed no bowel dilatation. We proceed with ultrasonography of abdomen, which showed presence of pseudokidney and doughnut sign at right lumbar region with surrounding free fluid (Figure 2&3).

Figure 2: Showed plain abdominal radiograph.
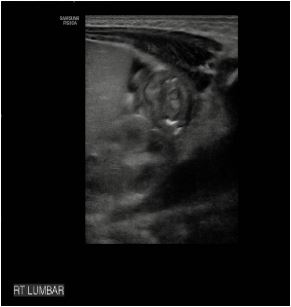
Figure 3: Showed pseudokidney sign at right lumbar region with free fluid surrounding.
The findings were intermittently seen during examination (spontaneously reduced and then demonstrable intussusception and then reduced again). There was normal orientation of SMA and SMV. The visualised splenic vein is normal with normal flow colour on Doppler and no intraluminal thrombus seen. The features were in keeping with intermittent intussusception.
With the findings given, and continuous assessment of the baby, decision made to manage him conservatively. He was kept nil by mouth, started on antibiotics for presumed sepsis. He still passed out blood mixed with stool on the next day. We arranged a barium study subsequent day. There was no demonstrable intraluminal pathology or lead point seen, and there was no intussusception (Figure 4&5).


Figure 4 and 5: Showed opacification of contrast from rectum to descending, transverse, ascending and caecum. No luminal stricture, narrowing or filling defect seen.
The baby was kept observed for the next 72 hours. He passed out yellowish stool. No more per rectal bleeding episode noted. There was no dropped in haemoglobin level. He tolerated expressed breast milk well, no vomiting, and no abdominal distension. He was discharged well on day 7 of life.
On follow up after one month and three month later, mother claimed child is well, passing out yellowish brownish stool. No more per rectal bleeding. The child is thriving well.
Discussion
Intussusception is the invagination of a segment of bowel into the distal adjacent bowel. Commonly it involves distal ileum and proximal colon and no lead point identified. It is a common cause of bowel obstruction in a less than two year of age [1]. Neonatal per rectal bleeding and intussusception is rare and comprises of 0.3% of all cases of childhood intussusception (2–4). Often vomiting and blood in the stool are the commonest symptoms. The incidence of intussusception in UK is about 1.6-4 cases per 1000 live birth. It is slightly commoner in boys than girls with ratio of 3:2 (5).
Abdominal pain and palpable abdominal mass are uncommon features in neonate, however if these are present, the diagnosis of intussusception can be made confidently [2]. Classical triad often described that patient will have colicky abdominal pain, vomiting and bloody stool [2,5]. However, in this case, since the patient is only 48 hours of life, only signs can be elicited. The most common intussusception at ileocolic, accounting about 80% of cases. Others are colocolic, rare for small bowel (ileoileal) intussusceptions [3,5]. Only about 2-12% of lead point can be identified in intussusception, but most neonates and infant do not have identifiable lead point [5].
Plain abdominal radiograph may show bowel dilatation if there is evidence of intestinal obstruction, but this is inconclusive. In United Kingdom, universally abdominal ultrasonography (USG) is the investigation of choice. It has sensitivity of 98% and specificity of 100% when looking for features of intussusception. The signs that suggestive evidence of intussusception are target and pseudokidney sign [1,5]. In our case, it was proven by USG image presence of those signs.
For this case, once diagnosis is established, fluid resuscitation was administered and antibiotics started for presumed sepsis. We arranged for barium study however intussusception spontaneously reduced upon investigation done. Therefore, the baby was managed conservatively. Non-operative management consist of saline, air or barium reduction. This procedure is performed by experienced radiologist under USG or fluoroscopy guidance. The success of procedure is determined by saline or contrast flow into proximal ileum. The contraindication for this procedure if patient has peritonitis or in shock. Saline or barium reduction success rate is about 70-80% of cases [1,5]. Presence of peritonism, perforation and failure of hydrostatic reductionare the indication for laparotomy. Open laparotomy and open reduction is the definitive management.
References:
- Lopes J, Huddart SN. Paediatric surgery ii. Surgery. 2013;31(12):626-30.
- Talwalker VC, Report C. INTUSSUSCEPTION IN THE NEWBORN. Arch Dis Child. 1961.
- PV Anand, R Ragupathy, V Kumaran, R Krishnaswami, D Nagalakshmi, G Girivasan NS. Neonatal Intussusception A Surgical Rarity.pdf. J Indian Assoc Pediatr Surg. 2004;9:198-200.
- Pollack C V, Pender ES. UNUSUAL CASES OF INTUSSUSCEPTION. J Emerg Med. 1991;9(July 1990):347-55.
- Robb A, Lander A. Intussusception in infants and young children. Surg - Oxford Int Ed. 2008;26(7):291-3.

