Chronic Intracranial Subdural Hematoma Case Report and Review of the Literature
Raul Fernando VD1, Maria Sofia VL2, Teresita De JLV3 and Gabriel MN4,*
1Department of Neurosurgery Service, Guadalajara Regional Military Hospital of Specialties, Mexico
2Undergraduate intern, Guadalajara Regional Military Hospital of Specialties, Mexico
3Department of Surgery, Guadalajara Regional Military Hospital of Specialties, Mexico
4Department of Neurology, Guadalajara Regional Military Hospital, Mexico
Received Date: 04/08/2020; Published Date: 20/08/2020
*Corresponding author: Gabriel Miranda Nava, Department of Neurology, Hospital Center of the Presidential General Staff, Master’s in Public Health, Doctor in Administration and Public policies, Mexico. E-mail: drgabrielmiranda@hotmail.com
Abstract
Chronic subdural hematoma is a common condition, the frequency of which is further increased due to an aging population and the more frequent use of antithrombotic medications. The case report of an 85-year-old female patient with chronic intracranial subdural hematoma, without a history of previous trauma, is presented. The patient started with insidious delay; Computed tomography performed makes the correct diagnosis of chronic subdural hematoma. The diagnostic suspicion of subdural hematomas in geriatric patients is essential since the symptoms are masked with nonspecific symptoms associated with hydro-electrolyte imbalances that are almost always the first diagnostic suspicion in this type of patient.
Keywords: Chronic Subdural Hematoma; Geriatric Patients; Antithrombotic Drugs; Diagnostic Suspicion
Introduction
Chronic subdural hematoma is a common condition, the frequency of which is further increasing due to the aging of the population and the more frequent use of antithrombotic medications. It leads to nonspecific symptoms and neurological deficits and is usually treated surgically [1]. It remains a major neurosurgical problem and the number of patients is increasing despite progress in the early diagnosis of brain injuries [4]. Chronic subdural hematoma is the most common of hematomas in patients over 65 years of age who have suffered head trauma. The incidence for this age group is 1-58 / 100,000. Parenchymal atrophy of the brain occurs over the years. The subdural area expands with the parenchyma causing atrophy, thus the space between the bridging veins and the subdural space becomes fragile [3]. Subdural hematoma is caused by bleeding from the bridging veins, causing blood to accumulate between the dura mater and the arachnoid, or also by bleeding from the cortical vessels. For this reason, bleeding can occur even after minor head trauma, and patients insidiously begin to show symptoms several days or even weeks after bleeding begins. Chronic subdural hematoma is common in elderly patients after minimal trauma or when they are receiving anticoagulant therapy; People with bleeding disorders, congenital or acquired, can also suffer from a subdural hematoma, acute or chronic [5]. In a study that analyzed 700 consecutive patients with a diagnosis of chronic subdural hematoma, all patients underwent computed tomography (CT) studies and were operated on by craniotomy or holes with a closed system drainage technique, more than 50% had bleeding intracranial extensive, almost half of the patients were treated with oral anticoagulants. Patients with extensive fresh bleeding were in significantly worse condition upon admission and were treated with craniotomy and external capsulectomy (42%). All the others had a closed subdural space drainage system. Treatment results were acceptable, 2% died and 1.5% remained vegetative, due to massive hemorrhage and serious neurological deficits on admission [4].
Description of the Clinical Case
An 85-year-old female patient with a history of long-standing systemic arterial hypertension without treatment, long-standing hypothyroidism treated with levothyroxine 50mg per day and a history of lumbar hernia managed with analgesics, including acetylsalicylic acid. He went to the emergency room due to hallucinations, loss of balance, headache, bradypsychia, and 24-hour retrograde amnesia. One week before, he reported the presence of disorientation in time and space, in addition to bilateral hearing loss and impaired ambulation. On physical examination, he presented right unilateral mydriasis and a Glasgow score of 13, and at 24 hours of hospitalization neurological deterioration at Glasgow 11. Due to these nonspecific symptoms and laboratory results: Serum electrolytes: sodium: 129, potassium: 3.4, chlorine: 100. Differential diagnoses of hyponatremia, decompensated hypothyroidism, and mixed structural-metabolic encephalopathy are made. The neurosurgery service is consulted and requests a CT scan. CT showed an image attributable to a hypodense chronic subdural hematoma of the left hemisphere (Figure 1 and 2).

Figure 1: Hematoma subdural chronic hypodense.
A heterogeneous hypodense lesion with irregular borders is observed, producing a mass effect with effacement of sulci and fissures in the left hemisphere, with collapse of the left ventricular system and displacement of midline structures of more than 1 centimeter.
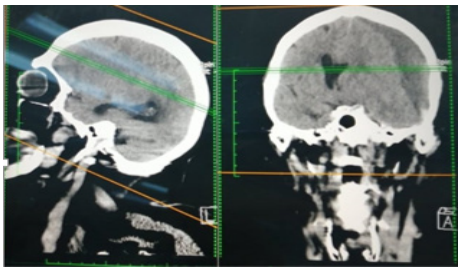
Figure 2: Hematoma subdural chronic hypodense in short coronal and sagittal.
Treatment
The day after the CT scan, a craniotomy was performed with drainage of the chronic subdural hematoma due to an enlarged trepan, in the left temporal dorsal hump, performing a single enlarged trepan measuring 1.8 cm in diameter, with a pneumatic motor, and a lavage technique with 5 litres of warm saline solution, applying this solution until the total resolution of the clot, in the postoperative period presenting significant improvement of the neurological deficit. Follow-up was continued one month later in the neurosurgery outpatient clinic, with a control CT scan in which minimal residual subdural collection was observed, and no image suggestive of a mass effect was observed. Currently a patient with no neurological deficit on the control CT scan, a scarce residual hygroma can be observed (Figure 3).

Figure 3: Simple skull CT scan one month after surgery.
Discussion
Subdural hematoma is a common entity in geriatric patients that has been associated with multiple causes: traumatic and non-traumatic. The symptoms are uncharacteristic and variable. The wide use of oral anticoagulants, especially in older populations, increases the number of spontaneous intracranial hemorrhages, both intracerebral and subdural (two). Despite progress in diagnosis, subdural hematoma remains a common cause of serious intracranial complications. The increasing number of cases of this lesion is strictly related to a wide use of oral anticoagulants [4].
Conclusion
The diagnostic suspicion of subdural hematomas in geriatric patients is essential since the symptoms are masked by nonspecific symptoms associated with fluid and electrolyte imbalances, which are almost always the first diagnostic suspicion in this type of patient. These symptoms are easily masked due to the cortical atrophy that can occur in this age group that allows the slow progression of this pathology, due to this the diagnosis can be difficult if there is no adequate diagnostic suspicion. Surgical removal remains the best type of treatment for such injuries.
Conflicts of Interest: The author declares no conflicts of interest during the planning, execution of the research and the preparation of the article for publication.
References:
- Juratli TA and Klein G. Schackert “Das chronische subduralhamatom im alter”. Der chirurg, 2017;88(2):131-135.
- Kotwica Z, Brzeziński J. Intracerebral hematoma as the complication of the surgical removal of chronic subdural hematoma. Case report. Neurol Psychiatr (Bucur). 1989;27:1679.
- Albayrak S, Burak Atçı İ, Üçler Necati, Yılmaz, H & Kaplan Metin. Evaluation of awake burr hole drainage for chronic subdural hematoma in geriatric patients: a retrospective analysis of 3 years. Cukurova Medical Journal. 2016;41(1):69-73.
- Kotwica Z, Saracen A & Dziuba I. Chronic Subdural Hematoma (CSH) Is Still an Important Clinical Problem. Analysis of 700 Consecutive Patients. Translational neurosciense. 2019.
- Pérez Rodríguez RM, Cairo Sáez G & Rodríguez Monteagudo, JL. Hematoma subdural crónico sin evidencia de trauma previo. Revista científica Villa Clara. 2018.

