Acute Limb Ischemia in a Case of Lower Extremity Artery Ectasia with Multiple Aneurysms Treated by Stent-Faciliated Mechanical Thrombectomy
Cheng-De ChangChien1, Nai-Yu Chi1,2, Ching-Tang Chang1,2, Tzu-chieh Lin1,2, Ho-Ming Su1,2,3, Tsung-Hsien Lin1,2,3 and Po-Chao Hsu1,2,3,*
1Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Taiwan
2Division of Cardiology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Taiwan
3Department of Internal Medicine, Faculty of Medicine, School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
Received Date: 11/01/2023; Published Date: 06/02/2023
*Corresponding author: Po-Chao Hsu, Division of Cardiology, Department of Internal Medicine; Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung. 80708, Taiwan, ROC
Abstract
Acute Limb Ischemia (ALI) is an unstable and emergency situation of peripheral artery disease (PAD). Timely recognition of arterial occlusion is crucial to successful treatment. Endovascular intervention for PAD has been robustly developed in recent years and plays an important role in ALI treatment. Catheter-directed thrombolysis and Pharmaco Mechanical Thrombectomy (PMT) are two major treatment strategies of endovascular therapy for ALI. Although PMT gradually becomes a useful and convenient method for physicians to treat ALI, it is still difficult to treat the patients with large thrombus burden in ectatic arteries and aneurysms. Herein we report a rare case of ALI with lower extremity artery ectasia and multiple aneurysms who initial failed to treat by PMT and finally treated by stent-faciliated mechanical thrombectomy. This rare case reminds physicians that assisted stent implantation may decrease the thrombus burden and let PMT more effective to treat the crisis of ALI.
Introduction
Acute Limb Ischemia (ALI) is an unstable and emergency situation of Peripheral Artery Disease (PAD). The definition of ALI is severe hypoperfusion of the limb less than 2 weeks characterized by the features: pain, pallor, pulselessness, poikilothermia, paresthesias, and paralysis. ALI is one of the most treatable and potentially devastating presentations of PAD. Timely recognition of arterial occlusion is crucial to successful treatment. Endovascular intervention for PAD has been robustly developed in recent years. It also plays an important role in ALI management. There are two major treatment strategies of endovascular therapy for ALI. One is catheter-directed thrombolysis (CDT). Another is Pharmaco Mechanical Thrombectomy (PMT) including several different devices such as rotarex, angiojet, Indigo, and so on. Although PMT gradually becomes a useful and convenient method for physicians to treat ALI, it is still difficult to treat the patients with large thrombus burden in ectatic arteries and aneurysms. Herein we report a case of ALI with lower extremity artery ectasia and multiple aneurysms who initial failed to treat by PMT and finally treated by stent-faciliated mechanical thrombectomy.
Case Presentation
A 71-year-old male presented to the Emergency Department (ED) due to left foot suddenly cyanosis with progressive painful and cold sensation. At ED, vital sign was relative stable, emergent lower extremities Computed Tomography (CT) was arranged for ALI evaluation and results showed total occlusion at left middle Superficial Femoral Artery (SFA), popliteal artery and Below-The-Knee (BTK) arteries without apparent collateral circulation. In addition, ectatic arteries and several huge aneurysms were also noted over the artery system of lower extremities. Because ALI was confirmed by the CT imaging, emergent endovascular intervention team was consulted for ALI treatment.
After explaining to the patient and family, they agreed to use mechanical thrombectomy device (Rotarex) for massive thrombus removal. Initial angiography was shown in Figure 1A-1C. Unfortunately, due to large thrombus burden and suspect some chronic lesions over the femoral-popliteal area, we tried several wires (0.014, 0.018 and 0.035 wire) and still failed to enter into BTK arteries. We decided to use rotarex thrombectomy to remove the thrombus over distal femoral artery first. However, rotarex device became soon occluded in the catheter lumen due to large amount thrombus. But accidentally, V18 wire can successfully enter into BTK arteries after initial rotarex device use. After that, we had to frequently extract the device to clean the catheter lumen in order to avoid dysfunction or breaking the device. After several times of rotarex thrombectomy (Figure 1D), there are still lots thrombus burden in the distal femoral artery and still no distal blood flow regained. Therefore, we tried to stent the distal SFA to popliteal artery with a bare metal stent and supera stent. After post-dilating the in-stent area and treat the BTK arteries by angioplasty, we can regain antegrade but slow blood flow from distal SFA to popliteal artery. We further use Rotarex device to perform mechanical thrombectomy for several times, and blood flow became better to BTK arteries despite still poor distal runoff over dorsal-plantal area. Then we inserted fountain catheter into popliteal artery for further CDT. After 2 days CDT treatment, follow-up angiography showed improved blood flow from SFA to distal foot via posterior tibial artery. We used edoxaban (60mg) plus clopidogrel as dual-therapy after the procedure to improve the residual thrombus in the left foot. The patient was finally discharged uneventfully without major or minor limb amputation.
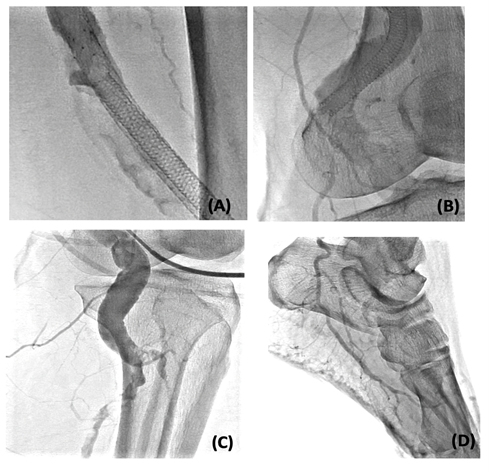
Figure 1: Initial angiography of left leg and usage of Rotarex device.
A: Left iliac artery aneurysm
B: Distal superficial artery showed acute thrombosis
C: Contrast staining revealed popliteal artery aneurysm
D: Stent-faciliated rotarex thrombectomy
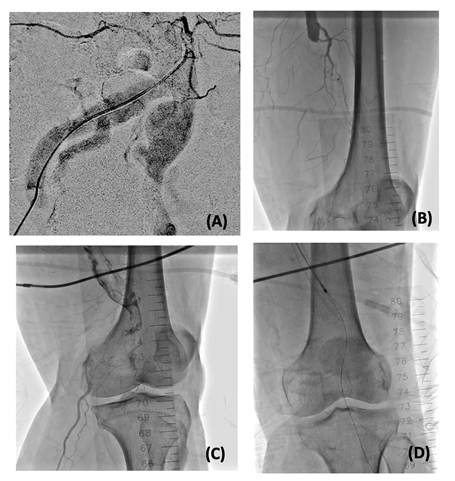
Figure 2: Post stent-facilated rotarex thrombectomy and further catheter-directed thrombolysis.
A: Distal superficial femoral artery to popliteal artery with ectasia noted after CDT treatment
B: Popliteal artery ectasia
C: Popliteal artery aneurysm formation
D: Blood flow can down to distal foot via posterior tibial artery.
Discussion
Aneurysms over lower extremity artery system, such as iliac, femoral, or popliteal aneurysm are reported to be highly associated with ALI. Up to 50% of all Popliteal Artery Aneurysms (PAA) present with ALI. ALI due to PAA is a ferocious problem for 20% to 60% incidence of limb loss and up to 12% mortality reported in the literature in the last three decades [1].
For PAA, surgical thrombectomy and additional femoro-popliteal or femorocrural bypass grafting were the treatments of choice [2]. However, intra-arterial CDT was successfully attempted to improve arterial runoff before surgical revascularization to increase patency rates of peripheral bypass surgery [3]. During recent years, complete endovascular treatment (thrombolysis, thrombectomy and stent grafting) has become an alternative to open surgery. Endovascular approaches are being used with increasing frequency as techniques and materials improve and because of their lower invasivity [4-6]. CDT and PMT are the current two major treatment strategy of endovascular therapy in ALI. Although PMT in combination with CDT treatment is a useful strategy to treat ALI, there are still several difficult situations such as ectatic peripheral arteries or huge aneurysms formation, which may cause PMT not effective or unsuccessful. Our patient was a case of ALI with not only ectatic peripheral arteries but also several huge aneurysms including iliac, femoral, and popliteal aneurysms. PMT only in our case was not so effective and cannot regain the adequate blood flow to distal foot. In this situation, surgical thrombectomy may be an alternative choice to treat the patient. However, we met some problems while manipulating wires to cross the popliteal artery which might suggest the patient had some chronic stenosis or occlusion over this area. Surgical thrombectomy may also not suitable for the patient with acute on chronic occlusions. Stenting is a useful technique which can help physicians to reduce the thrombus burden and let PMT have higher successful rate in this situation. According to the literature, there are rare cases discussing about the stent-facilitated PMT strategy for ALI patients with multiple aneurysm formation. Our case should be one of the limited cases successfully treated by the stent-facilitated PMT strategy in the patients with ecstatic peripheral arteries and multiple aneurysms.
Conclusion
For the ALI patients with ectatic peripheral arteries and multiple aneurysms, PMT may sometimes failed to recanalize the acute thrombosis due to large thrombus burden. By assisted stent implantation, we may decrease the thrombus burden and let PMT more effective to treat the crisis of ALI.
References
- Robinson WP, Belkin M. Acute limb ischemia due to popliteal artery aneurysm: a continuing surgical challenge. Semin Vasc Surg, 2009; 22(1): 17-24.
- Kropman RH, Schrijver AM, Kelder JC, Moll FL, de Vries JP. Clinical outcome of acute leg ischaemia due to thrombosed popliteal artery aneurysm: systematic review of 895 cases. Eur J Vasc Endovasc Surg, 2010; 39(4): 452-457.
- Schwarz W, Berkowitz H, Taormina V, Gatti J. The preoperative use of intraarterial thrombolysis for a thrombosed popliteal artery aneurysm. J Cardiovasc Surg (Torino). 1984; 25(5): 465-468.
- Bandeira RN, Cacione DG, Bandeira FCV, Pelissoni AS, Leite CON, Nakano LCU. Tratamento endovascular versus tratamento aberto de aneurisma de artéria poplítea: artigo de revisão. J Vasc Bras, 2018; 17(1): 34-41.
- Tayfur K, Bademci MŞ. Popliteal artery aneurysms treatments: early midterm results of the use of endovascular stent grafts. Turk J Med Sci, 2021; 51(3): 1106-1114.
- Saunders JH, Abisi S, Altaf N, Yong Y, MacSweeney ST, Whittaker S, et al. Long-term outcome of endovascular repair of popliteal artery aneurysm presents a credible alternative to open surgery. Cardiovasc Intervent Radiol, 2014; 37(4): 914-919.

