Presentation of a Clinical Case: Improvement Of Diffuse Axonal Injury and Sinking Flap Syndrome Post-Craneoplasty
Raul Fernando VD1, Maria Sofia VL2, Teresita De JLV3 and Gabriel MN4*
1Department of Neurosurgery Service, Guadalajara Regional Military Hospital of Specialties, Mexico
2Undergraduate intern, Guadalajara Regional Military Hospital of Specialties, Mexico
3Department of Surgery, Guadalajara Regional Military Hospital of Specialties, Mexico
4Department of Neurology, Guadalajara Regional Military Hospital, Mexico
Received Date: 01/08/2020; Published Date: 24/08/2020
*Corresponding author: Gabriel Miranda Nava, Department of Neurology, Hospital Center of the Presidential General Staff, Master’s in Public Health, Doctor in Administration and Public Policies, Mexico. E-mail: drgabrielmiranda@hotmail.com
Abstract
The syndrome of the trephined, craniectomized or sunken flap syndrome is commonly referred as neurological manifestations associated to skin flap depression and reversible after craneoplasty, which allows its differentiation from post-traumatic syndrome. We present the case of a male patient, 35 years old, with history of de-compressive craniectomy. He evolved with sudden neurological worsening associated to syndrome of the trephined and recovery after craneoplasty. Physiopathology of the syndrome involves cerebrovascular, metabolic and cerebrospinal fluid hydrodynamic disturbances as well as parenchymal hyperdynamic mechanisms.
Keywords: Síndrome Suken Flap; Decompressive Craniectomy; Difuse Axonal Injury
Introduction
Traumatic brain injury (TBI), according to the National Head Injury Foundation, is defined as "damage to the brain, of a non-degenerative nature, caused by an external force, which can produce a decrease or alteration of the state of consciousness, resulting in a impaired functioning of cognitive and physical abilities ". The damage occurs mainly in physical and cognitive capacities, such as attention, perception, memory, problem solving, understanding, among others. The most common causes of a TBI are accidents at work, at home, outdoors, or while playing sports; as well as falls, physical assaults and traffic accidents. The latter, with the highest incidence, in 42% of the cases [1].
In Mexico, it is the third cause of death with an index of 38.8 per 100,000 inhabitants and with the highest incidence in men between 15 and 45 years of age [2]. The TBI classification is carried out taking into account the level of consciousness measured according to the “Glasgow Coma Scale” (GCS). The GSC assesses three types of response independently: ocular, verbal and motor. A patient is considered to be in a coma when the score resulting from the sum of the different responses is less than 9 [3].
Based on this scale we differentiate:
- Mild TBI: GCS 15-14
- Moderate TBI: GCS 13-9
- Severe TBI: GCS <9
Mild TBI: It is the most frequent, there is usually no loss of consciousness or if there is, its duration is usually limited to the minutes after the contusion.
Moderate TBI: The period of loss of consciousness is greater than 30 minutes but does not exceed one day and the period in which the patient who suffers from it has difficulty learning new information is less than one week.
Severe TBI: In this type of trauma, the period of loss of consciousness is greater than one day and / or the period in which the patient who suffers it has difficulties learning new information is greater than one week [4]. TBI can be divided into penetrating and non-penetrating injuries, the latter in turn being subdivided into focal or diffuse injuries (Figure 1) [5].
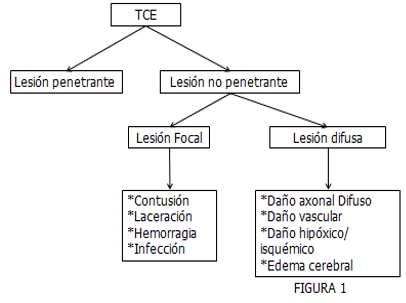
The focal injury includes: contusions, which usually affect the cerebral cortex and are caused by a direct mechanism against the impact area, or by an indirect one, which by backlash affects the opposite side of the trauma, the most frequent locations are the frontal lobes and temporary. Lacerations occur when the injury is so severe that it involves the leptomeninges. Bleeding can develop after a period of time and spread into the subarachnoid space, forming bruises. Local infections are complications from contamination, generally bacterial [6,7].
Diffuse Axonal Injury
Diffuse injury includes Diffuse Axonal Damage (DAD), diffuse vascular damage (DVD), and diffuse hypoxia / ischemia. DVD is caused by stress and traction on the capillaries of the brain parenchyma resulting in parenchymal hemorrhages. Diffuse hypoxic / ischemic damage sometimes accompanies TBI, especially in patients with intracranial hypertension [1,4]. DAD is caused by inertial, angular, or rotational forces (acceleration-deceleration) that cause rapid movement of the skull which deforms white matter, the axonal damage pattern is described as multifocal, appears deep in subcortical white matter and is particularly common in midline structures, including the corpus callosum [5].
The brain is relatively flexible when it is subjected to the effect of slow inertia, as it adapts to change and recovers its original physical state without being damaged; however, when this effect occurs very quickly, less than 50 milliseconds, the white matter deforms considerably. Thus, factors such as the magnitude, location, duration, direction, and velocity of the force determine the severity of axonal damage [2,5]. Axonal damage can be caused by an immediate axotomy (primary injury), which damages the structural elements of the axons, such as microtubules, and by a delayed action after minutes or hours after impact (secondary injury), in which the injury axonal is a response to the cellular cascade [5,6].
The trauma induces focal permeability of the axolemum, which increases the entry of calcium and this generates the activation of proteases, calpains and caspases, which cause the degradation of the axon cytoskeleton and its disconnection.Sunken flap síndrome. Sunken flap syndrome corresponds to a complication of decompressive craniectomy. The pathophysiology of the syndrome is believed to be multifactorial, including hydrodynamic alterations of the cerebrospinal fluid (CSF), changes in cerebral metabolism and blood flow, pressure exerted by the atmospheric gradient and movements of the parenchyma [8]. Under normal conditions a The individual in the supine position presents a CSF pressure of 15cm H2O and in an upright position a pressure of 0 at the level of the cisterna magna and –8 cm H2O in the ventricles. This negative pressure in a craniectomized patient generates a vacuum or suction effect that is added to the positive atmospheric pressure in the opposite direction, favoring the depression of the skin flap and the underlying brain tissue. Likewise, this subsidence causes collapse of the subarachnoid space, contributing to the alteration of the normal dynamics of the CSF [9].
In craniectomized subjects, there is both a decrease in arterial flow and a decrease in venous return. The former occurs as a consequence of the increase in vascular resistance secondary to the transmission of atmospheric pressure to the cerebral blood vessels, as well as due to their distortion by deviation of the midline structures. Venous return, for its part, is affected by focal cerebral compression at the site of subsidence. Both phenomena contribute to the decrease in pulsatility of the sunken brain and to the vacuum effect on the flap. An immediate consequence of these changes corresponds to the failure of cerebral circulatory autoregulation, a mechanism by which the presentation of reperfusion injuries after cranioplasty is explained [10].
Different authors propose that flow velocities (measured by transcranial Doppler) increase in the ipsilateral and contralateral middle cerebral and internal carotid arteries when restoring the bone defect in craniectomized patients, particularly when this gesture is performed. carried out early. Furthermore, it is observed that the flow velocities of the damaged hemispheres in craniectomized patients tend to decrease with postural changes (sitting or standing), reversing this situation with cranioplasty [11].
Description of the Clinical Case
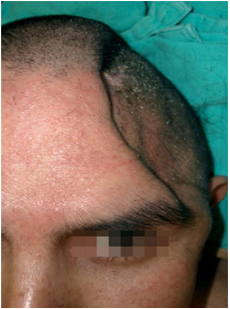
35-year-old male, with no significant personal pathological history; suffered a run over accident three years ago with severe head trauma and loss of alertness. During the initial evaluation in the hospital, a CT scan is performed showing the presence of an acute subdural hematoma in the left frontotemporal region and severe cerebral edema, in addition to presenting data of intracranial hypertension, a decompressive left frontotemporoparietal craniectomy is performed plus drainage of subdural hematoma acute frontotemporal plus partial temporal lobectomy and loose dura mater plasty with pericranium. After the surgical procedure, he showed a notable improvement in the frontal syndrome, in addition to behavioral alterations secondary to the lesion of the frontal lobes, ability to speak without alterations, quadriparesis, limitation of movements in upper and lower extremities, sensitivity to touch and symmetrical nocioseptive stimuli. coordination and gait absent. His discharge is decided, however at 3 months he presented a neurological deficit and the ability to speak was symbolically degraded, it was only limited to words such as "yes" and "no", to the abnormal skull physical examination, with a scar in the frontotemporoparietal region Neurologically conscious with post-traumatic dementia, poor speech, quadriparesis due to diffuse axonal damage, position with limbs in flexion due to ankylosis and contractures, coordination and impaired gait. As part of the treatment, a right frontotemporal cranioplasty was decided. After the procedure, he was oriented in time, place and person, performed movements of the lower and upper extremities without pain. Due to the health contingency due to SARS COVID-19, a second cranioplasty in the left frontotemporal region is awaiting.
Discussion
In Mexico, death from trauma continues to be among the main causes of death and disability, and injuries to the nervous system and hemorrhagic shock are its main contributors. Severe head injury is a cause of mortality and disability in the young injured patient. The polytrauma patient with sequelae of head trauma constitutes a complex group of patients who may present with different types of brain injury, including diffuse axonal damage. We know that most head injuries occur in previously healthy people in general terms and unfortunately, also a large number of patients are left with a disability or subsequent sequela, which affects their neurological and intellectual capacities or leads to economic and family imbalances sexual or emotional [12].
Despite current technological advances, there is still a very high mortality According to data from the Revista Mexicana de Neurosciencia “worldwide, 1.2 million people die annually from Cranioencephalic Trauma (TBI) and between 20 and 50 million suffer non-traumatic injuries mortal [13]”.
That is why the immediate initial treatment is essential within the first hour since it will modify the prognosis of the patients. It is important to identify the symptoms of intracranial hypertension so as not to delay surgical treatment, although we do not know the time that passed between the impact and medical care, it is an ethical and moral duty of health institutions to have the personnel and technological implements to be able to apply them in a timely manner, it is clear that there was a failure in the decision-making of the definitive treatment [14,15]. The diffuse axonal damage triggered a significant cognitive and functional deterioration during the first days after the TBI, the patient showed quadriparesis as a sequela but was neurologically stable in addition to maintaining a fluent conversation, however, three months later there was a significant decrease in speech and neurological status, evidencing apart from axonal damage. Diffuse sunken flap syndrome, which corresponds to a complication of decompressive craniectomy, its clinical spectrum is variable, triggering vague and nonspecific manifestations until sudden neurological deterioration in most cases, as our patient clinically manifested. Although its incidence is unknown with certainty, it acquires importance not only because it is underdiagnosed, but also because of the possibility of reversing the symptoms with correct treatment [16]. The cornerstone of treatment is given by the surgical repair of the defect, for which more weighty studies are required to determine the appropriate surgical time. After the cranioplasty, a notable improvement was shown in the patient, his speech was a little more fluent and he can hold a conversation for more than 7 minutes, without diverting the subject, an increase in the mobility of the lower and upper extremities was also observed [13,14,15].
Conclusion
Cranioencephalic trauma requires aggressive emergency treatment, in order to prevent or minimize irreversible damage to the nervous system, for which it is necessary to adopt a decided and organized approach that ensures optimal patient care from the initial management and during the following bases of diagnosis and definitive treatment. One case is not enough to reach definitive conclusions about the best approach to a TCS. Traumatic axonal injury is undoubtedly the most frequent variety of head trauma that predominantly affects young men and is the cause of significant disability. Prevention of traumatic brain injury is the most important pillar in medical care followed by neurointensive care guided by neuromonitoring [17,18]. Every physician must have a good knowledge of the mechanisms of head trauma that trigger alterations whose anatomical and physiological impact can be profound and potentially fatal for the patient due to the sequelae and complications that this entails. It is important to emphasize that the sequelae and complications that occur after TBI will depend, to a large extent, on the good, fast and efficient management assigned to the patient from the moment the head injury begins. Based on the foregoing, it must be concluded that patients suffering from ADD post TBI should be evaluated early to carry out the correct therapeutic measures and thus reduce neurological sequelae. In addition to taking strict care in post-operative decompressive craniectomy patients once they have been discharged from the hospital in order to avoid sunken flap syndrome. Also no less important is the prevention of motor vehicle accidents, emphasizing motorcycle drivers wearing helmets, in addition to placing important emphasis on promoting road safety measures among the population.
Acknowledgements
This research work was carried out under the supervision of the TTE. COR. MC Raúl Fernando Viera Dorame, to whom I express my deep gratitude, for his dedication, patience and time he had to carry out this clinical case and also not least to the Regional Military Hospital of Guadalajara, for the opportunity to exercise my year of internship and allow my abilities and knowledge to be exploited.
References:
- Curry P, Friday D, Sharma D. Perioperative management of traumatic brain injury. International Journal of critical illness and injury science. 2015;1:27-35.
- National Institute of Statistics and Geography. Mortality. [Internet] [Cited 2018 Sept 23]. Available at: www.beta.inegi.org.mx/temas/mortalidad/.
- Gilli Miner M, Murillo Cabezas F, Perrea Milla E, In Martínez Navarro F, Antó JM, Casttellanos PL, et al. Epidemiology and prevention of head injuries.Public Health. Madrid: Mc-Graw Hill Interamericana. 1998;614-631.
- Luque Fernández M. Boscá Crespo A. Cranioencephalic Trauma. University Clinical Hospital of Malaga. Viewed at: http://www.medynet.com/usuarios/jraguilar/Manual%20de%20urgencias%20y%20Emergencias/traucra.pdf.
- Casas FC. Head trauma. Therapeutic Diagnostic Protocols of the AEP: Pediatric Neurology. 2018;118:118-127.
- Levine JM, Kumar MA. Traumatic Brain Injury. Neurocritical Care Society Practice Update. 2013.
- Villareal-Reyna G. Diffuse axonal injury, contusion and brain stem damage. Available from: http://www.neurocirugiaendovascular.com.
- Patel HC, Menon DK, Tebbs S, Hawker R, Hutchinson PJ, Kirkpatrick PJ. Specialist neurocritical care and outcome from head injury. Intensive Care Med. 2012;28:547-53.
- Vareles PN, Eastwood D, Yun HJ, Spanaki MU, Bey LH, Kessaris C, et al. Impact of a neurointensivist on outcome in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 2016;104:713-9.
- Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: An international observational study. Crit Care Med. 2017;35:1815-20.
- Bratton SL, Chestnut RM, Ghajar J, Hammond FFM, Harris OA, Hartl R, et al. Anesthetics, analgesics and sedatives. J Neurotrauma. 2017;24(1):S71-6.
- Cruz BL y col. Estrategias de diagnóstico y tratamiento para el manejo del traumatismo craneoencefálico en adultos. Trauma. 2017;10:46-57.
- Abadal-Centellas JM, Llompart-Pou JA, Homar-Ramirez J, Pérez-Bárcena J, Roselló-Ferrer A, Ibañez-Juvé J. Neurologic outcome of posttraumatic for refractory intracranial hypertension treated with external lumbar drainage. J Trauma. 2012; 62:282-6.
- Smith DH, Hicks R, Povlishock JT. Therapy Development for Diffuse Axonal Injury. J Neurotrauma. 2013;30:307-323
- Werner C, Engelhard K. Pathophysiology of traumatic injury. Br J Anaesth. 2016.
- Tintinalli JE y cols. Medicina de Urgencias Tomo II, 8a. edición. Ed. Mc Graw-Hill Interamericana. 2018:CAP:257.
- Reddy S, Khalifian S, Flores JM, et al. Clinical outcomes in craneoplasty: Risk factors and choice of reconstructive material. Plast Reconstr Surg. 2014;133(4):864-873.
- Baumeister S, Peek A, Friedman A, et al. Management of postneurosurgical bone flap loss caused by infection. Plast. Reconstr. Surg. 2008;122 (6):195e-208e.

