A dirty that kills: A Tetanus Case Report
Nkya JS1 and Mkwizu E1*
Kilimanjaro Christian Medical Center, Kilimanjaro, Tanzania
Received Date: 12/07/2020; Published Date: 31/07/2020
*Corresponding author:
Mkwizu E, Department of internal medicine at Kilimanjaro Christian Medical Center, Institute of public health, Kilimanjaro Christian Medical University College, Kilimanjaro, Tanzania. E-mail: emkwizu@gmail.com
Abstract
Tetanus is a bacterial disease caused by Clostridium tetani spores entering the body via broken skin barrier. The symptoms and signs include inability to open mouth, painful spasm of back, abdomen and extremities muscles which may be triggered by light or noise, spasm of facial muscles, neck stiffness, changes in blood pressure and fast heart rate. Tetanus diagnosis is mainly clinical, treatment is based on immunotherapy, antibiotics, and muscle relaxant and airway management. The earlier the diagnosis the better the outcome. Tetanus toxoid injection in adults is given in 3 doses, first 2 doses in 4week interval and last dose at 6-12 months. Three booster doses are recommended after 10 years of full primary immunization. This is a report of a 30 years old male who presented to the emergency department with inability to open mouth and was ultimately diagnosed with tetanus. This report highlights the importance of tetanus vaccination in adults, mostly males as women are scheduled in pregnancy.
Keywords: Tetanus; Spore; Trismus; Risus Sardonicus
Introduction
Tetanus is a serious illness contracted through exposure to the spores of bacteria that lives in soil, saliva, dust and mite called Clostridium tetani [1]. Tetanus is an acute neuromuscular disease as spores enter the body through skin breakage [2]. Tetanus has 3 clinical forms; it can be generalized, localized or cephalic, generalized pattern is most common, presents with spasms of masseter muscle (trismus) which progresses to painful generalized spams of muscles of neck, abdomen and extremities [3]. Localized and cephalic types are less common, and may progress to the generalized form. Tetanus was first discovered in Egypt over 3000 years ago and was prevalent throughout the world despite passive immunization since 1893 and effective active immunization in 1923 it continues to have significant morbidity and mortality worldwide [4].
Globally in 2015 non neonatal tetanus deaths were 36,806, Eastern Sub-Saharan Africa 8,834 and in Tanzania 683, with most deaths in Africa, South Asia and China [5]. In a retrospective study on tetanus done in Tanzania at Muhimbili national referral hospital in Dar es salaam with 91% of males and only two women, mortality rates were 72.7% in 1-10days hospital stay [6]. In Tanzania, only 28% of males aged at least 15 years are immunized against tetanus [7].
There is no cure for tetanus, only management of complications can be done until the effects of tetanus toxin resolves.
Here, we describe the case of a 30 years old male (with unknown immunization history) who presented with inability to open the mouth and unable to articulate words that was ultimately diagnosed with tetanus.
Case Report
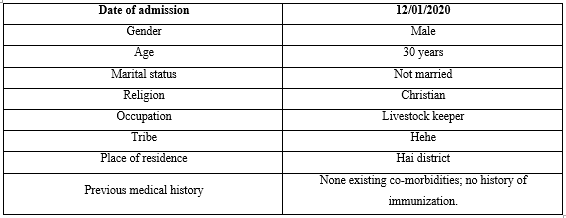
A 30 years old man was admitted to medical ward in Kilimanjaro Christian Medical Center (KCMC-a zonal consultant referral hospital) on January 2020. He presented with history of inability to open mouth and articulating words for 4 days following a motor traffic accident (MTA) as a motorcycle passenger under the influence of alcohol 6 days prior to the onset of the symptoms. The resultant injuries were bruises on the left side of his face and shoulder. Thirty minutes later at his domicile address he dressed them with gauze without observing any antiseptic technique. There was no history of loss of consciousness reported or bleeding per ear nose and throat, no headache or hypersensitivity to bright light, no history of vomiting or blurry vision. The patient denied to have received tetanus prophylaxis for the wound and as far as he could remember he had never received one. He was taken to a local hospital in Hai district where he was given anti pain and advised to go to a regional referral hospital for further management. About 2 days later he went, where the referral letter says he had one episode of convulsion, generalized, lasted for about 2 minutes and was not associated with loss of bowel and bladder control. He was sedated with diazepam before being referred to KCMC for further management. His socio demographic characteristics and previous medical history are summarized in Table 1.
Table 1: Socio demographic characteristics and previous medical history.
Physical Examination
On physical examination he was alert, febrile with temperature of 380C, tachypnea with a respiration rate (RR) of 26breaths/min, had a tachycardia of 110 beats/min, BP of 100/70mmhg, saturating at 95% in room air, random blood glucose (RBG) of 7mmol/l. He had neck stiffness, unprovoked episodes of spasm of neck and jaw muscles (risus sardonicus) associated with shortness of breath without neck hyperextension or opisthotonus. Kerning was negative.
On local examination of the wounds, he had a healing septic wound on the left frontal temporal region approximately 5 x 4 cm discharging yellowish pus, on the left shoulder superiorly about 3 x 4 cm dry healing wound. He was conscious with Glasgow Coma Score (GCS) of 15/15, intact memory short and long term, slurred speech, pupils were reactive to light with hemineglect, cranial nerves were intact except CN IX, X and XII couldn’t be assessed (due to inability to open mouth). Muscle tone was normal, power of 5/5 reflexes were intact except Babinski which was unresponsive. Cardiovascular and per abdomen were unremarkable, lungs auscultation he had bilateral basal crepitation’s. A provisional diagnosis of tetanus was reached.
Laboratory Investigations
Laboratory investigations done were full blood picture (FBP), blood grouping and cross match, Na+, K+, BUN, SCr, blood culture, lumbar puncture and CT scan on 12/01/2020. Cerebral spinal fluid (CSF) analysis and microbiology were uneventful, FBP showed leukocytosis of 19.36 * 109/L (4.00-11.00*109/L) with predominant neutrophils of 88.69% indicating ongoing infection, hypernatremia of 149mmo/l (136-145) and hypokalemia of 3mmol/l (3.5-5.1) indicating slight electrolyte imbalance, normal serum urea of 5.77mmo/l (0.0-8.3) and serum creatinine of 41mcmol/l (62-106). Blood culture results did not grow any organism. CT scan showed bilateral maxillary haemosinusitis, no calvarial bone fracture, no epidural/subdural collection or area of cerebral hemorrhagic contusion seen.
Treatment Given
The patient was given human anti tetanospasmin immunoglobulin TIG injection 5000 units IM start at emergency department, metronidazole 500mg IV 6hrly for 5 days, ceftriaxone 1g IV start, diazepam 10mg IV 4hrly for 5days (seizures were controlled) and paracetamol 1g start. Surgical debridement of both wounds was done, left open and he was transferred to Medical Intensive Care Unit (MICU). First day post admission at 15:58:34 he started desaturating to 52%, he was intubated under sedation with thiopental 500mg and succynyl 100mg, ETT 7.5 cuff was inserted at 22cm and saturations improved to 97%. The tube was secured and he was kept on mechanical ventilation.
At the same day, at around 18hours his BP was 213/89, PR 190, SO2 97% on mechanical ventilation, RR 36, RBG 13.1, was diaphoretic (i.e. sweating heavily), and at 21:10 the patient started to gasp, vitals were not recordable, pupils were dilated and sluggish reacting to light. Resuscitation was done for 20 minutes with ambubag and chest compressions but was unsuccessful and death was certified.
Discussion
Tetanus is a medical emergency and diagnosis is mainly dependent on carefully taken history and pattern of clinical presentation. Usually the incubation period is 7-21days where spores germinate locally under anaerobic mechanism producing an tetanospasmin and tetanolysin. Tetanolysin is locally lyses and tetanospasmin follows a retrograde axonal flow to myoneural junctions. Tetanospasmin binds the neural muscular receptors results in continuous stimulation which produces painful contractions associated with inhibition of GABA receptors [3].
WHO defines adult tetanus by one of the following signs, trismus (inability to the open mouth), risus sardonicus (sustained spasm of the facial muscles) and painful muscular contractions with the patient recalling history of injury or not [8]. In current case presentation, it took about two weeks until the patient came to KCMC hospital since he got involved in MTA, and by the time he was admitted at KCMC he presented with episodes of risus sardonicus and trismus. This falls within the incubation period of 7-21 days and WHO definition of tetanus as described above. One of the reasons for late help-care seeking at KCMC hospital was lack of funds. He was not on any medical insurance cover and he didn’t have any family support except his fellow local workers. Due to limited financial resources, he failed to cover the direct cost like buying tetanus immunoglobulin second dose as he received the first on admission. This late presentation led to undesirable outcome as it opposes WHO recommendation of earlier treatment the better the outcome [9], as well as missing the second immunoglobulin dose.
Tetanus diagnosis is strictly clinical, there are no confirmatory laboratory tests. Despite the slight derangement in electrolytes (Na+, K+) and raised neutrophils, autonomic dysfunction (i.e. with hypertension of 213/89mmhg and tachycardia of 190bpm) caused death.
Tetanus toxoid injection in adults is given in 3 doses, first 2 doses in 4week interval and last dose at 6-12 months (CDC 2009). Three booster doses are recommended after 10 years of full primary immunization.
Tetanus toxoid injection is mandatory for any open wound for tetanus prevention. Community is aware but most, especially adult men tend to ignore minor injuries for vaccine, booster or immunoglobulin.
In conclusion, the case discussed here shows that unvaccinated adults which most are males once exposed to tetanus spores, the outcome may be fatal. Thus more enforcement toward tetanus toxoid injection is needed, especially in adult men.
Acknowledgements
Dr. Bernard Njau for reviewing the final draft of case report, Jamil for helping me with the corrections and my fellow MD5 students 2020 at KCMUCo for all the support in one way or another in accomplishing this work.
Conflicts of Interest
No potential conflict of interest
References:
- WHO. Tetanus. http://www.who.int/health-topics/tetanus, accessed on 25th April 2020.
- Judith A, Cottrill G, Lancioni C, Eriksson C, Cho YJ, Liko J. Tetanus in an Unvaccinated Child- Oregon. Morbidity and mortality weekly report. 2017.
- Mcelaney P, Iyanaga M, Monks S and Michelson E. The quick and dirty; A tetanus case report. 2019;3(1):55-58.
- Farrar JJ, Yen LM, Cook T, Fairweather N, Binh N, Parry J, et al. Tetanus, NEUROLOGICAL ASPECT OF TROPICAL DISEASE. 2000;69:292-301.
- Kyu HH, Mumford JE, Stanaway JD et al. Mortality from tetanus between 1990 and 2015; findings from global burden disease study 2015. BMC Public Health. 2017;17:179. https://doi.org/10.1186/s12889-017-4111-4.
- Mchembe MD and Mwafongo V. Tetanus and its treatment outcome in Dar es salaam: Need for Male Vaccination. East African Journal of Public Health. 2005;2(2);22-23.
- Aziz R, Peck RN, Kalluvya S, Kenemo B, Chandika A, Downs JA. Tetanus in adult males, Bugando Medical Centre, United Republic of Tanzania. Bulletin of the world health organization. 2017;(97)729-792.
- WHO. Current recommendations for treatment of tetanus during humanitarian emergencies. 2010.
- WHO. Fact sheet on tetanus. http://www.who.int/news=room/fact-sheet, accessed on 4th April 2020.
- Alfilfil WA, Alshahrani MS, Abdulbaser MA, El Fakarany NEB. Severe generalized tetanus: A case report and literature review. 2015;(3)2:167-169.
- Felman A. Everything you need to know about tetanus. Medical News Today. 2017.
- Liu SW, Huang LC, Chung WF, Wu J, Chen LF, Chen CY. Tetanus Vaccination and Extra-Immunization among Adult Populations: Eight – Year Follow Up Cohort Study of 771,443 Adlts in Taiwan. 2018;15(8):1622.

