A Clinical Case of Mobitz Type II
Dhruv Patel1, Leobel Urquiaga Perez1, Rebecca Hargett2, Sultan S Ahmed2,*, Syed AA Rizvi2,* Prerana Upadhyaya3 and Syed M Imam4
1Ross University School of Medicine, Bridgetown, Barbados
2College of Biomedical Sciences, Larkin University, Miami, Florida, USA
3JAS Medical Management, Miramar, Florida, USA
4HCA Northside Hospital, USF Morsani College of Medicine, St Petersburg, Florida, USA
Received Date: 01/06/2023; Published Date: 29/09/2023
*Corresponding author: Syed AA Rizvi, MD, PhD, MPH, MBA, College of Biomedical Sciences, Larkin University, 18301 N Miami Ave, Miami, FL 33169, USA
Sultan S Ahmed, MD, College of Biomedical Sciences, Larkin University, 18301 N Miami Ave, Miami, FL 33169, USA
Abstract
A 56-year-old male presented to the clinic with intermittent dizziness, shortness of breath, and multiple syncopal-like episodes. He has been having these symptoms for the past 5 years. He had previously gone to the hospital on multiple occasions due to the syncopal episodes. In the hospital, neurological pathologies were ruled out with a negative Computed Tomography (CT) scan of the brain. An Electrocardiography (ECG) was done in the Emergency Department (ED) and based on the interpretations from the emergency physician, was unable to detect any abnormalities. He was not in any acute distress or displayed any symptoms. Patient was discharged and advised to follow up with the primary care provider. Upon follow up, the patient continued to have his symptoms, so an ECG was conducted in the office that revealed a 2:1 Mobitz II AV block.
Introduction
Mobitz type II AV blocks are often missed on ECGs which have resulted in multiple incorrect management for patients. It is important to understand how Mobitz type II AV block can be differentiated from other AV blocks and how attentive physicians should be when a patient comes in with the signs and symptoms that may represent a Mobitz type II [-2].
There are three known degrees of AV blocks which can be differentiated through the observation of an ECG. In first-degree AV block, impulses reach the ventricle but are always delayed, resulting in a prolongation of the PR interval (>200ms). These impulses are not interrupted so complete atrial conduction is produced. In second-degree AV block, some AV conduction is taking place, but two or more consecutive P impulses are blocked. Therefore, atrial to ventricular conduction is intermittent with patterns of 2:1. 3:2, 4:3, 5:4, etc. In third-degree there are no impulses from the atria reaching the ventricles. This indicates that conduction is completely blocked, and P waves are not conducted [3].
Second degree can be further divided into Mobitz type I or Mobitz type II. Mobitz type I is characterized by an increase in the delay of the signal from the atria to the ventricle whenever there is a contraction until there is no signal reaching to the ventricles from the atria. Mobitz type II is a second-degree AV block that is a disturbance in the conduction pathway in the myocardium anywhere from below the AV node to the branches of the Bundle of His. In a second-degree AV block, the impulses from the atria to the ventricles are intermittent. The second-degree AV block can further be classified into Mobitz II in which there is no delay in the electrical conductance between the atria and ventricle, but the impulse from the AV node is not always conducted. The prevalence of Mobitz type I and II have been only conducted only in small scale studies which found no association with age, gender, or race [4]. Incidence is greater in those with heart failure, about 1 in 30 will develop Mobitz type II [5]. Common symptomatology of Mobitz type II include syncope, dizziness, fatigue, chest pain, and dyspnea. Syncope is a common symptom that is seen in Mobitz type II occurring in 63% of people with a block at the distal Bundle of His and 29% of people with a block at the proximal of Bundle of His [6]. Due to the asynchronization between the atria and ventricles, the atrial pressure increases resulting in the release of Atrial Natriuretic Peptide (ANP) which leads to reflex systemic hypotension and resulting in hypoperfusion to the brain.
Case Presentation
The patient has a medical history of Coronary Artery Disease (CAD), hypertension, and diabetes mellitus type 2. He denied a history of tobacco use, alcohol, or any substance abuse. His current medications are Metformin, Carvedilol, Aspirin, and Atorvastatin. His blood pressure was 142/84 mmHg, his respiratory rate was 17 breaths/min, and his pulse rate was 38 beats/min with a regularly-irregular rhythm. His height was 167.6 cm and his weight was 60.8 kg with a body mass index of 21.6 kg/m2. He had bradycardia and no murmurs, gallops, or rubs that were detected. The apical impulse was felt at the 5th intercostal space midclavicular with a normal character, and S1 and S2 were normal. The patient had no carotid artery bruit and orthostatic blood pressure was normal. The neurological examination findings were all normal. Upon observation, the patient had scalene muscles that were prominent bilaterally.
Laboratory test results were the following: total cholesterol, 94 mg/dL; high-density lipoprotein cholesterol, 45 mg/dL; low-density lipoprotein cholesterol, 33 mg/dL; triglycerides, 84 mg/dL; glucose, 1224 mg/dL; glycated hemoglobin, 7.2%; thyroid stimulating hormone, 1.12 mIU/L; sodium,141 mEq/L; potassium, 4.6 mEq/L; chloride, 105 mEq/L; calcium, 9.7 mg/dL; carbon dioxide, 29 mmol/L; blood urea nitrogen, 9 mg/dL; creatinine 0.78 mg/dL; hemoglobin 14.3 g/dL, and hematocrit, 41.6%.
ECG results showed a normal PR interval (120ms-200ms) with wide QRS complexes (>120 ms). At every 2 p waves, a QRS complex was conducted showing a 2:1 AV block (Figure 1). The ECG showed bradycardia (38 beats/min) with a left axis deviation (RBBB with Left anterior fascicular block). The findings were consistent with second degree Mobitz type II AV block.
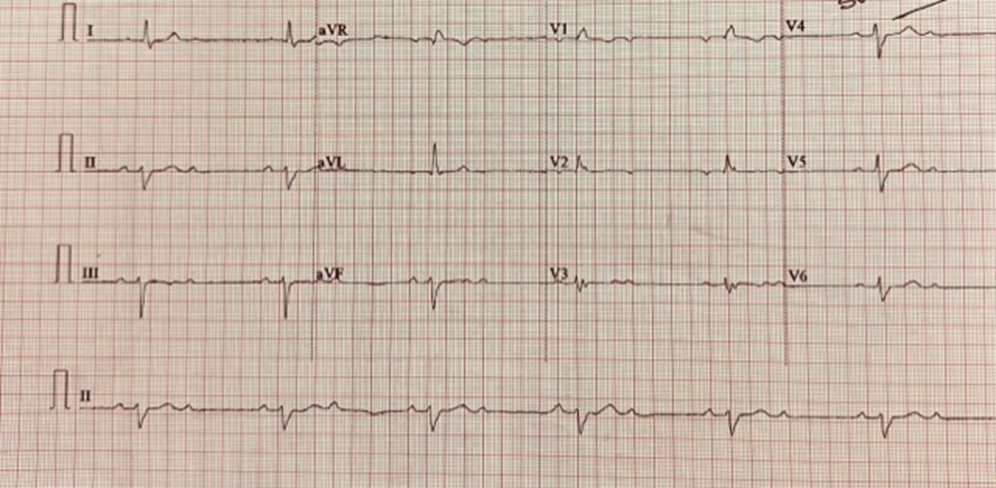
Figure 1: Patient with the initial ECG done at office. The ECG shows a 2:1 AV block seen in leads II, II, and avF.
Discussion
It is important to suspect the possibility of a heart condition based on symptoms of syncope, dizziness, fatigue, chest pain, or dyspnea. Physicians should be more attentive in reading ECGs when presented with patients having symptoms like syncope or lightheadedness as AV blocks could be easily missed. Based on evidence, in about 33% of ECG interpretations, some type of error was seen and in 11% has resulted in an incorrect management [7].
Detrimental effects such as collapsing anytime without any warnings can potentially be a result from missing Mobitz type II AV block. When looking at an ECG, it is important to identify whether the 2:1 AV block is due to Mobitz type I or Mobitz type II since the protocol for treatments are different. In Mobitz type I, the treatment is based on whether the patient presents with any symptoms, while Mobitz type II will require a pacemaker regardless. Since majority of the cases Mobitz type I is intranodal, the QRS complexes are narrow, but Mobitz type II is generally infranodal more commonly distal to the Bundle of His which would produce wider QRS [8]. It is important to note that identifying the site of the block based on the QRS complex may be helpful but is not always the case. Vagal maneuvers can be performed to decrease the sinus rhythm by allowing recovery time for the excitation of the Bundle of His to help identify the type of AV Block [9].
Mobitz type II AV block can be caused from a variety of reasons from pathologic to iatrogenic. Some of the more common pathologic causes include myocardial ischemia, cardiomyopathy, myocarditis, endocarditis with abscess formation, hyperkalemia, or hypervagotonia. Some of the iatrogenic causes include medication related to the AV node blocking, post-cardiac surgery, or post-catheter ablation [4].
The treatment is based on where the block is in the conduction between the atria and the ventricles. Any block below the AV node requires a pacemaker, whereas an intranodal block may not require a pacemaker due to a junctional rhythm taking over [10]. However, if the patient has symptomatic bradycardia with a second-degree AV block regardless of type or site of block, a permanent pacemaker is indicated according to the American Heart Association [11]. If a permanent pacemaker is not able to be placed immediately, a transcutaneous pacing can be placed in patients until a permanent pacemaker is obtained to reduce the complication of progressing into a third-degree AV block [12]. There are 3 types of permanent pacemakers- dual-chamber pacing, single-chamber pacing, and biventricular pacing. Based on current evidence, there is no superiority based on mortality of a specific permanent pacemaker for a type II Mobitz AV block [13]. However, if the patient progresses to have symptomatic bradycardia, a dual-chamber pacing is recommended based on the National Institute for Health and Care Excellence [14,15].
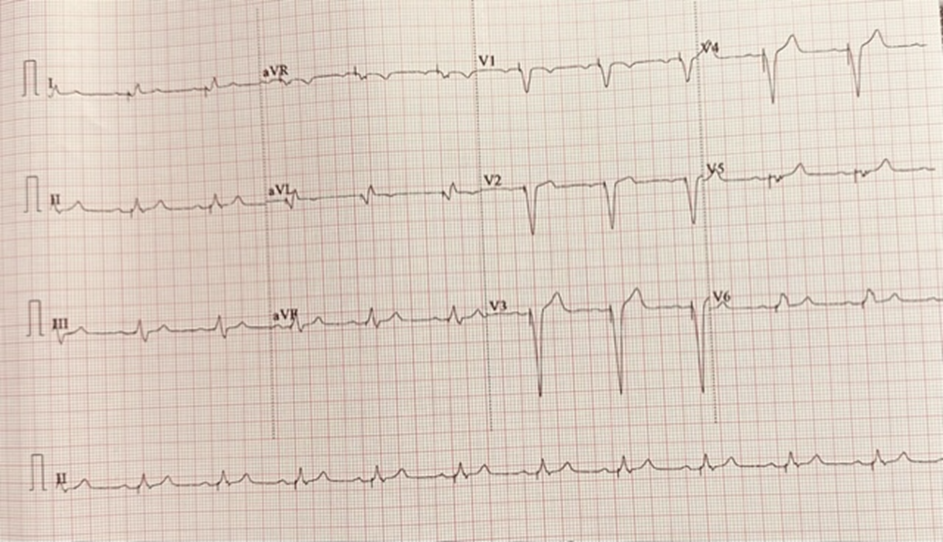
Figure 2: Patient after the pacemaker was placed. The ECG shows normal PR interval at all leads.
Our patient was experiencing multiple syncopal-like episodes with dizziness which warranted an ECG. The ECG showed a 2:1 Mobitz type II AV block which indicated the need for a permanent pacemaker. He was sent to the emergency department, where an electrophysiologist placed the pacemaker. The patient returned back to the office after 15 days for a follow up where an ECG was repeated. The ECG in the office showed a normal sinus rhythm with a normal axis. The AV block was no longer seen as each P wave was followed by a QRS complex (Figure 2). The patient reported that he no longer has any syncopal-like episodes, dizziness, or any shortness of breath.
Disclosures: The authors report no relevant financial relationships.
References
- Barold SS. Problematic definitions of Mobitz type II second degree AV block: Historical aspects. J. Electrocardiol, 2023; 79: 122-123. doi.org/10.1016/j.jelectrocard.2023.03.086
- Jiménez-Díaz J, González-Ferrer JJ, Heredia GU, Moreno-Planas J. Mobitz type II second-degree atrioventricular block with narrow QRS and junctional extrasystoles: what is the mechanism? J Cardiovasc Electrophysiol, 2014; 25(4): 447-449. doi:10.1111/jce.12321
- Sauer WH. Etiology of atrioventricular block. In: Post T, ed. UpToDate., 2023.
- Mangi MA, Jones WM, Mansour MK, et al. Atrioventricular Block Second-Degree. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023.
- Heart block, 2023.
- Rosen KM, Dhingra RC, Loeb HS, Rahimtoola SH. Chronic heart block in adults. Clinical and electrophysiological observations. Arch Intern Med, 1973; 131(5): 663-672.
- Breen CJ, Kelly GP, Kernohan WG. ECG interpretation skill acquisition: A review of learning, teaching and assessment. J Electrocardiol, 2022; 73: 125-128. doi:10.1016/j.jelectrocard.2019.03.010
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society [published correction appears in J Am Coll Cardiol. 2019 Aug 20;74(7):1014-1016]. J Am Coll Cardiol, 2019; 74(7): 932-987. doi:10.1016/j.jacc.2018.10.043
- Niehues LJ, Klovenski V. Vagal Maneuver. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023.
- Kashou AH, Goyal A, Nguyen T, et al. Atrioventricular Block. [Updated 2023 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023.
- Gregoratos G, Cheitlin MD, Conill A, et al. ACC/AHA Guidelines for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices: Executive Summary--a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). Circulation, 1998; 97(13): 1325-1335. doi:10.1161/01.cir.97.13.1325.
- Doukky R, Bargout R, Kelly RF, Calvin JE. Using transcutaneous cardiac pacing to best advantage: How to ensure successful capture and avoid complications. J Crit Illn, 2003; 18(5): 219-225.
- Castelnuovo E, Stein K, Pitt M, et al. The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation. 2005. In: NIHR Health Technology Assessment programme: Executive Summaries. Southampton (UK): NIHR Journals Library; 2003.
- National Institute for Health and Care Excellence (NICE). Dual-Chamber Pacemakers for Symptomatic Bradycardia due to Sick Sinus Syndrome and/or Atrioventricular Block. London: NICE, 2005.
- Mbizvo GK, Derry C, Davenport R. Ictal asystole: a diagnostic and management conundrum. J R Coll Physicians Edinb, 2019; 49(2): 128-131. doi:10.4997/JRCPE.2019.209

