Intestinal Mucormycosis Presenting as Perforation Peritonitis in a 35 Year Old Diabetic Male: Case Report
Shreyash R*
Department of General Surgery, UCMS and GTB Hospital, New Delhi, India
Received Date: 15/06/2020; Published Date: 15/07/2020
*Corresponding author:Shreyash Rai, Department Of General Surgery, Ucms And Gtb Hospital, Ward 24, Surgery Office 4th Floor,University College Of Medical Sciences, New Delhi-110095, India. E-mail: shreyash001@hotmail.com
Abstract
Invasive mucormycosis causes extensive angioinvasive disease with high mortality rates in patients with risk factors. Gastrointestinal mucormycosis is a rare form of the disease with increasing number of cases being reported from developing countries. Early stages of the disease largely remain unrecognised due to nonspecific symptoms and signs. We report a case of intestinal mucormycosis presenting as perforation peritonitis in a 35 year old diabetic male. He was managed surgically and with anti-fungal therapy. The patient expired postoperatively. Gastrointestinal mucormycosis still largely remains a post-mortem diagnosis because of nonspecific clinical signs and symptoms and the aggressive nature of the disease.
Keywords: Mucormycosis; Intestinal; Gastrointestinal; Case Report
Introduction
Invasive mucormycosis is an uncommon disease particularly affecting immunocompromised individuals. Individuals with solid organ transplantation, heamatopoeitic stem cell malignancy, receiving corticosteroids or deferoxamine therapy and uncontrolled diabetics are especially at risk with notably high reported mortality rates [1]. Depending on the site involved, mucormycosis has been divided into rhinocerebral, pulmonary, gastrointestinal, cutaneous, isolated renal and disseminated forms [2]. Gastrointestinal involvement is rare with stomach, colon and small bowel being the usual sites of involvement [3].
Case Report
A 35 year old male presented to the emergency room of a tertiary care centre with abdominal pain since 1 month which had a sudden increase in intensity associated with multiple episodes of vomiting and abdominal distension since 5 days. Patient was not a known diabetic and was not on any immunosuppressant drugs. He was in shock and abdominal examination revealed peritonitis. Investigations revealed deranged blood sugar levels and the erect chest X-ray showed gas under the right diaphragm. No viral marker was positive. A previous CECT of the abdomen done 20 days ago was suggestive of ascites, ileal thickening and decreased enhancement of terminal ileum (Figure 1 and 2). Patient was taken up for exploratory laparotomy which revealed 2 litres of fecopurulent peritoneal contamination. A 3*3 cm perforation was identified in jejunum 10 cm distal to duodenojejunal junction with 30 cm of gangrenous ileum with multiple perforations. Resection of the jejunal perforation and anastomosis was done with retrograde duodenostomy and distal feeding jejunostomy considering the contamination. Gangrenous ileal segment was resected and a double barrel ileostomy was formed. Histopathology revealed mucormycosis (Figure 3) when liposomal amphotericin B was started for the patient. Patient could not recover and expired postoperatively.
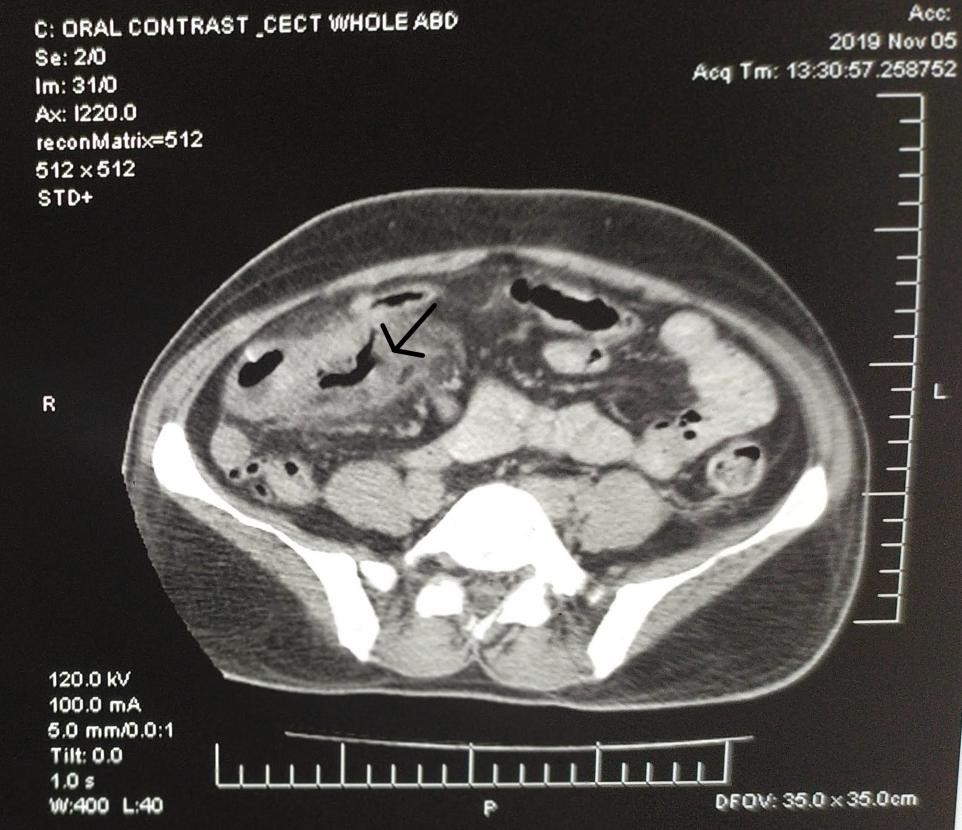
Figure 1: Thickened non enhancing ileum on CECT hyphae.
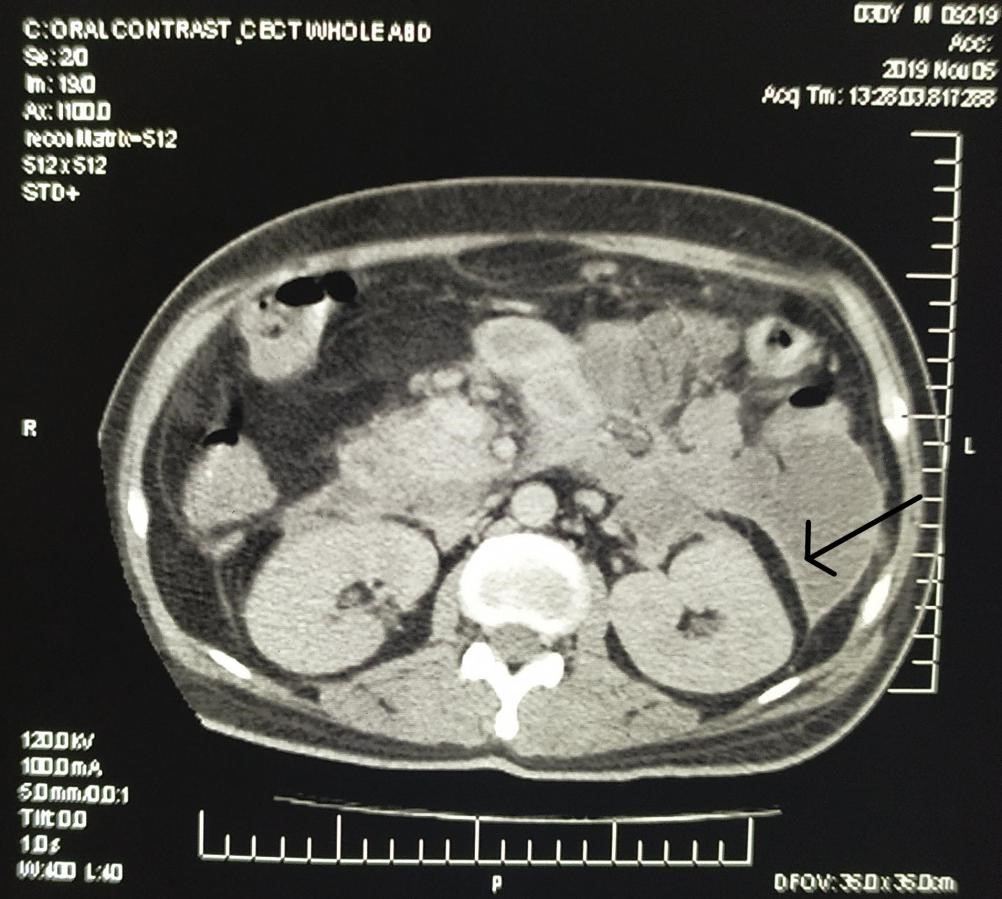
Figure 2: Ascites with peritoneal enhancement on CECT.
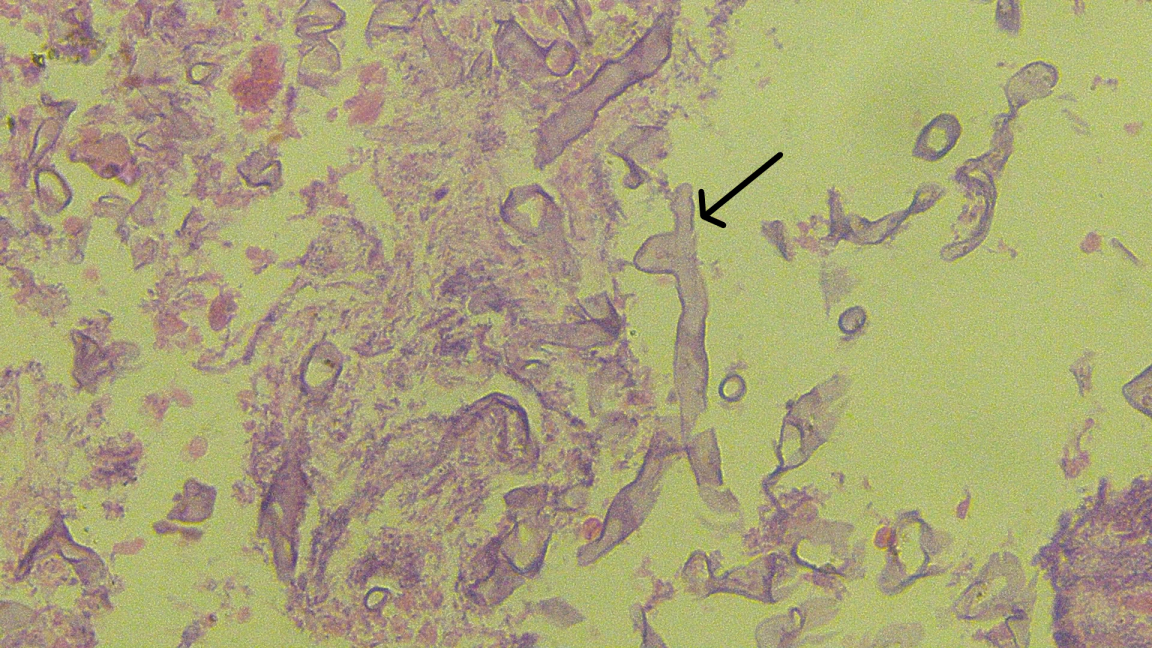
Figure 3: Biopsied specimen showing broad aseptate hyphae in necrotic background.
Discussion
Primary gastrointestinal disease is the least frequent form of presentation for mucormycosis. Early diagnosis and treatment are important considering the aggressive nature of the disease. Colonoscopy and biopsy of the affected segment may help prove the diagnosis. In other cases, biopsy after laparotomy paves the way. Clinical diagnosis of the same is difficult due to nonspecific clinical features with most of the diagnosis being formed after histopathological analysis post-surgery or post-mortem [4]. Radiological features are nonspecific and CECT features may include thickened bowel wall with intense and poor contrast enhancement suggestive of congested and necrotic areas, respectively [5]. A delay of therapy of more than 6 days has been shown to double the mortality rate [6]. The management of GIT mucormycosis involves surgical debridement and antifungal directed therapy (liposomal amphotericin B) [7]. There is a high reported mortality (63.9%) probably due to delay in diagnosis and rapid progression of the disease after angioinvasion [8]. In conclusion, GIT mucormycosis is a rare life threatening disease with high incidence in immunocompromised patients.
Acknowledgment
I acknowledge the role of Department of pathology, University College of Medical Sciences for providing relevant histopathology photograph.
Funding
No funding was received for the publication of this manuscript.
Conflicts of Interest
No known conflict of interests.
References
-
- Ibrahim AS, Kontoyiannis DP. Update on mucormycosis pathogenesis. Curr Opin Infect Dis. 2013;26(6):508-515.
- Riley TT, Muzny CA, Swiatlo E, Legendre DP. Breaking the Mold: A Review of Mucormycosis and Current Pharmacological Treatment Options. Ann Pharmacother. 2016;50(9):747-757.
- Forrester JD, Chandra V, Shelton AA, Weiser TG. Gastrointestinal mucormycosis requiring surgery in adults with hematologic malignant tumors: literature review. Surg Infect (Larchmt). 2015;16(2):194-202.
- Chakrabarti A, Singh R. Mucormycosis in India: unique features. Mycoses. 2014;57(s3):85-90.
- Lee JH, Ha HK, Yoo E, Yang SK, Min YI, Auh YH. CT and sonographically guided biopsy in a patient with intestinal mucormycosis. AJR Am J Roentgenol. 2000;175(1):129-131.
- Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis. 2008;47(4):503-509.
- Martinello M, Nelson A, Bignold L, Shaw D. “We are what we eat!” Invasive intestinal mucormycosis: A case report and review of the literature. Med Mycol Case Rep. 2012;1(1):52-55.
- Kaur H, Ghosh A, Rudramurthy SM, Chakrabarti A. Gastrointestinal mucormycosis in apparently immunocompetent hosts-A review. Mycoses. 2018;61(12):898-908.

