A Rare Case of Takotsubo Cardiomyopathy Following Head and Neck Oncologic Surgery
Robert T Cristel1, Brown L1 and Elise L2
1University of Illinois at Chicago, Department of Otolaryngology Head & Neck Surgery, 1855 W. Taylor, Suite 2.42, Chicago, IL 60612, USA
2Department of Otolaryngology Head and Neck Surgery, Harvard Medical School, Massachusetts Eye and Ear Infirmary, Boston, MA, USA
Received Date: 15/08/2020; Published Date: 01/09/2020
*Corresponding author: Robert T. Cristel, University of Illinois at Chicago, Department of Otolaryngology-Head & Neck Surgery,1855 W. Taylor, Suite 2.42, Chicago, IL 60612, USA. Tel: 314-440-7441; Email: Rcrist3@uic.edu,
Abstract
Takotsubo cardiomyopathy (TTC) is a rare cardiac syndrome, particularly in the head and neck oncologic surgery population. There have been only 5 prior cases reported in the literature of TTC following head and neck oncologic surgery, all with patients over the age of 60. TTC is an acute, self-resolving form of left ventricular dysfunction often triggered by severe emotional or physical stress, such as surgery. We report the case of a 23-year-old male that underwent right hemiglossectomy, right selective neck dissection, and radial forearm free flap that developed TTC following surgery.
Key Words: Takotsubo Cardiomyopathy; Head And Neck Oncologic Surgery; Reconstructive Surgery
Introduction
Takotsubo cardiomyopathy (TTC) is a rare cardiac syndrome, particularly in the head and neck oncologic surgery population. There have only been 5 prior cases reported in the literature of TTC following head and neck oncologic surgery [1-4]. TTC is characterized by an acute, transient and reversible left ventricular dysfunction, often triggered by severe emotional or physical stress, in the absence of obstructed coronary arteries [5-7]. TTC was initially described in 1990 and named after the appearance of the patient’s left ventricle in systole on an echocardiogram resembling a Japanese octopus trap (Figure 1A-1B) [6,8]. In the majority of patients, including the 5previously reported cases in the head and neck population, the mean age is reported to be 61-76 years [1-4,7]. We report an unusual case of TTC following head and neck oncologic surgery in a young 23-year-old male with oral cavity squamous cell carcinoma.
Case Report
A 23-year-old male from Democratic Republic ofthe Congo was found to have oral cavity (tongue)p16 negative squamous cell carcinoma (SCCa).He had no other medical or surgical history and was not on any medications. He was a non-smoker and did not use alcohol. The patient underwent a sentinel lymphoscintigram followed by a partial glossectomy. A right perifacial node was found on lymphoscintigram, excised, and found to be positive for SCCa. The extent of tumor invasion was found to be much greater than initially seen on physical exam and imaging. The operation was aborted to plan for definitive resection and reconstructive surgery. This procedure lasted 3 ½ hours.
The patient returned 1 week following his initial procedure for completion right hemiglossectomy, right selective neck dissection levels I-IV, and radial forearm free flap. The procedure was completed without complication and lasted 9 hours. Final pathologic staging was confirmed to be pT3N1M0 SCCa of the oral cavity, tongue. Upon extubation, his heart rate elevated to 160 beats per minute (bpm), 180bpm and 220bpm at three separate time periods over a 15-minute window. His blood pressure remained within the normal range during this time and after the 15-minute window, his heart rate returned to the normal range.
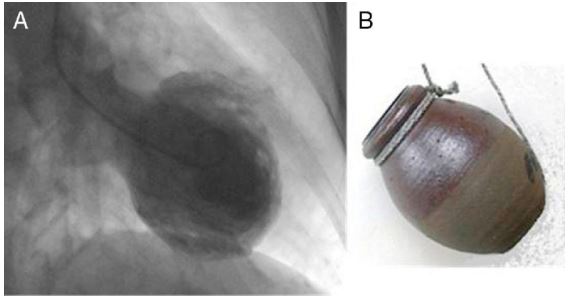
Figure 1a: Representative echocardiogram image demonstrating apical ballooning and hypokinesis in takotsubo cardiomyopathy.
Figure 1b: Representative image of a takotsubo, Japanese octopus fishing pot.
On the first postoperative night, he was bradycardic between 50-60bpm. He denied any chest pain or shortness of breath. An electrocardiogram (ECG) on POD 1 found sinus bradycardia with sinus arrhythmia and an incomplete right bundle branch block. The patient remained asymptomatic with heart rate as low as 48bpm. A repeat ECG was performed on POD 2 and revealed sinus arrhythmia, moderate ST depression and possible right ventricular hypertrophy. Cardiology was consulted and an echocardiogram was performed. The echocardiogram revealed diffuse hypokinesis of the left ventricle with a reduced ejection fraction of 40-45%, and severe hypokinesis of the mid-apical anterior, apical lateral, and apical myocardium. He was diagnosed with Takotsubo cardiomyopathy and started on benazepril and metoprolol. Psychiatry was also consulted due to concern for anxiety and depression. He was diagnosed with adjustment disorder and started on mirtazapine. The patient remained asymptomatic throughout his postoperative course and was discharged on benazepril and metoprolol.He completed a 1-month course of his cardiac medications and had no long-term sequelae of TTC.
Discussion
Takotsubo cardiomyopathy is a relatively uncommon diagnosis of transient and self-resolving heart failure typically limited to the elderly, including the head and neck population [1-4]. The development of TTC in our 23-year-old patient is the first patient under the age of 60 to be reported in the head and neck oncologic surgery literature. TTC commonly presents with chest pain and dyspnea and has been reported to occur following significant stressors such as emotional triggers or physical triggers such as malignancy, infection, and surgery [1,6,7]. Some patients may remain asymptomatic, as in our patient, and findings are only found on ECG or echocardiogram [7]. The exact mechanism of TTC remains unknown, yet excess catecholamine release and activation is one of the leading theories which produces oxidative stress on the myocardium [5-7].
ECG and echocardiogram are the two most commonly performed procedures when TTC is suspected.ECG findings vary but often include ST segment elevation, depressions or T-wave inversion [6,7]. The echocardiogram more reliably shows characteristic apical wall changes including hypokinesia, akinesia, or dyskinesia with reduced ejection fractions.7 The Mayo Clinic is a commonly used guidelinefor diagnostic criteria (Figure 2), though many variants of diagnostic criteria exist [6,9]. Management of TTC is primarily supportive. Beta-blockers are often used to counteract the excessive catecholamine release [5,7] and angiotensin-converting enzyme inhibitors (ACE inhibitors) are commonly used to reduce after load and increase ejection fraction [5].
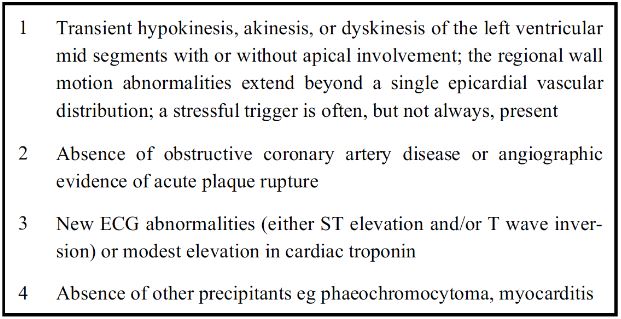
Figure 2: Mayo Clinic Diagnostic Criteria for Takotsubo Cardiomyopathya.
All criteria must be met for diagnosis
TTC typically resolves spontaneously within days to weeks with the majority of patients having no acute or long-term complications [5-7]. The recurrence rate has been reported from 0-15%and is of particular importance in head and neck surgery where patients may return with disease recurrence that requires further surgery [6,7]. While surgery is a known risk factor for the development of TTC, this is a very rare occurrence in a 23-year-old patient. This patient underwent two separate procedures within a 1-week period with the first surgery being 3 ½ hours, and the second lasting 9 hours. He was also diagnosed with adjustment disorder in the early postoperative period. This combination likely led to his development of TTC despite his otherwise healthy and active lifestyle.
Conclusion
This is the first case of TTC in a young patient, under the age of 60, following head and neck oncologic surgery. TTC is typically a transient, self-resolving condition, but requires prompt recognition and treatment to ensure positive outcomes.
Conflict of Interest
No funding sources were obtained to support this work. The authors claim no conflict of interests.
References:
- Gerecci D, Sullivan B, Burchill LJ, Clayburgh DR. Takotsubo Cardiomyopathy following Head and Neck Oncologic Surgery: A Case Report. Oto Open. 2016:1-2.
- Jeon D, Park K, Lee J, Kim U, Kim E, Yoon J. Takotsubo cardiomyopathy in a patient with oral cancer. J Dent Anesth Pain Med. 2015;15(3):157-160.
- Mori M, Nagashima H, Akazaw S, et al. Takotsubo Cardiomyopathy after Head and Neck Reconstructive Surgery. PRS Global Open. 2017:1-4. DOI: 10.1097/GOX.0000000000001366.
- Brooks JK, Warburton G, Clark BC. Takotsubo Syndrome After Surgical and Nonsurgical Oral and Maxillofacial Events: Review of Published Cases. J Oral Maxillofac Surg. 2019;77:478-488.
- Kurisu S, Kihara. Clinical Management of Takotsubo Cardiomyopathy. Circulation Journal. 2014;78:1559-1566.
- Ono R, Falcao. Takotsubo cardiomyopathy systemic review: Pathophysiologic process, clinical presentation and diagnostic approach to Takotsubo cardiomyopathy. Int J of Cardiology. 2016;209:196-205.
- Roshanzamir S, Showkathali R. Takotsubo Cardiomyopathy A Short Review. Current Cardiology Reviews. 2013;9:191-196.
- Cesario V, Loureiro MJ, Pereira H. Takotsubo cardiomyopathy in a cardiology department. Rev Port Cardiol. 2012;31(9):603-608.
- Prasad A. Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction. Circulation. 2007;115(5):e56-59.

