Café Au Lait Spot is Marker for Pheochromocytoma in Hypertensive Crisis With a Wide-Differential Diagnosis: A Case Report
Elsayed YMH*
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
Received Date: 16/07/2020; Published Date: 10/08/2020
*Corresponding author:Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt. E-mail: dryaser24@yahoo.com
Abstract
Rationale: Hypertensive crisis is a serious cardiovascular problem. Refractory and resistant severe hypertension is sometimes needed urgent clinical diagnostic assessment for the cause. Hypertensive crisis due to pheochromocytoma is a rare problem but have an association with both café au lait spots, and axillary freckling, and neurofibromatosis. The correlation among hypertensive crisis, café au lait spots, neurofibromatosis, and presence of pheochromocytoma is highly significant. Cafe au lait spots by themselves are not a harm lesion. The presence of café au lait spots may be helping in the arrival to cause of hypertensive crisis.
Patient concerns: A middle-aged male patient presented to the emergency room with hypertensive crisis due to suspected pheochromocytoma.
Diagnosis: Hypertensive crisis due to suspected pheochromocytoma.
Interventions: Electrocardiography and intravenous nitroglycerin infusion
Outcomes: Dramatic clinical improvement and blood pressure controlling within 15 minutes of labetalol oral tablet had happened.
Lessons: Café au lait Spot is a marker for pheochromocytoma in hypertensive crisis but with a wide-differential diagnosis. Labetalol may be chosen in hypertensive crisis due to pheochromocytoma.
Keywords: Café Au Lait; A marker for Pheochromocytoma; Hypertensive crisis; Neurofibromatosis
Abbreviations: CALS: Café au lait spots; NIH: National Institutes of Health; NF1: Neurofibromatosis
Introduction
Café au lait spot (CALS) are prescribed as a birthmark with flat pigmented surface and irregular border [1,2]. CALS are caused by the epidermal collection of melanocytes [3]. CALS are considered one of the early manifestations of neurofibromatosis 1 (NF1) [2]. However, there is numerous association with CALS4.
Table 1: Several associations implicated in café au lait spots [3,5,9-12].
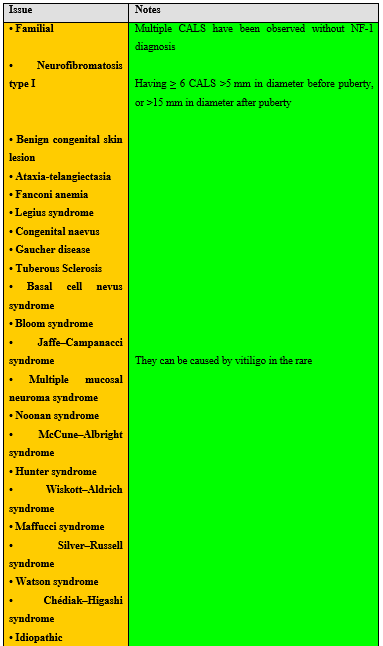
Diagnosis is clinical observation with measurement of the spot size. The number of spots is highly significant for the diagnosis of associated disorders. Anyway, ≥ spots of at least 5mm in diameter in prepubertal children and at least 15mm in post-pubertal individuals is one of the major diagnostic criteria for NF15. The following are suggestive findings [5] for diagnosis of associated disorders such as NF1.
Neurofibromatosis 1 (NF1) should be suspected in individuals who have any of the following findings:
- ≥ 6 CALS >5 mm in greatest diameter in pre-pubertal persons and >15 mm in greatest diameter in post-pubertal persons.
- Two or more neurofibromas of any type or one plexiform neurofibroma.
- Axillary or inguinal Freckling.
- ≥ Lisch nodules (iris hamartomas).
- Optic glioma.
- A distinctive osseous lesion e.g. sphenoid dysplasia or tibial pseudarthrosis
- A first-degree relative (parent, sib, or offspring) with NF1 as defined by the above criteria
The diagnosis of NF1 is established in a proband who meets the diagnostic criteria for NF1 developed by the National Institutes of Health (NIH) [6]. The NIH diagnostic criteria for NF1 are met in an individual who has two or more of the features listed in suggestive findings [5]. The NIH diagnostic criteria are both highly specific and highly sensitive in adults with NF1 [7].
Café au lait spots are often harmless and benign and do not cause any illness or problems [4]. Café au lait spots can be removed with lasers [8]. Despite pheochromocytoma is a rare disorder in cases of NF1, It may be a cause for uncontrolled hypertensive crisis [1]. Pheochromocytoma happens in a range of 0.1%-5.7% of patients with NF-1 [9]. The incidence of an uncontrolled hypertensive crisis increases by up to 20% among pheochromocytoma [10]. However, the association between uncontrolled hypertensive crisis and pheochromocytoma rare [9]. Diagnosis is a clinical requiring highly suspicion of the condition to arrive at the right way [9].
Case Report
A 47-year-old married, farmer, Egyptian male patient presented to emergency (ER) room with headache and dizziness. He denied the history of cardiovascular diseases, the same attack, drugs or any other special habits. Chest pain had become anginal, compressible, and progressive. Upon general physical examination; generally, the patient was anxious, profuse sweaty, with a regular heart rate of 66 bpm, blood pressure of 230/140 mmHg, respiratory rate of 18 bpm, the temperature of 36.9 °C, and pulse oximeter of O2 saturation of 97%. Multiple anterior chest café au lait spots and axillary freckling were seen (Figure 1) No more relevant clinical data were noted during the clinical examination. He was admitted to the intensive care unit as a hypertensive crisis. Urgent ECG showed down-sloping ST-segment depressions in the anterolateral (I, aVL, V5 and V6) leads, prolonged QT-interval of 600 msec with the Corrected QT Interval (QTc;) 600 msec, wide T-wave, and abnormally were seen U-wave (Figure 2). Hypertensive crisis due to pheochromocytoma was the most probable diagnosis. A sublingual 5-dinitrate tablet was given (5 mg). O2 inhalation was given (100%, by nasal cannula, 5L/min). Intravenous nitroglycerin infusion (10 µg/min with intermittent titration) was given. Within 6 hours later, there was no difficulty in blood pressure controlling. Labetalol oral tablet (100 mg twice daily). Dramatic clinical improvement and blood pressure controlling within 15 minutes had happened. Despite there was still an electrocardiographic ST-segment depression. Measured random blood sugar was 173 mg/dl. The troponin test was negative. D-dimer was negative. Later echocardiography showed left ventricular hypertrophy with a normal ejection fraction of 63%. The patient was discharged within 12 hours on oral nitroglycerin retard capsule (2.5 mg twice daily) and labetalol oral tablet (100 mg twice daily). Planning for further investigation was a future option.

Figure 1: Chest imaging showing multiple café au lait spots with the largest one marked in (green arrow) and several near axillary freckling (red arrows).
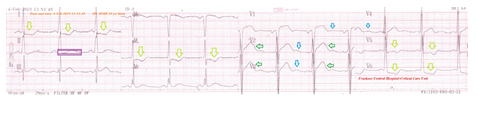
Figure 2: ECG tracing showing down-sloping ST-segment depressions the anterolateral (I, aVL, V5, and V6) leads (lemon arrows), prolonged QT-interval of 600 msec with the Corrected QT Interval (QTc;) 600 msec (purple rectangle), wide T-wave (green arrows), and abnormally were seen U-wave (blue arrows).
Discussion
Overview
- A 47-year-old married, farmer, Egyptian male patient presented ER with a hypertensive crisis and manifested with café au lait spots and axillary freckling
- I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near
Limitations of the study
- There are no known limitations to the study.
- The objective primary for my case study was the presence of hypertensive crisis which manifested with café au lait spots and axillary freckling
- The secondary objective for my case study was the question of how is the café au lait spots with NF1 and pheochromocytoma significant in the management of hypertensive crisis.
Conclusion and Recommendations
Café au lait Spot is a marker for pheochromocytoma in hypertensive crisis but with the considered wide-differential diagnosis.
Labetalol may be the recommended choice in the cases of hypertensive crisis due to pheochromocytoma.
Acknowledgment
The author wishes to thank the critical care unit nurses who make extra ECG copies for helping me.
Conflicts of Interest
There is no conflicts of interest.
References:
- Plensdorf S, Martinez J. Common pigmentation disorders. American Family Physician. 2009;79(2):109-16. PMID 19178061.
- Abeliovich D, Gelman-Kohan Z, Silverstein S, et al. Familial café au lait spots: a variant of neurofibromatosis type 1. J Med Genet. 1995;32(12):985-6. PMID: 8825931 PMCID: PMC1051784 DOI: 10.1136/jmg.32.12.985.
- Goldsmith LA. Fitzpatrick's dermatology in general medicine 8th ed.. New York: McGraw-Hill Medical. 2012;239. ISBN 978-0-07-166904-7.
- Morelli, JG. CURRENT Diagnosis & Treatment: Pediatrics, 22e. New York, NY: McGraw-Hill. 2013pp. 15: Skin. ISBN 978-0-07-182734-8.
- Friedman JM. Neurofibromatosis 1. Available online: https://www.ncbi.nlm.nih.gov/books/NBK1109/ (Accessed: June 6, 2019).
- NIH. National Institutes of Health Consensus Development Conference Statement: neurofibromatosis. Bethesda, Md, USA, July 13-15, 1987. Neurofibromatosis. 1988;1:172-8. PMID:3152465.
- Ferner RE, Gutmann DH. Neurofibromatosis type 1 (NF1): diagnosis and management. Handb Clin Neurol. 2013;115:939-55. PMID:23931823 DOI:10.1016/B978-0-444-52902-2.00053-9.
- Hardy CL. Laser Treatment of Benign Pigmented Lesions. Available online: https://emedicine.medscape.com/article/1120359-overview (Accessed: June 30, 2019).
- Petrovska J, Kitanovska BG, Bogdanovska S, Kuzmanoska SP. Pheochromocytoma and Neurofibromatosis Type 1 in a Patient with Hypertension. Open Access Maced J Med Sci. 2015;15;3(4):713-6. PMID:27275314 PMCID:PMC4877914 DOI:10.3889/oamjms.2015.130.
- Walther MM, Herring J, Enquist E, Keiser HR, Linehan WM. Von Recklinghausen’s disease and pheochromocytomas. J Urol. 1999;162(5):1582-6. PMID:10524872.
- Arnsmeier SL, Riccardi VM, Paller AS. Familial Multiple Cafe au lait Spots. Arch. Dermatol. 1994;130(11):1425-1426. doi:10.1001/archderm.1994.01690110091015. PMID 7979446.
- Whyte MP, Podgornik MN, Zerega J, Reinus WR. Café-au-lait spots caused by vitiligo in McCune-Albright syndrome. J Bone Miner Res. 2000;15(12):2521–2523. doi:10.1359/jbmr.2000.15.12.2521. PMID 11127218.

