An Exploration on the Location Evaluation of Umbilical Venous Catheter: Based on a Case Report of Pleural Effusion Associated with a Properly Placed Umbilical Venous Catheter and Literatures
Yuanqing Z1*
1Department of Neonatal Intensive Care Unit, Women’ s Hospital, Zhejiang University School of Medicine, Hangzhou, ZhejiangProvince 310006, China
Received Date: 01/08/2020; Published Date: 14/08/2020
*Corresponding author: Yuanqing Zhu, Department of Neonatal Intensive Care Unit, Women’s Hospital, Zhejiang University School of Medicine, Xueshi Road 1, Hangzhou, Zhejiang, Province 310006, Peoples R China. Tel: 86 15957146842; E-mail: yuanqing_2005@163.com
Abstract
A case of pleural effusion with parenteral nutrition solution associated with a UVC that appeared to be positioned appropriately in the inferior vena cava happened in our NICU. The infant’s respiratory status deteriorated. Endotracheal intubated mechanical ventilation was applied. After the UVC was moved, the infant’s respiratory status became stable. Pleural effusion following properly placed UVC is rare but serious. The mechanism of generating has been still a problem. Injury of IVC (inferior vena cana) by UVC may have good prognosis in very low birth weight infants (VLBWI) as long as UVC is removed in proper time. Re-evaluating position of UVC after insertion is necessary.
Keywords: Pleural Effusion; Umbilical Venous Catheter; UVC; Inferior Vena Cava; Very Low Birth Weight
Introduction
Umbilical venous catheters (UVCs) are commonly used in the treatment of preterm low weight infants or ill neonates. Serious complications [1] from UVC placement includes infection [2], thrombosis [3], hemorrhage, pericardial effusion [3] and cardiac arrhythmias [4] etc. Pleural effusion is a rare complication of a properly placed Umbilical Venous Catheter (UVC) [5,6]. No one has explored the function of procedure of placement and evaluation [5,6]. In this paper, we explored the reason of pleural effusion occurrence relating with the procedure of placing UVC and position evaluation based on this case and literatures.
Case Report
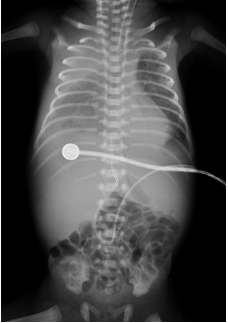
A permission to report this patient was gained from the mother. A 28 4/7weeks gestation preterm female infant was delivered to a 26-year-old gravida 1 mother via spontaneous vaginal vertex delivery with a birth weight of 1190 g. Apgar scores were 9 and 10 at 1 and 5 minutes, respectively. Treatment at delivery included reposition airway, suction and keeping warm. The infant was placed on NCPAP ventilation. FIO2% is 21%. A single lumen UVC (ombilicath, prodimed, 6, rue Louis Armand LE NPLESSIS BOUCHARD, Tel: 33(0)134441515 fax:33(0)130722208) were placed at the first 24 hours of life. Anteroposterior (AP) chest radiograph showed the UVC tip was high in the right atrium (Fig. 1). The UVC was withdrawn 1.5cm. No fluids were infused through the catheter prior to checking the UVC position. TPN and intravenous lipid emulsion were infused at 80mL/kg/day on the first day through the UVC, added by 10ml/kg/day. Initial arterial blood gas showed a pH of 7.293, PaCO2 of 44.3 mmHg, PaO2 of 72.9 mmHg and base deficit –5.57 mmol/l; complete blood count was within normal limits. At 24 hours of life, an echocardiogram showed a moderate-size PDA 1.3mm and the UVC to be in the terminal IVC, prior to its entry into the right atrium. During the first 79 hours of life, that is, during the first 3 days after UVC operation, the infant’s respiratory status was stable on the NCPAP, with the oxygen requirement 21%. At 79 hours of life, the oxygen requirement rose to 25%, then 60%, then 80% and the SpO2 was not stable and not normal still. Apnea happened frequently and it is not easy to recover. So the respiratory sustaining mode of this infant was switched to synchronized intermittent positive pressure ventilation (SlPPV) due to the unstable respiratory status, with a PIP of 20cm H2O, PEEP 5cm H2O, RR 55bp and 25% oxygen. A routine arterial blood gas showed a pH of 7.08, PaCO2 of 69.6 mm Hg, PaO2 of 56.8mmHg, and a base deficit of –10.93 mEq/L. A stat chest radiograph showed right pleural effusion (Figure 2).
The UVC were in good position but in a lower position than before. The infant was switched to high-frequency oscillatory ventilation (HFOV) due to the high PaCO2, with a mean airway pressure of 10cm H2O, amplitude of 2, frequency of 12 Hz, and 25% oxygen. The UVC was suspected related with the sudden deterioration of the disease and was removed at 88 hours of age. A stat ultrasound of the chest showed a large pleural effusion on both sides of the chest, and no pericardial effusion. Ultrasound-guided thoracentesis was performed on the both sides of the chest, and a totally 70mL of milky blood-tinged pleural fluid was withdrawn. Pleural fluid analysis showed a pH of 7.49, glucose of 974 mg/dl, sodium of 132mEq/L, potassium of 4.6mEq/l, chloride of 104 mEq/l; red blood cell count of 15,000/mm , nucleated cells of 12.7/mm ,39% segmented neutrophils, 37% lymphocytes, and 23% monocytes. A repeat chest radiograph showed resolution of the pleural effusion at 94 hours of age (6 hours after thoracentesis). Arterial blood gas after thoracentesis showed a pH of 7.337, PaCO2 of 45.9mm Hg, PaO2 of 61.3mmHg, bicarbonate of 22.6mEq/L, and a base deficit of –1.74 mEq/L. The infant remained stable on the HFOV with an oxygen requirement of 21%, later transferred to SIMV over the next few days with an oxygen requirement of 25%-35% and was extubated at 192 hours. No further pleural effusion was noted.
Discussion
From the stretching way of the umbilical vein in anatomy,we could speculate that the pleural cavity may be in contact with the inserted umbilical vein in the vicinity of the heart, which is the possibility of causing anatomical damage [5]. We presume that during the procedure of placement, UVC traversed the inferior vena cava and penetrated into the right pleural space, resulting in extravasation of TPN fluid and thus in a right-sided pleural effusion. The drainage in this case was mixed with blood which was from IVC. Penetrating injury to the inferior vena cava in infants did not cause uncontrolled continuing hemorrhage but did in older children [7] and adults [8], which carry a high mortality rate, ranging up to around 65%[8]. The relatively lower CVP (Central Venous Pressure) in VLBWI (very low birth weight infants) probably protects them from hemorrhage. Pubmed (1964–2019) was searched using the terms: ‘infant, newborn’ AND ‘inferior vena cava injury’ in September 2019, yielding no relevant results of inferior vena cava injury in VLBWL.
During the umbilical vein catheterization process, whether or not there is resistance, the movement should be gentle to avoid potential vascular and organs damage. The blood vessels of pre-term infants are particularly fragile, which is easier to be damaged. Confirming the position through the chest radiograph, although simple and feasible, is inaccurate, prone to be too low or too high [5]. Prenatal B-mode ultrasonic diagnose is necessary to be done to eliminate some abnormal shapes and some anatomical deformities [10,11].
After UVCs are completed, B-mode ultrasound diagnostic has been considered to be more accurate to locate the position [9,12]. However, for some health-care institutions in underdeveloped areas, B-mode ultrasound equipment and technology is too difficult to acquire.
And during the follow-up period, rechecking the position of UVC is still necessary as observed most of the tips of catheters will move higher as umbilical cords shrink though catheters’ calibrations outside do not change if they were rechecked the next day after insertion (Table 1).
Although the frequency of pleural effusion following properly placed UVC is exceedingly rare, these reports [5,13] suggest that further close observations and checks still should be maintained for the development of any complications though UVC has been properly placed.
Disclosure Statement
The author declares that there is no conflict of interest.
References:
- Mutlu M, Aslan Y, Kul S, et al. Umbilical venous catheter complications in newborns: a 6-year single-center experience[J]. J Matern-Fetal Neo M. 2016;29(17):2817-2822.
- Ming-Yan H, Xiao-Chun Z, Xiang-Yu G, et al. Catheter-related infection and pathogens of umbilical venous catheterization in a neonatal intensive care unit in China[J]. Am J Perinat. 2012;29(02):107-114.
- Sehgal A, Cook V, Dunn M. Pericardial effusion associated with an appropriately placed umbilical venous catheter[J]. J Perinatol. 2007;27(5):317-319.
- Verheij G, Smits-Wintjens V, Rozendaal L, et al. Cardiac arrhythmias associated with umbilical venous catheterisation in neonates[J]. Bmj Case Rep. 2008;2009(2009):r4-r2009.
- Pabalan MJ, Wynn RJ, Reynolds AM, et al. Pleural effusion with parenteral nutrition solution: an unusual complication of an "appropriately" placed umbilical venous catheter [J]. Amer J Perinatol. 2007;24(10):581-585.
- Unal S, Arifoglu İ, Çelik İH, et al. Pleural and Pericardiac Effusion as a Complication of Properly Placed Umbilical Venous Catheter [J]. Journal of Neonatal Surgery. 2017;6(2):34.
- Jan WA, Samad A, Anwar R. Mortality and morbidity of abdominal inferior vena-caval injuries [J]. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP. 2004;14(10):622.
- Rooyen PLV, Karusseit VOL, Mokoena T. Inferior vena cava injuries: a case series and review of the South African experience[J]. Injury. 2015;46(1):71-75.
- Michel F, Brevautmalaty V, Pasquali R, et al. Comparison of ultrasound and X-ray in determining the position of umbilical venous catheters.[J]. Resuscitation. 2012;83(6):705-709.
- Raisanen P, Cassel I, Martin G, et al. Umbilical venous catheter complication in an infant with left-sided congenital diaphragmatic hernia: extravasation owing to hepatic vein catheterization[J]. J Pediatr Surg. 2010;45(12):e33-e35.
- Hofstaetter C, H-G B, Isaksen C, et al. Abnormal umbilical-portal-hepatic venous system in two siblings: a sign for congenital cholangiodysplasia[J]. Ultrasound Obst Gyn. 2010;26(5):571-573.
- Greenberg M, Movahed H, Peterson B, et al. Placement of umbilical venous catheters with use of bedside real-time ultrasonography [J]. J Pediatr. 1995;126(4):633-635.
- Unal S, Arifoglu İ, Çelik İH, et al. Pleural and Pericardiac Effusion as a Complication of Properly Placed Umbilical Venous Catheter [J]. Journal of Neonatal Surgery. 2017;6(2):34.

