An Unusual Cause of Respiratory Distress in a Newborn
Christin L1, Lindsay E1, Raja R2 and Steven MD1
1Department of Pediatrics, Division of Neonatal-Perinatal Medicine, C.S.Mott Children's Hospital, Michigan Medicine, University of Michigan, Ann Arbor, Michigan, USA
2Department of Pathology, Division of Pediatric and Perinatal Pathology, C.S.Mott Children's Hospital, Michigan Medicine, University of Michigan, Ann Arbor, Michigan, USA
Received Date: 01/07/2020; Published Date: 07/08/2020
*Corresponding author: Christin Lawrence, 8-621 C.S. Mott Children’s Hospital, 1540 East Hospital Drive Ann Arbor, MI 48109-4254, USA. Tel: 734 763-4109; Fax: 734 763-7728; E-mail: lawrencechristin@gmail.com
Abstract
We report a case of a preterm male, who presented with respiratory distress and was found to have tracheal agenesis and other anomalies, including laryngeal atresia, lung lobation anomalies, esophageal-pulmonary fistula, duodenal atresia, and complex congenital heart defects. Tracheal agenesis is rare and has been described in association with other anomalies, though this specific combination of anomalies has not been previously described.
Keywords: Tracheal Agenesis; TACRD
Introduction
Tracheal agenesis is an infrequent anomaly and is fatal in most cases. Newborns often present with respiratory distress and are extremely difficult to intubate [1]. The reported incidence is 1 per 50,000 live births [2]. Tracheal agenesis may be associated with other anomalies including VACTERL (vertebral defects, imperforate anus, tracheoesophageal fistula, cardiac anomalies, renal anomalies, and limb anomalies) and TACRD (tracheal atresia or laryngo-tracheal atresia, cardiac anomalies, renal anomalies, and duodenal atresia) [1,3,4]. The case below describes an unusual lethal combination of malformations.
Case Report
This patient was a preterm male born at 27 2/7 weeks’ gestation by primary Cesarean section following premature rupture of membranes, vaginal bleeding with concern for placental abruption, and a non-reassuring fetal heart rate pattern. The mother had complained of decreased fetal movement beginning one week prior to delivery and received two doses of betamethasone after hospital admission. The prenatal history was significant for maternal depression, managed with Escitalopram, obesity, and a maternal family history significant for type I diabetes mellitus. Maternal serologies were unremarkable with the exception of a nonimmune rubella status. Antenatal sonography was concerning for intrauterine growth restriction and an abnormal umbilical artery Doppler flow study showing intermittently absent end diastolic flow. Additionally, findings suggestive of Tetralogy of Fallot were seen on fetal echocardiography. Amniocentesis was performed for a chromosomal microarray and FISH for DiGeorge Syndrome; both were normal.
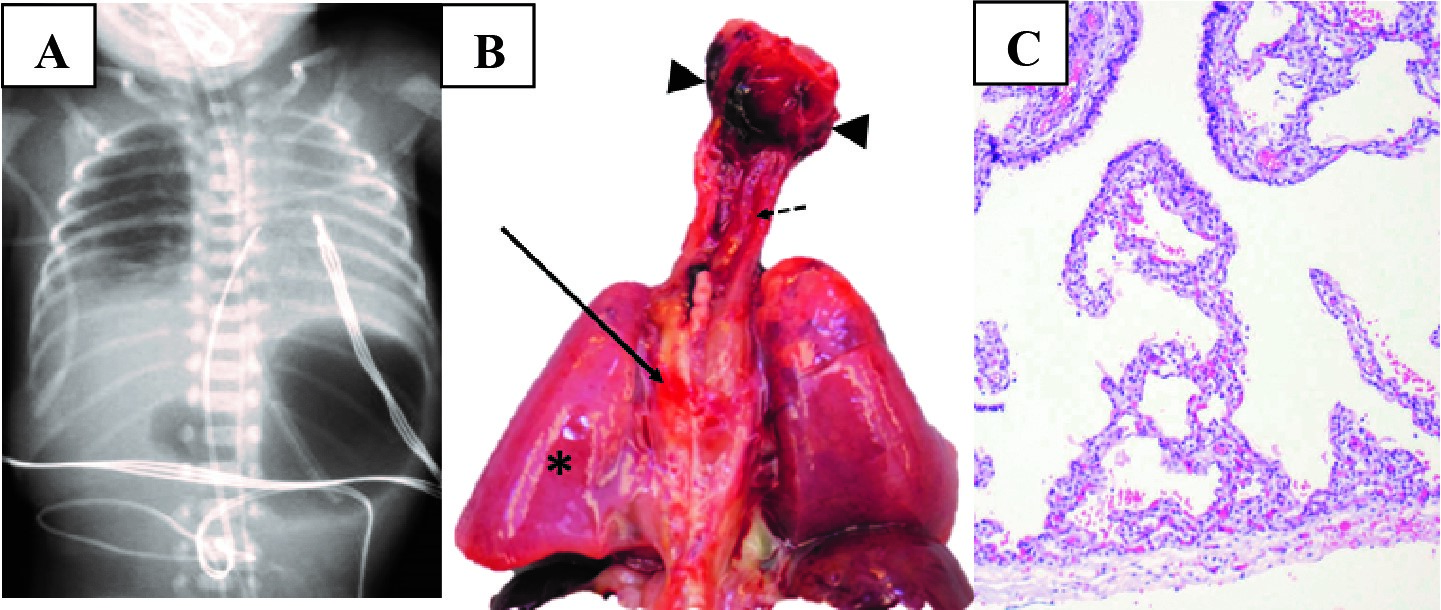
At delivery, Apgar scores were 2, 6, and 8 at one, five, and ten minutes, respectively. The neonate was intubated in the delivery room for respiratory failure. Endotracheal tube placement was confirmed with colorimetric capnography, auscultation of breath sounds, and radiography. Surfactant was administered for respiratory distress syndrome. He underwent a sepsis evaluation and was treated with empiric antibiotics. He developed severe hypotension and was given vasopressors. Radiography revealed a “double bubble sign,” concerning for duodenal atresia, which prompted gastric decompression. By 24 hours of age, there was concern for an esophageal intubation based on review of the radiographic images; however, the infant continued to tolerate minimal ventilator support. A repeat chest radiograph revealed a deeply placed endotracheal tube and poor aeration of the left lung, with persistent gastric distension (Figure 1A). The endotracheal tube was retracted. Colorimetric capnography failed to show a color change and prompted direct laryngoscopy, which revealed the endotracheal tube to be in the esophagus. Reintubation by direct laryngoscopy was attempted but was unsuccessful. The neonate responded to T-piece ventilation, with a positive color change and was subsequently evaluated by pediatric otolaryngology and transported to an operating room, where tracheal agenesis was discovered. The neonate was transitioned to comfort care and expired at 35 hours of age.
A postmortem examination found multiple anomalies, including laryngeal atresia and complete absence of the trachea and bronchi with a small fistula from the esophagus to the right lung (Figure 1B). There was no obvious fistula to the left lung nor lobation of the left lung. There was bilateral pulmonary hypoplasia with hyaline membrane formation (Figure 1C). Complex congenital heart disease was also found, including a double outlet right ventricle, pulmonary valvular stenosis, and a severely hypoplastic main pulmonary artery and branches. The aorta arose from the right ventricle, and there was anomalous right-sided pulmonary venous return and a moderate ventricular septal defect. Duodenal atresia was indeed present. Other anatomic abnormalities included multiple accessory spleens, increased extramedullary hematopoiesis, bile duct paucity, a right retroperitoneal undescended testis, and mild early ischemic changes within the brain.
Discussion
Tracheal agenesis is a rare and usually fatal diagnosis [1]. Prenatal diagnosis is difficult and typically suspected in the setting of congenital high airway obstruction syndrome (CHAOS) [2]. Floyd classified tracheal agenesis into three types: type I- agenesis of the upper trachea, normal bronchi, and a tracheoesophageal fistula; type II- complete tracheal agenesis, normal bronchi, and a fistula between the carina and esophagus; and type III- a bronchus arising from the esophagus separately [5]. The present case did not fit any of these classifications, but rather had an esophageal-pulmonary fistula. The duodenal atresia may have aided ventilation, as the enlarged gastric bubble with distal obstruction increased resistance to flow, diverting gas flow through the lower resistance fistula to the lung. Approximately half of newborns with duodenal atresia also have an anomaly of another organ system [6]. The most common include congenital heart disease, intestinal malrotation, esophageal atresia, and annular pancreas; however, a combination of anomalies in a single patient is rare [7,8].
Though other congenital anomalies are often present with tracheal agenesis, a combination of the specific anomalies observed in this case has not yet been reported. The combination of tracheal agenesis and associated anomalies has been described with the VACTERL association (vertebral defects, imperforate anus, tracheoesophageal fistula, cardiac anomalies, renal anomalies, and limb anomalies) [3]. Evans and colleagues described tracheal agenesis associated with other malformations, a pattern known as TACRD, which includes tracheal atresia or laryngo-tracheal atresia, cardiac anomalies, renal anomalies, and duodenal atresia [4]. They reviewed 84 cases of tracheal atresia compared to 28 cases of tracheoesophageal atresia and found tracheal atresia to be more common in males [4]. Additionally, they noted that infants with tracheal atresia were more often premature and had a history of growth restriction compared to patients with isolated tracheoesophageal fistula. They stratified findings into four sub-populations, summarized in Table 1. The first group was characterized by anomalies specific to the trachea and larynx accompanied by cardiac defects. The second group described more complex cardiac anomalies and lung lobation anomalies. The third group included caudal anomalies, including anal and renal anomalies, in addition to the thoracic anomalies mentioned above. The fourth group had a more severe pattern of anomalies including three organ systems in addition to the airway anomalies; many infants had midline defects, such as vertebral anomalies and a large number of anomalies involving foregut derivatives, such as the esophagus, stomach, pancreas, and duodenum. There were no known chromosomal abnormalities in these cases [4]. This infant was most closely related to the fourth group described by Evans, given the laryngeal atresia and tracheal-bronchial agenesis, complex congenital heart disease, lack of lobation of the left lung, and duodenal atresia along with abnormalities of the liver and spleen.
Conclusion
In summary, the diagnosis of multiple anomalies with tracheal agenesis is rare. This case demonstrated two important features. First, when two major abnormalities are present, it is important to screen for additional associated anomalies. In this case, the baby was diagnosed with Tetralogy of Fallot prenatally and there was concern for duodenal atresia postnatally. If time allowed, it would have been pertinent to obtain further evaluation, such as a sonographic investigation of the liver and kidneys. Thorough examination for abnormalities on physical examination is also essential. Second, this case demonstrates the importance of a postmortem examination, which provides detailed anatomic information. In this case, it revealed additional anomalies there were not known prior to death. Postmortem examination may also be useful in providing information to determine the recurrence risk and for subsequent pregnancy counseling.
Author Contributions
Ø Christin Lawrence, DO: Designated guarantor; acquired data and literature review, and drafted article.
Ø Lindsay Ellsworth, MD: Literature review, designed table and figure legends, and revised article.
Ø Raja Rabah, MD: Prepared and provided figures and revised article.
Ø Steven Donn, MD: Senior author; extensively revised article and provided mentorship and guidance to primary author.
Conflicts of Interest
The authors report no conflicts of interest.
Grant Information
The authors received no specific funding for this work.
References:
- Krishnamurthy K, Kochiyil J, Poppiti, RJ. Tracheal agenesis with esophageal atresia: an autopsy case report of a variant incompatible with life. Fetal and Pediatric Pathology. 2020;39(1):45-50.
- Park BJ, Kim MS, Yang JH, Jun TG. Tracheal agenesis reconstruction with external esophageal stenting: postoperative results and complications. Korean J Thorac Cardiovasc Surg. 2015;48:439-42.
- Wei JL, Rodeberg D, Thompson DM. Tracheal agenesis with anomalies found in both VACTERL and TACRD associations. Int J Pediatr Otorhinolaryngol. 2003;67(9):1013-7.
- Evans JA, Greenberg CR, Erdile. Tracheal agenesis revisited: analysis of associated anomalies. Am J Med Genet. 1999;82:415-22.
- Floyd J, Campbell DC Jr, Dominy DE. Agenesis of the trachea. Am Rev Respir Dis. 1962;86:557-60.
- Bailey PV, Tracy TF Jr, Connors RH, Mooney DP, Lewis JE, Weber TR. Congenital duodenal obstruction: a 32-year review. J Pediatr Surg. 1993;28(1):92-5.
- Sweed Y. Duodenal obstruction. In: Puri P, editor. Newborn Surgery.2nd ed. London: Arnold; 2003. p. 423.
- Mirza B, Ijaz L, Saleem M, Sheikh A. Multiple associated anomalies in a single patient of duodenal atresia: a case report. Cases J. 2008;1(1):215.

