The Systematized Approach of Hematuria is the Key Even in Unusual Cases: Simultaneous Endovascular and Endourological Management in a Hybrid OR of a Hemorrhagic Shock Secondary to a Ureteroarterial Fistula
Mohamed Bakhri1,2,*, Jaafar Benjaafar Marrakchi1,2, Meryem Sassi2,3, Adil Mellouki1,2, Mustapha Ahsaini1,2, Soufiane Mellas1,2, Jalal Eddine El Ammari1,2, Mohammed Fadl Tazi1,2, Mohammed Jamal El Fassi1,2 and Moulay Hassan Farih1,2
1Department of Urology, Hassan II University Hospital, Morocco
2Faculty of Medicine, Pharmacy and Dentistry of Fez, Sidi Mohammed Ben Abdellah University, Morocco
3Department of vascular surgery, Hassan II University Hospital, Morocco
Received Date: 02/01/2024; Published Date: 20/05/2024
*Corresponding author: Mohamed Bakhri, Department of Urology, Hassan II University Hospital; Faculty of Medicine, Pharmacy and Dentistry of Fez, Sidi Mohammed Ben Abdellah University, Fez, Morocco
Abstract
Ureteroarterial fistula is a rare, life-threatening short-term emergency. It is often secondary, the main causes being prolonged ureteral stenting and pelvic radiotherapy. Haematuria is the main revealing symptom in a particular context.
Diagnostic confirmation is based on angiography, ureteropyelography or arteriography. Treatment is currently based on endovascular and endourological intervention. In our publication, we report the case of a fistula between the right common iliac artery and the pelvic ureter in a patient with an indwelling JJ catheter admitted in hemorrhagic shock, who was managed by a double team in a hybrid urological and vascular operating theatre, consisting of a diversion of the excretory tract and placement of a covered stent in the right common iliac artery. This case illustrates the importance of making an early diagnosis in the presence of haematuria with a range of specific anamnestic and clinical arguments.
Keywords: Haematuria; Uretero-arterial fistula; Endo-urology; Endovascular
Introduction
Ureteroarterial fistula is a rare, life-threatening short-term emergency. It is often secondary, the main causes being prolonged ureteral stenting and pelvic radiotherapy. Haematuria is the main revealing symptom in a particular context [2].
It most often involves the iliac artery, although other arteries may be affected, in particular the abdominal aorta, with an even more serious clinical presentation [3-5].
The therapeutic arsenal is based on a combined endo-urological and endovascular approach, applied in an emergency situation. The aim of our publication is to provide an update on the diagnostic approach and simultaneous treatment using a double team in a hybrid surgical suite including one vascular interventional unit and another urological unit, and to highlight the importance of evoking this diagnosis in the presence of haematuria with a range of specific anamnestic and clinical arguments in order to reduce the morbidity and mortality associated with a delay in diagnosis.
Ureteroarterial fistula is a rare clinical entity in everyday practice, often presenting with frank haematuria, which is life-threatening, with an estimated mortality rate of 9% and morbidity of 23% [6,7].
This pathology is often associated with well-known risk factors including radiotherapy, prolonged ureteral stents, pelvic surgery with a background of degenerative vascular pathology (aortic or iliac artery aneurysm, arterial malformation).
Case Presentation
We present the case of a 77-year-old female patient with a history of gravid hypertension and right iliofemoral bypass surgery for a false aneurysm of the right primitive iliac artery at the age of 39. The sequelae were marked by acute ischaemia of the right lower limb justifying repeat iliofemoral bypass surgery. 2 years later, the patient reported right renal colic, and a uroscanner revealed ureteral stenosis at the crossing with the primitive iliac artery, justifying the use of a JJ catheter with repeated changes. The course was marked by four episodes of acute pyelonephritis.
The patient was admitted as an emergency with clinical and biological signs of pyelonephritis and massive macroscopic haematuria. An angioscan revealed a ureteroarterial fistula (between the ureter and the false aneurysm of the common iliac artery upstream of an iliofemoral bypass) (Figure 1).
After stabilisation of the haemodynamic state and bladder catheterisation with bladder rinses to clear the urine, the patient was admitted to the operating theatre in a hybrid room where the endovascular procedure was carried out firstly by inserting a covered stent, and secondly by a urological procedure involving removal of the excretory tract and insertion of a CH7 endoureteral catheter to allow rinsing of the excretory tract, which was replaced by a JJ catheter at D+2 (Figures 2 and 3).
The patient was allowed to return home postoperatively from day 4, with a follow-up angioscanner at day 21 and at 3 months, and urology follow-up with regular replacement of the JJ catheter.
A 3-month angioscan revealed stability of the false aneurysm, obliteration of the fistula and marked regression of the dilatation of the right ureteropyelocal cavities. Six months later, the patient underwent a segmental ureterectomy with ureterovesical reimplantation on a psoic bladder, enabling the JJ catheter to be weaned.
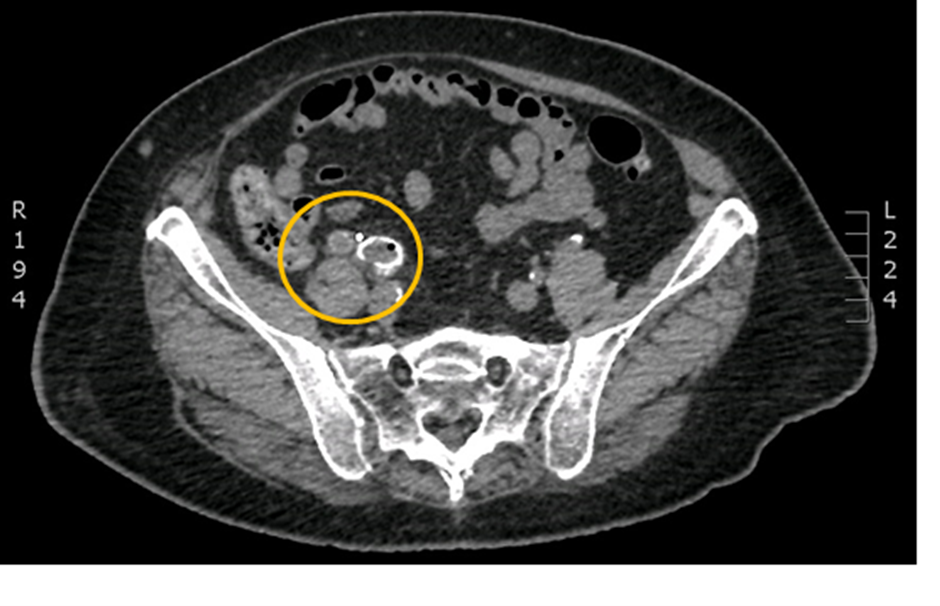
Figure 1: Axial non-contrast CT scan showing infiltration of the peri-ureteral fat and all around the right common iliac arteriovenous axis (yellow circle).
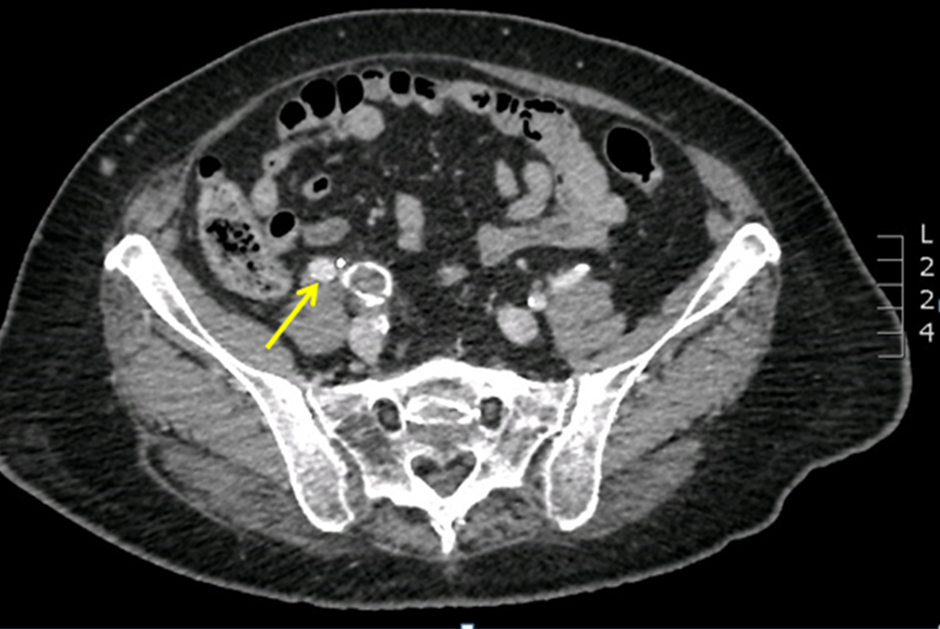
Figure 2: Axial CT scan, after injection of PDC (arteriovenous time) shows early opacification of the dilated right iliac ureter (yellow arrow), indicating a vascular-ureteral fistula.
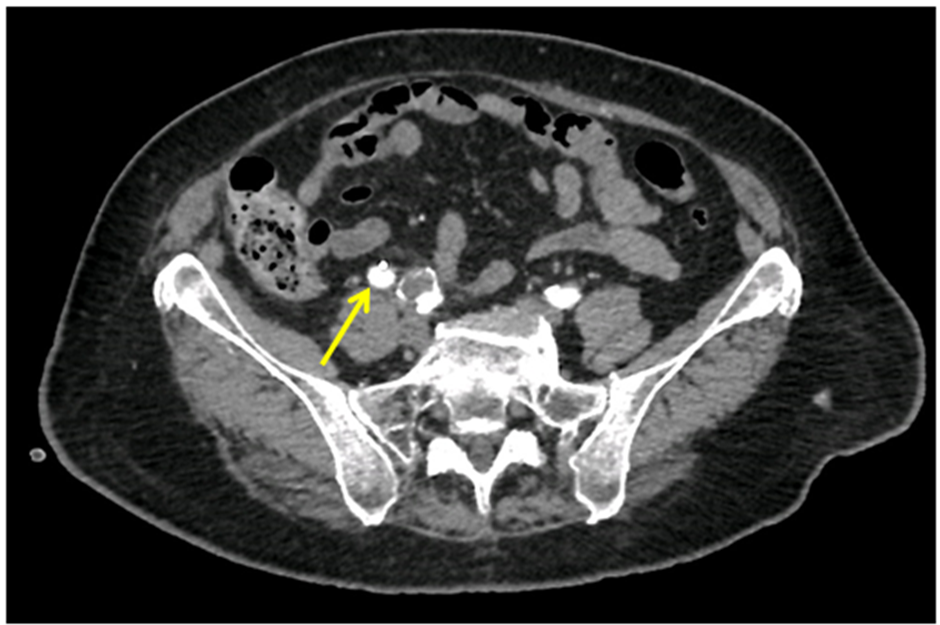
Figure 3: Axial CT section, after injection of PDC (late time): Persistent opacification of the right iliac ureter containing the JJ catheter (yellow arrow).
Discussion
Ureteroarterial fistula (UAF) is a rare condition that represents a life-threatening emergency and requires a rapid, multidisciplinary diagnostic and therapeutic approach.
Ureteroarterial fistulas are primitive in 15% of cases [13], in which case they systematically occur in the setting of degenerative arterial vascular pathology (usually aorto-iliac aneurysm or arteriovenous malformation) [3]. The remaining majority of cases of arterio-ureteral fistula (85%) are secondary, the consequence of complex situations that may involve one or more of the risk factors specified in a study carried out in 2016 on 118 cases of uretero-arterial fistula showed that 67% of cases were women, with the main risk factors being related to an indwelling ureteral stent (73, 3%), a history of malignancy was also common, with cervical, bladder and colorectal cancers being the most frequently observed (25%, 22% and 17% respectively). Abdominal and pelvic surgery (the majority of which were oncological procedures) was reported in 69.5% of patients, and pelvic radiotherapy and vascular pathology were found in 48.3% and 41.5% of patients respectively [1].
The pathophysiology of arterio ureteral fistulisation can be explained by the repeated transmission of arterial beats via a rigid body (ureteral catheter or vascular prosthesis) on an inflammatory (radiation, In our case, the fistula complicates a false aneurysm of the common iliac artery in contact with a ureter fitted with a JJ catheter.
The dominant symptom is haematuria, which is seen in all patients; it may be intermittent or massive, with hypotension or even shock, and in some cases low back pain associated with dilatation of an overlying ureteral obstruction, or pyelonephritis.
In patients with a stent or catheter, bleeding may be provoked or exaggerated when the stent or catheter is changed [1]. Ureteroarterial fistula presents with atypical, non-specific symptoms, making it difficult to diagnose.
Angioscanner is used for initial orientation, and selective intraoperative arteriography appears to be the most effective modality. After injection into the iliac vascular system, direct contrast extravasation through the uretero-arterial defect is documented. As an alternative to arteriography, retrograde ureteropyelography can be used to document direct contrast extravasation from the ureter into the arterial circulation.
In a review by van den Bergh et al, arteriography and retrograde ureteropyelography established the diagnosis of FUA in 69% and 52% respectively [5,9].
There are few other effective options for the detection of FUA, in some cases cystoscopy can help to put pulsatile blood from the corresponding ureteral orifice, abdomino-pelvic CT is usually negative or non-specific and bleeding is rarely seen, if contrast is used the fistula can be visualised with non-specific findings include the presence of a pseudo aneurysm, signs of infection or hydronephrosis. [12].
From a diagnostic point of view, and in order to organise the sequence of paraclinical examinations correctly, Krambec et al suggested that if there is a suspicion of a fistula (haematuria +/- lumbago) + an indwelling ureteral stent and/or radiotherapy and/or abdomino-pelvic surgery, the first step should be angiography, followed by provocative angiography and then cystoscopy. If all these methods are negative and there is a strong suspicion, exploratory surgery can be performed [10].
In our case, the angioscan allowed us to identify the fistula and its aetiology, which enabled our patient to be referred rapidly to the operating theatre. This was a multidisciplinary operation, involving the intensive care unit, radiologist, vascular surgeon and urologist.
Several therapeutic options are available for the treatment of ureteroarterial fistulas, which must include both arterial and ureteral repair. Vascular repair can be carried out openly with embolisation, ligation and extra-anatomical reconstruction, or with a covered vascular stent following angiography, which is considered to be a minimally invasive, rapid and effective procedure that is adapted to each clinical situation and is the gold standard today. Repair of the ureteral defect can be carried out either endoscopically by retrograde JJ catheter assembly or percutaneous nephrostomy. Delayed surgical ureteroplasty may be considered to avoid recurrence. [16, 17].
Conclusion
Ureteroarterial fistula is a rare situation with serious consequences in the absence of emergency diagnostic and therapeutic management. Subject to the availability of the technical platform, the reference treatment should involve simultaneous endovascular and minimally invasive endourological management.
Reducing morbidity and mortality goes hand in hand with diagnostic orientation in the face of macroscopic haematuria in the presence of specific risk factors guided by a hierarchy of explorations to reduce the time to specific management.
References
- Akhil Das, Patricia Lewandoski, Dean Laganosky, John Walton, Patrick Shenot, Ureteroarterial fistula: A review of the literature.
- List A, Collins J, MacCormick M. Massive hemorrhage from an arterioureteral fistula associated with chronic renal transplant failure. J Urol, 1990; 144: 1229–1230.
- Dervanian P, Castaigne D, Travagli JP, Chapelier A, Tabet G, Parquin F, et al. Arterioureteral fistula after extended resection of pelvic tumors: report of three cases and review of the literature. Ann Vasc Surg, 1992; 6(4): 362-369.
- Bergqvist D, Parsson H, Sherif A. Arterio-ureteral fistula–a systematic review. Eur J Vasc Endovasc Surg, 2001; 22(3): 191-196.
- Dana A, Helenon O. Urinary tract imaging: conventional radiology and ultrasound. J Radiol, 2004; 85(2 Pt 2): 169-170.
- van den Bergh RC, Moll FL, de Vries JP, Yeung KK, Lock TM. Artério-urétéral fistula: 11 new cases of a wolf in sheep’s clothing. J Urol, 2008; 179(2): 578-581.
- van den Bergh RC, Moll FL, de Vries JP, Lock TM. Arterioureteral fistulas: unusual suspects-systematic review of 139 cases. Urology, 2009; 74(2): 251-255.
- Demailly M, Gastaud O, Hakami F, Petit J. About two cases of arterioureteral fistula. Prog Urol, 2001; 11: 528-533.
- van den Bergh RC, Moll FL, de Vries JP, Lock TM. Arterioureteral fistulas: unusual suspects – systematic review of 139 cases. Urology, 2009; 74: 251–255.
- Krambeck AE, DiMarco DS, Gettman MT, Segura JW. Ureteroiliac artery fistula: diagnosis and treatment algorithm. Urology, 2005; 66(5): 990-994
- Tselikas L, Pellerin O, Di Primio M, Ben Arfi M, Joskin J, Beyssen B, et al. Ureteroiliac fistula: modern endovascular management.
- Bergqvist D, Pa¨rsson H, Sherif A. Arterio-ureteral Fistula – a Systematic Review, Department of Surgical Sciences, 2 Section of Surgery & Section of Urology, University Hospital, Uppsala, Sweden.
- Bodak A, Levot E, Schut A, Vincent JP, Lagneau P. A case of arterioureteral fistula: a review of the literature. J Urol, 1990; 96: 55-59.
- Dalmas P, Haddad O, Jaquier A, Lechevallier E, André M, Bartoli JM, et al. Arterioureteral fistula: diagnostic and therapeutic approach. Prog Urol, 2001; 11: 1277-1281.
- Menasse F, Rossi D, Heckenroth H, Ayuso D, Albertini JN, Tournigand P. Ureter-arterial fistulas: a review of two cases and a review of the literature. Prog Urol, 1997; 7: 1007-1011.
- Quillin SP, Darcy MD, Picus D. Angiographic evaluation and therapy of ureteroarterial fistulas. Am J Radiol, 1994; 162: 873–878.
- Verduch M, Beuamud GA, Estorell MF, et al Postappendectomy arterio-ureteral fistula. Urol Act Esp, 1980; 4: 331–334.

