The Role of Surgical Hip Dislocation in the Management of Selected Traumatic Injuries: A Case Series
Thiago SB1, Artur A2, Marcelo M3, Lucas DG3, Gladyston RMF3, Julian C3 and Juan RVC4
1Department of Surgery, Chair of CRIAr Hip Surgery Fellowship Programme, Curitiba, Brazil
2Department of Orthopedic Surgery, Former Fellow of CRIAr, Curitiba, Brazil
3Department of Orthopedic Surgery, Staff of Hip Surgery Group, Curitiba, Brazil
4Department of Hip Surgery, Curitiba, Brazil
Received Date: 07/08/2020; Published Date: 27/08/2020
*Corresponding author: Thiago Sampaio Busato, Department of Surgery, Chair of CRIAr Hip Surgery Fellowship Programme, Curitiba, Brazil. Email: tsbusato@hotmail.com
Abstract
Objective: We aimed to report our initial experience with hip surgical dislocation in a series of cases of different traumatic injuries. We have reviewed the relevant literature. Ganz initially described the surgical hip dislocation as a technique for treating femoroacetabular impingement through a safe hip dislocation. The method was later described as an auxiliary tool for managing specific patterns of acetabular and femoral head fractures.
Methods: We retrospectively analyzed 10 cases of traumatic injuries treated at our institution using the controlled Ganz dislocation from 2013 to 2015.
Results: The main indication found was an acetabular fracture. Other indications were fractures of the femoral head in two cases and two cases of withdrawal of an intra-articular firearm projectile. The average age was 37.2 years, all individuals were male, with a follow-up of 23.5 months. At the endpoint, all osteotomies healed, and there was no case of avascular necrosis of the femoral head. The results found in this study were similar to those in the literature.
Conclusion: In our experience with the Ganz technique applied to selected trauma cases, there was clinical and radiographic healing of the trochanteric osteotomy in all cases. There was no episode of aseptic necrosis of the femoral head until the mean follow-up of 23.5 months.
Keywords: Hip Dislocation; Ganz; Femoral Head Fracture; Acetabular Fractues
Introduction
The treatment of specific traumatic injuries to the hip and acetabulum in young adults represents a challenge for the orthopedic surgeon. In addition to the initial trauma, usually of high energy, there is the risk of secondary complications such as post-traumatic arthritis or avascular necrosis of the femoral head (AVN), among others, aggravated by the surgical trauma itself and also by the inherent difficulties in the treatment of these injuries. Based on previous anatomical studies, described in 2001 a technique of surgical hip dislocation with no case of AVN reported in their series [1,2]. Firstly conceived for the treatment of femoral-acetabular impingement, later its use was also expanded for traumatic injuries of the hip [3]. In this way, it became an ancillary tool for the treatment of selected patterns of joint fractures, allowing a more significant reach, including a 360-degree direct view of the femoral head's articular surface and acetabulum [4]. The main indications for its use in trauma are acetabular fractures [5-8]: high transverse or associated with fracture of the posterior wall, juxtatectal, "T" fractures, in addition to aged fractures [9] or simply when there is a need for better, direct control of the reduction. Other indications include: femoral head fractures [10-12], irreducible posterior dislocations13 or removal of intra-articular foreign bodies [14]. The objectives of this study are to evaluate the safety of Ganz's surgical dislocation concerning the consolidation of trochanteric osteotomy and the presence or absence of avascular necrosis of the femoral head in our initial series with this technique applied to the selected traumatic injuries of the hip.
Materials and Methods
From the hospital records and through the digital image file, all the first 10 cases treated at our service were identified and analyzed retrospectively. Ganz controlled dislocation was used to treat traumatic hip injuries. All cases were treated by the main author, between the years 2013 to 2015. Medical records and radiological images were evaluated.
For radiological analysis, the radiographic anteroposterior, alar, and obturator views were initially evaluated alongside the computed tomography studies to classify the lesions. In addition to the preoperative radiological images, records of surgical description and medical records were also considered for the characterization of lesions. Follow-up images were evaluated radiographically in anteroposterior and frog views. All postoperative images were scrutinized for radiographic signs of avascular necrosis of the femoral head or the greater trochanter's nonunion.
Surgical Technique
The technique described by Ganz2 consists of positioning in lateral decubitus, Gibson or Kocher-Langenbeck (KL) access, fasciotomy between the gluteus maximus muscles, and tensor fascia lata (Gibson) or divulsion of the gluteus maximus muscle (KL). KL access is used in the traditional way when posterior fixation to the wall or acetabular column is required. When this is not necessary, Gibson access is used. Next, the osteotomy line of the greater trochanter (GT) is identified, connecting the posterior edge of the vastus lateralis muscle with the posterior border of the trochanteric insertion of the middle gluteal muscle. In this stage, the GT can be pre-drilled to facilitate its fixation at the end of the procedure. The osteotomy is performed with a saw, leaving the trochanteric fragment with about 1 cm to 1.5 cm in its greatest thickness. In this way, the fragment is then elevated anteriorly, the capsular insertions are previously detached, while the lower limb is rotated laterally. A figure in "Z" capsulotomy is performed, with the anterior section of the capsulotomy towards the neck and the posterior section following the acetabular ridge, taking care not to injure the acetabular labrum. The ligament teres is sectioned, and the femoral head is elevated from the acetabulum (dislocation). The femoral head is perforated with a Kirschner wire or 2.0mm drill to ensure its viability (through the presence of active bleeding through the orifice). Maneuvers with the lower limb allow full exposure of the femoral head and the acetabulum's articular surface. The femoral head must be irrigated continuously with physiological saline to prevent chondral dryness. After the desired repair, the joint is reduced and the capsulotomy is sutured. The digastric osteotomy is fixed using two or three 3.5mm bi-cortical traction screws, directed to the calcar. The surgical wound is then closed in layers in the usual manner. We evaluated all patients radiologically for the healing of trochanteric osteotomy and the presence of NACF. The study was approved by the Research Ethics Committee of our institution and is registered on Plataforma Brasil.
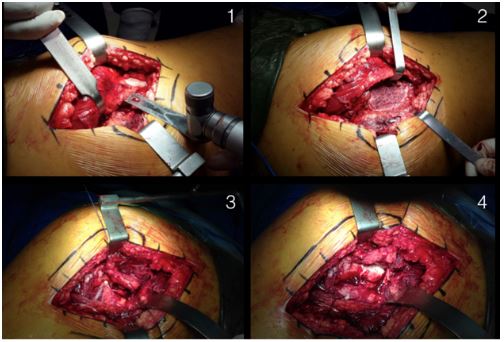
Figure1: Main steps of the surgical technique.

Figure 2: Hip Dislcation.
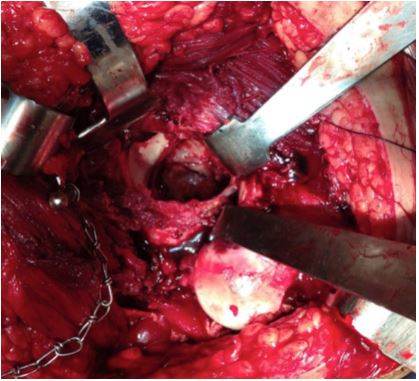
Figure 3: Acetabular exposure.
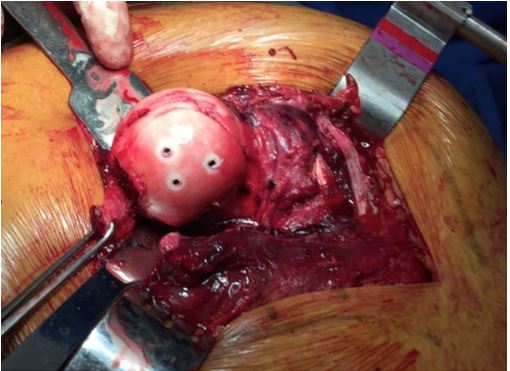
Figure 4: Femoral head exposure.
Results
Table 1 shows the complete description of the studied population. Of the ten patients who underwent this technique, all were male. Age ranged from 21 to 54 years, with an average of 37.2 years. Follow-up ranged from 12 to 37 months, with an average of 23.5 months. The main indication for the use of controlled dislocation was an acetabular fracture, in three cases, juxtatectal transverse fractures and one case associated with the posterior wall. Other indications were a "T" fracture in two cases, fractures of the femoral head in two cases (one associated with the posterior wall of the acetabulum), and two intra-articular firearm projectiles removal. All patients presented consolidation of the trochanteric osteotomy and absence of signs of NACF in the last follow-up, through radiographic evaluation.
Table 1: Cohort description.
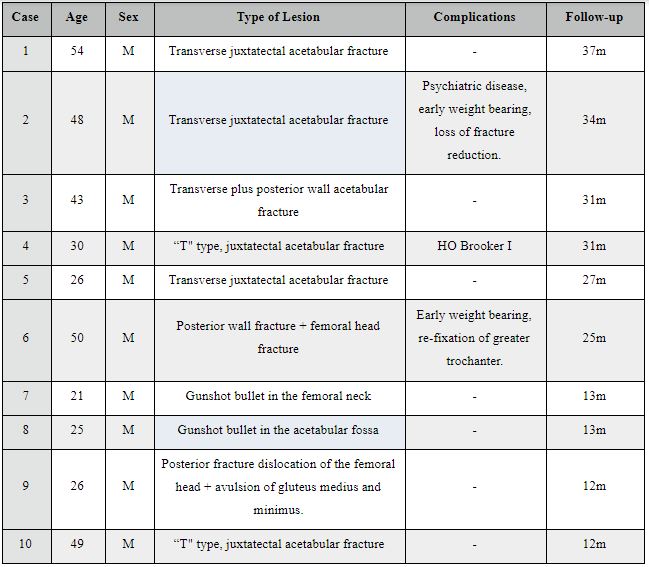
The complications observed were as follows: According to family members, case 2 had a history of psychiatric illness and walked without crutches at home since the first days after surgery due to a mental crisis for refusing to use his routine medications. He returned to the outpatient clinic thirty days after surgery, with loss of reduction of the acetabular fracture. Total hip arthroplasty was indicated after the control of the psychiatric condition and fracture healing. In definitive surgery, four months after the fracture, there was a regular extoscopic aspect of the femoral head medulla, which was then particulate and used as a graft. The trochanteric osteotomy was healed. It evolved satisfactorily after arthroplasty until the last follow-up. Case 4 presented Grade 1 heterotopic ossification, according to Brooker, without complaints or functional limitations. Case 6 presented the loosening of the trochanteric fixation in the week following the surgery. It was found that he was walking without crutches, jumping on the contralateral side. It was surgically reopened, and the osteotomy was re-fixed, using 4.5mm screws, evolving satisfactorily with GT consolidation and without NACF until the last follow-up.
The analysis of complications in cases 2 and 6 highlights the need for a meticulous preoperative selection. The lack of adherence to the postoperative protocol may have precipitated the need for reoperation. Case 9, with a diagnosis of irreducible posterior dislocation associated with a femoral head fracture, was referred to our service with five days of evolution. In the intraoperative period, the viability of the femoral head (bleeding) was verified. Total traumatic avulsion of the tendons of the gluteus medius and minimum of their insertions in the greater trochanter was also found reinserted to the footprint with titanium anchors at the end of the procedure. In this case, trochanteric osteotomy was not performed, given that the abductor system was no longer an obstacle due to its traumatic disinsertion, but the same technique of anterior "Z" arthrotomy and anterior dislocation was performed. This case was the subject of a case report by this team due to the rarity of the associated injuries.
Discussion
Ganz's technique, initially described for the treatment of femoral-acetabular impingement in 2001, with a series of 213 patients and a seven-year follow-up, proved the possibility of addressing the hip joint surface in its full range, without the risk of osteonecrosis [2-4].
The technique, initially developed to allow total joint access in elective cases, was later described for the treatment of acetabular fractures5-8 and femoral head.10-12 Siebenrock reported a series of 12 patients treated for traumatic pathologies with no evidence of NACF in a 35-month follow-up.3 Tannast published a series of 60 cases of acetabular fractures using controlled dislocation with no occurrence of NACF in eight years of follow-up.8 He also stressed the usefulness of intra-articular control in reducing and preventing intra-articular synthesis material. Haverkamp [9] demonstrated the utility of Ganz's dislocation for the treatment of acetabular pseudoarthrosis. According, the traumatic fracture-dislocation of the femoral head presented a better prognosis when treated using the Ganz technique, when compared to other accesses [12]. Keel et al. reached similar conclusions [13] Maqungoa [14] described firearm projectile removal cases using the Ganz technique with satisfactory results.
We had two possibly preventable complications (cases 2 and 6). The lack of adherence to postoperative care seems to have led to the need for a re-operation, but which did not present AVN and culminated in osteotomy healing. Case 4 showed grade 1 heterotopic calcification of Brooker, which was reported as the most frequent complication in this access, but without any clinical repercussions.
Conclusion
In our experience with Ganz controlled dislocation applied to trauma, there was clinical and radiographic consolidation of trochanteric osteotomy in all cases, and there was no episode of aseptic necrosis of the femoral head until the mean follow-up of 23.5 months.
Conflicts of Interest
The authors declare no conflicts of interest.
References:
- Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679-83.
- Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119-24.
- Siebenrock KA, Gautier E, Woo AK, Ganz R. Surgical dislocation of the femoral head for joint debridement and accurate reduction of fractures of the acetabulum. J Orthop Trauma, 2002;16(8):543-52.
- Jacob PJ, Sreeganesh K. Ganz safe surgical dislocation of hip: overview. Kerala J Orthop. 2013;26(2)107-9.
- Hadjicostas PT, Thielemann FW. The use of trochanteric slide osteotomy in the treatment of displaced acetabular fractures. Injury, 2008;39(8):907-13.
- Masse A, Aprato A, Rollero L, Bersano A, Ganz R. Surgical dislocation technique for the treatment of acetabular fractures. Clin Orthop Relat Res. 2013;471(12):4056-64.
- Naranje S, Shamshery P, Yadav CS, Gupta V, Nag HL. Digastric trochanteric flip osteotomy and surgical dislocation of hip in the management of acetabular fractures. Arch Orthop Trauma Surg. 2010;130(1):93-101.
- Tannast M, Krüger A, Mack PW, Powell JN, Hosalkar HS, Siebenrock KA. Surgical dislocation of the hip for the fixation of acetabular fractures. J Bone Joint Surg Br. 2010;92(6):842-52.
- Haverkamp D, Luitse JS, Eijer H. Acetabular reduction osteotomy using surgical dislocation of the hip joint for treatment of a malunited acetabular fracture. Arch Orthop Trauma Surg. 2004;124(8):527-30.
- Henle P, Kloen P, Siebenrock KA. Femoral head injuries: Which treatment strategy can be recommended? Injury. 2007;38(4):478-88.
- Gardner MJ, Suk M, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19(5):334-42.
- Ozcan M, Copuroğlu C, Sarıdoğan K. Fractures of the femoral head: what are the reasons for poor outcome? Ulus Travma Acil Cerrahi Derg. 2011;17(1):51-6.
- Keel MJ, Bastian JD, Büchler L, Siebenrock KA. Surgical dislocation of the hip for a locked traumatic posterior dislocation with associated femoral neck and acetabular fractures. J Bone Joint Surg Br. 2010;92(3):442-6.
- Maqungoa S, Hoppea S, Kautaa JN, McColluma GA, Laubschera M, Helda M, et al. Surgical hip dislocation for removal of retained intra-articular bullets. Injury. 2016;47(10):2218-22.

